Volume 18 Number 1
Kidney Health for All: Bridging the gap in kidney health education and literacy
Robyn G Langham, Kamyar Kalantar-Zadeh, Ann Bonner, Alessandro Balducci, Li-Li Hsiao,
Latha A Kumaraswami, Paul Laffin, Vassilios Liakopoulos, Gamal Saadi, Ekamol Tantisattamo, Ifeoma Ulasi and Siu-Fai Lui
Keywords Health literacy, health policy, educational gap, kidney health, social media
For referencing Langham RG et al. Kidney Health for All: Bridging the gap in kidney health education and literacy. Renal Society of Australasia Journal 2022; 18(1):4-8
DOI
https://doi.org/10.33235/rsaj.18.1.4-8
Submitted 11 February 2022
Accepted 17 February 2022
Abstract
The high burden of chronic kidney disease (CKD), global disparities in kidney care, and poor outcomes of kidney failure bring a concomitant growing burden to persons affected, their families and carers, and the community at large. Health literacy (HL) is the degree to which persons and organisations have – or equitably enable individuals to have – the ability to find, understand and use information and services to make informed health-related decisions and actions for themselves and others. Rather than viewing HL as a patient deficit, improving HL largely rests with healthcare providers communicating and educating effectively in co-designed partnership with those with CKD. For kidney policy makers, HL provides the imperative to shift organisations to a culture that places the person at the centre of healthcare. The growing capability of and access to technology provides new opportunities to enhance education and awareness of CKD for all stakeholders. Advances in telecommunication, including social media platforms, can be leveraged to enhance persons’ and providers’ education; World Kidney Day declares 2022 as the year of Kidney Health for All to promote global teamwork in advancing strategies in bridging the gap in kidney health education and literacy. Kidney organisations should work toward shifting the patient-deficit HL narrative to that of being the responsibility of healthcare providers and health policy makers. By engaging in and supporting kidney health-centred policy making, community health planning and HL approaches for all, the kidney communities strive to prevent kidney diseases and enable living well with CKD.
Introduction
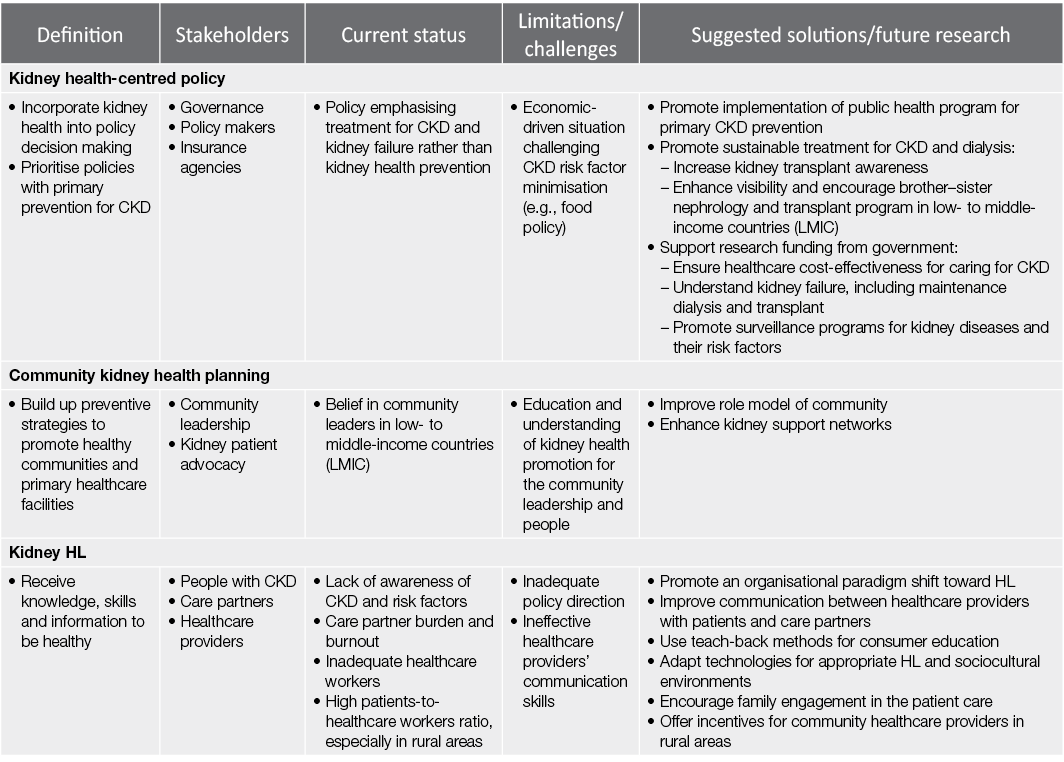
The challenging issue of bridging the well-identified gap in the health literacy (HL) of chronic kidney disease (CKD), from both an individual and a global perspective, is the theme for World Kidney Day 2022. HL, simply put, is the degree to which persons and organisations have – or equitably enable individuals to have – the ability to find, understand and use information and services to inform health-related decisions and actions for themselves and others (CDC, 2022). Not only is there is growing recognition of the role that HL has in determining outcomes for persons affected by CKD and the community in general, but there is an emergent imperative for policy makers worldwide to be informed and cognisant of opportunities and measurable outcomes that can be achieved through kidney-specific preventative strategies. Promoted in health policy for around a decade, current approaches that increase partnerships between health-centred policy, community health planning and kidney HL (Dinh et al., 2021) need to be shifted forward (Table 1).
Table 1. Summary of the characteristics of kidney health promotion, involving kidney health-centred policy, community kidney health planning and kidney HL, and proposed future directions
The global community of people with CKD
Most in the community do not even know what their kidneys do or where their kidneys are, amplifying the challenge for those afflicted by CKD. Effective healthcare provider communication is critical in supporting individuals in not only understanding their condition but in what to do, in making decisions and taking action. Optimal HL includes not only the functional but also the cognitive and social skills needed to gain access to, understand and use information to manage health conditions. HL is also contextual in that, as health needs change, so too does the level of understanding required and the ability to problem solve change. This is particularly so with CKD progression as health changes and treatments become increasingly complex, in turn making it more challenging for individuals to manage (Mathias-Shah et al., 2021).
While it has been recognised in some studies that low HL abilities in people with CKD have demonstrated an association with poor CKD knowledge, self-management behaviours and health-related quality of life, most CKD studies have measured only functional HL (Dinh et al., 2021). Because of this, the evidence that low HL increases healthcare utilisation and mortality (Taylor et al., 2018) and reduces access to transplantation (Taylor et al., 2019) is weak. There is a need for studies that assess HL using appropriate multidimensional patient-reported measures such as the World Health Organization (WHO) recommended Health Literacy Questionnaire rather than tools measuring only functional HL (Dobson et al., 2015).
HL is considered an important bridge between lower socio-economic status and other social determinants of health (Sørensen et al., 2012). This is, however, not a feature that can be measured by the gross domestic product (GDP) of a county; the effects of low HL on the extent of CKD in the community is recognised as a global phenomenon regardless of GDP. The lack of awareness of risk factors of kidney disease, even in those with high HL, is testament to the difficulties in understanding this disease. The United States, for instance, recommends that a “universal precautions” approach be undertaken toward improving HL (Brega, 2015). Imperatives around HL are now recognised as indicators for the quality of local and national healthcare systems and healthcare professionals within it (Nutbeam & Lloyd, 2021).
So, what does the perfect HL program look like for people with CKD? In several high-income countries there are national HL action plans with the emphasis shifted to policy directives, organisational culture and healthcare providers (ACSQHC, 2014), some with compulsory HL accreditation standards ensuring healthcare providers are cognisant of individual HL requirements. Despite the increasing array of web-based programs that provide detailed information and self-care training opportunities, there is substantial evidence that improving healthcare provider communication skills are more likely to improve understanding of health problems and abilities to adhere to complex treatment regimens (Visscher et al., 2018).
Access to information that is authentic and tailored specifically to the needs of the individual and the community is the aim, specifically the provision of culturally appropriate knowledge. In developing an approach to improving HL, incorporating local consumers in a co-design approach will ensure outcomes that are more appropriate to need in different regions of the world. This applies especially to communities that are smaller, with less access to electronic communication and healthcare services, where the level of HL is shared across the community and where what affects the individual also affects all the community.
HL research is still at an early stage (Boonstra et al., 2020). The best evidence supports the provision of targeted programs aimed at improving communication capabilities of healthcare professionals. Indeed, programs that address the lack of culturally safe, person-centred and holistic care, along with improving the communication skills of health professionals, are crucial for those with CKD (Synnot et al., 2018).
The global kidney community of policy and advocacy
HL is not only an identified gap between individuals and their healthcare providers, but also central in advocacy with health policy makers (Sørensen et al., 2012). Policy and advocacy are well recognised tools that can bring about change and paradigm shift at jurisdictional level, in turn improving community health. At the centre of advocating for policy change to better address health outcomes is an exercise in improving the HL of the policy makers. Good policy development requires good understanding of the problem at hand. For the key stakeholder, for example the kidney community, who believes that a problem exists which should be tackled through governmental action, there is an increasing recognition of the importance of formulating succinct, meaningful and authentic information to present to government for action, akin to approaches for improving HL for those with CKD.
Having said that, the development and communication of this message, designed to bridge the gap in knowledge of relevant jurisdictions, is only part of the process of policy development. An awareness of the policy process is important to clinicians who are aiming to advocate for effective change in prevention or improvement of outcomes in the CKD community. Authentic information that is meaningful to the government is critical. The policy development process can be stratified into five stages (Young & Quinn, 2002) (Figure 1). The policy cycle constitutes an expedient framework for evaluating the key components of the process. Importantly, of the five principles of advocacy that underline policy making (Young & Quinn, 2012), the most important for clinicians engaged in this space is that of commitment, persistence and patience.
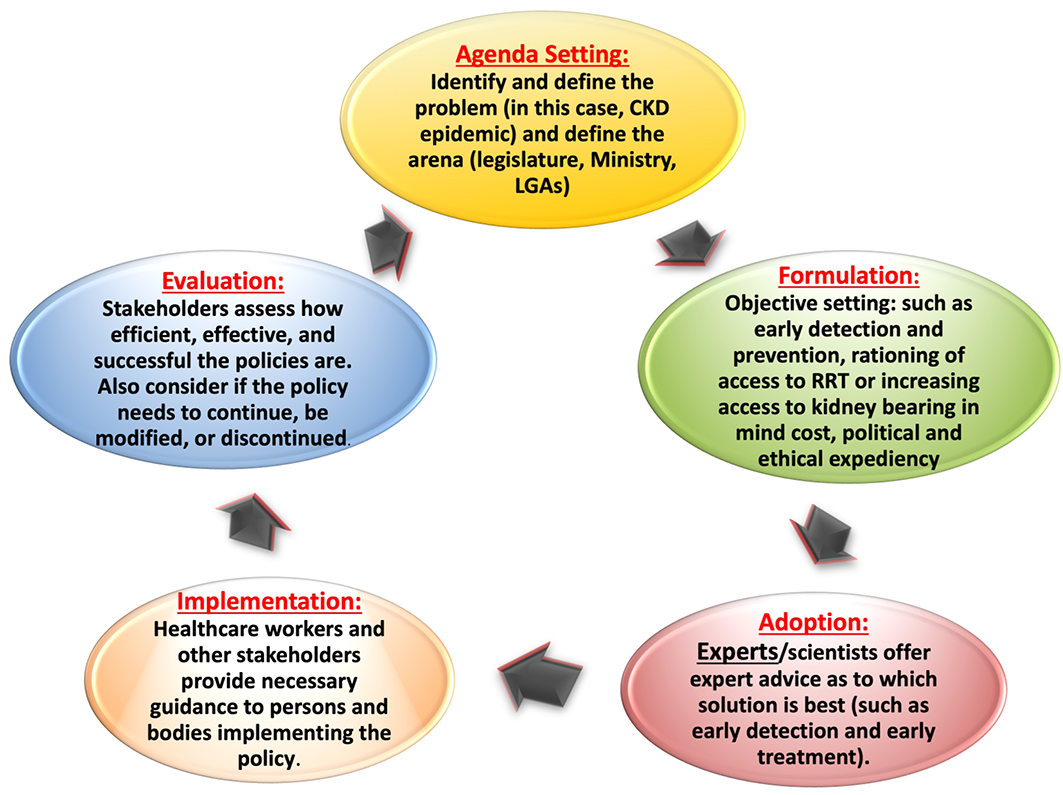
Figure 1. Policy cycle involving five stages of policy development
KRT, kidney replacement therapy; LGA, local government area
The Advocacy Planning Framework developed by Young and Quinn in 2002 (Young & Quinn, 2002) consists of three overlapping concepts that are key to planning any campaign:
- Way into the process: discusses the best approaches to translate ideas into the target policy debate and identify the appropriate audience to target.
- Messenger: talks about the image maker or face of the campaign and other support paraphernalia that are needed.
- Message and activities: explains what can be said to the target audiences that is engaging and convincing, and how best it can be communicated through appropriate tools.
As with improving HL, it is the communication of ideas to policy makers for adoption and implementation as policy that is key. There is much to be done with bridging this gap in understanding of the magnitude of community burden that results from CKD. Without good communication, many good ideas and solutions do not reach communities and countries. Again, aligned with the principles of developing resources for HL for those who suffer CKD, the approach to jurisdictions also needs to be nuanced according to the local need, aimed at the needs of the local community.
Advocacy requires galvanising momentum and support for the proposed policy or recommendation. The process is understandably slow as it involves discussions and negotiations for paradigms, attitudes and positions to shift, and multiple factors must be considered.
Approaches to choose from include (Start & Hovland, 2004; Young & Quinn, 2012):
- Advising: provides new evidence-based proposals to assist in decision-making.
- Activism: involves petitions, public demonstrations, posters, fliers and leaflet dissemination often used by organisations to promote a certain value set.
- Media campaign: having public pressure on decision makers helps in achieving results.
- Lobbying: entails face-to-face meetings with decision makers; this is often used by business organisations to achieve their purpose.
In this lies the importance of effective and successful advocacy by policy makers, healthcare professionals, communities and key change makers in society. World Kidney Day has gained trust by delivering relevant and authentic messaging and supporting leaders in local engagement, and is celebrated by both kidney care professionals and those with CKD and their caregivers all over the world. To achieve this goal, an implementation framework of sustainable success requires creativity, collaboration and communication. Utilising different social media platforms (Table 2) is an option to connect patients, family and healthcare professionals and provide kidney education (Figure 2).
Table 2. Social media platforms that are more frequently used for kidney education and advocacy
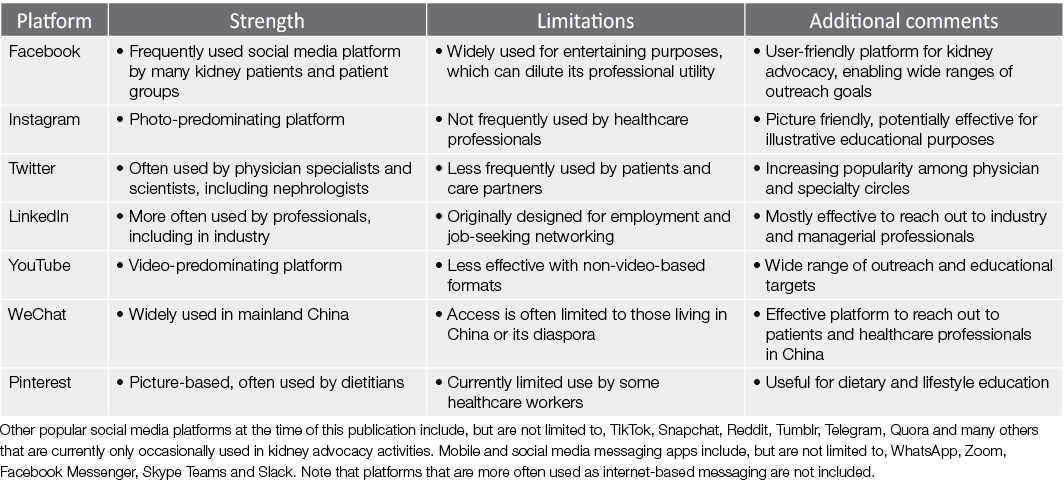
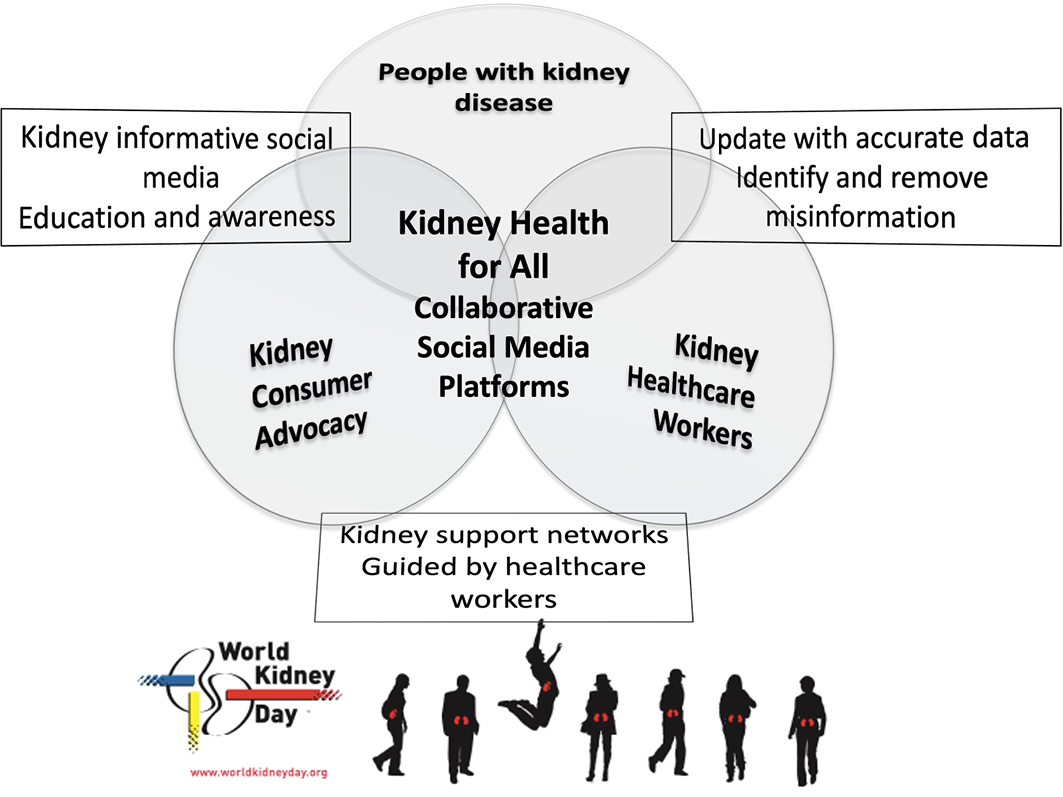
Figure 2. Schematic representation of consumer and healthcare professionals’ collaborative advocacy using social media platforms with the goal of Kidney Health for All.
The ongoing challenge for the International Society of Nephrology and International Federation of Kidney Foundations – World Kidney Alliance, through the Joint Steering Committee of World Kidney Day, is to operationalise the policy making process at the local, national and international levels in order to inform or guide decision making. This may be via increasing engagement of global organisations like WHO, the United Nations, or through regional governments in low-resource settings. There is a clear need for ongoing renewal of strategies in order to increase efforts at closing the gap in kidney HL, ultimately empowering those affected with CKD and their families, giving them a voice to be heard.
This article is being published in Kidney International and is being reprinted concurrently in several journals. The articles cover identical concepts and wording, but vary in minor stylistic and spelling changes, detail, and length of manuscript in keeping with each journal’s style. Any of these versions may be used in citing this article.
Note that all authors contributed equally to the conception, preparation and editing of the manuscript.
Copyright ©2022, World Kidney Day Steering Committee. Published by Elsevier Inc., on behalf of the International Society of Nephrology. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Conflict of interest
KK-Z reports honoraria from Abbott, Abbvie, ACI Clinical, Akebia, Alexion, Amgen, Ardelyx, AstraZeneca, Aveo, BBraun, Cara Therapeutics, Chugai, Cytokinetics, Daiichi, DaVita, Fresenius, Genentech, Haymarket Media, Hospira, Kabi, Keryx, Kissei, Novartis, Pfizer, Regulus, Relypsa, Resverlogix, Dr Schaer, Sandoz, Sanofi, Shire, Vifor, UpToDate and ZS-Pharma. VL reports non-financial support from Genesis Pharma. GS reports personal fees from Multicare, Novartis, Sandoz and AstraZeneca. ET reports non-financial support from Natera. All the other authors declared no competing interests.
Author(s)
Robyn G Langham† MBBS, PhD
St. Vincent’s Hospital, Department of Medicine, University of Melbourne, Melbourne, VIC, Australia
Kamyar Kalantar-Zadeh† MD, MPH, PhD
Division of Nephrology, Hypertension and Kidney Transplantation, Department of Medicine, University of California Irvine, Orange, California, USA
Ann Bonner RN, PhD
School of Nursing and Midwifery, Griffith University, Southport, QLD, Australia
Alessandro Balducci† MD
Italian Kidney Foundation, Rome, Italy
Li-Li Hsiao† MD, PhD
Brigham and Women’s Hospital, Renal Division, Department of Medicine, Boston, Massachusetts, USA
Latha A. Kumaraswami† BA
Tamilnad Kidney Research (TANKER) Foundation, The International Federation of Kidney Foundations-World Kidney Alliance (IFKF-WKA), Chennai, India
Paul Laffin† MS
International Society of Nephrology, Brussels, Belgium
Vassilios Liakopoulos† MD, PhD
Division of Nephrology and Hypertension, 1st Department of Internal Medicine, AHEPA Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece
Gamal Saadi† MD
Nephrology Unit, Department of Internal Medicine, Faculty of Medicine, Cairo University, Giza, Egypt
Ekamol Tantisattamo MD, MPH
Division of Nephrology, Hypertension and Kidney Transplantation, Department of Medicine, University of California Irvine, Orange, California, USA
Ifeoma Ulasi† MD
Renal Unit, Department of Medicine, College of Medicine, University of Nigeria, Ituku-Ozalla, Enugu, Nigeria
Siu-Fai Lui† MD
International Federation of Kidney Foundations – World Kidney Alliance, The Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong, China
†Note that these authors also form part of the World Kidney Day Joint Steering Committee
Correspondence to Robyn G Langham, University of Melbourne, Melbourne, VIC, Australia
Email rlangham@unimelb.edu.au
Reprints Ekamol Tantisattamo, Division of Nephrology, Hypertension and Kidney Transplantation, Department of Medicine, University of California Irvine School of Medicine, 101 The City Drive South, Orange, California 92868, USA
Email etantisa@hs.uci.edu
References
ACSQHC. (2014). Health literacy: Taking action to improve safety and quality. Sydney: ACSQHC. Retrieved from https://www.safetyandquality.gov.au/publications-and-resources/resource-library/health-literacy-taking-action-improve-safety-and-quality
Boonstra, M. D., Reijneveld, S.A., Foitzik, E. M., Westerhuis, R., Navis, G., & de Winter, A. F. (2020). How to tackle health literacy problems in chronic kidney disease patients? A systematic review to identify promising intervention targets and strategies. Nephrology, Dialysis, Transplantation, 36, 1207–1221.
Brega, A. G. (2015). AHRQ health literacy universal precautions toolkit (2nd ed). Denver, CO: Agency for Healthcare Research and Quality.
CDC. (2022). Healthy people 2030: What is health literacy? Retrieved from https://www.cdc.gov/healthliteracy/learn/index.html
Dinh, H. T. T., Nguyen, N. T., & Bonner, A. (2021). Healthcare systems and professionals are key to improving health literacy in chronic kidney disease. Journal of Renal Care, 48(1), 4–13.
Dobson, S., Good, S., & Osborne, R. (2015). Health literacy toolkit for low and middle-income countries: A series of information sheets to empower communities and strengthen health systems. New Delhi: World Health Organization.
Mathias-Shah, J., Ramsbotham, J., Seib, C., Muir, R., & Bonner, A. (2021). A scoping review of the role of health literacy in chronic kidney disease self-management. Journal of Renal Care, 47, 221–233.
Nutbeam, D., & Lloyd, J. E. (2021). Understanding and responding to health literacy as a social determinant of health. Annual Review of Public Health, 42, 159–173.
Sørensen, K., Van den Broucke, S., Fullam, J., et al. (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12, 80.
Start, D., & Hovland, I. (2004). Tools for policy impact: A handbook for researchers, research and policy in development programme. London, UK: Overseas Development Institute. Retrieved from https://www.ndi.org/sites/default/files/Tools-for-Policy-Impact-ENG.pdf
Synnot, A., Bragge, P., Lowe, D., et al. (2018). Research priorities in health communication and participation: International survey of consumers and other stakeholders. BMJ Open, 8(5), e019481.
Taylor, D. M., Bradley, J. A., Bradley, C., et al. (2019). Limited health literacy is associated with reduced access to kidney transplantation. Kidney International, 95(5), 1244–1252.
Taylor, D. M., Fraser, S., Dudley, C., et al. (2018). Health literacy and patient outcomes in chronic kidney disease: A systematic review. Nephrology, Dialysis, Transplantation, 33(9), 1545–1558.
Visscher, B. B., Steunenberg, B., Heijmans, M., et al. (2018). Evidence on the effectiveness of health literacy interventions in the EU: A systematic review. BMC Public Health, 18(1), 1414.
Young, E., & Quinn, L. (Eds.). (2002). Writing effective public policy papers: A guide to policy advisers in Central and Eastern Europe. Budapest, Hungary: Open Society Institute. Retrieved from https://www.icpolicyadvocacy.org/sites/icpa/files/downloads/writing_effective_public_policy_papers_young_quinn.pdf
Young, E., & Quinn, L. (Eds.). (2012). Making research evidence matter: A guide to policy advocacy in transition countries. Budapest, Hungary: Open Society Foundations. Retrieved from https://advocacyguide.icpolicyadvocacy.org/sites/icpa-book.local/files/Policy_Advocacy_Guidebook_2012.pdf
