Volume 19 Number 2
CARI guidelines: Culturally safe and clinical kidney care for First Nations Australians – A summary
Melissa Arnold-Ujvari, Liz Rix, Adela Yip, David J Tunnicliffe, Janet Kelly
Keywords cultural safety, clinical kidney care, First Nations, community voice
For referencing Arnold-Ujvari M et al. CARI guidelines: Culturally safe and clinical kidney care for First Nations Australians – A summary. Renal Society of Australasia Journal 2023; 19(2):93-99.
DOI
https://doi.org/10.33235/rsaj.19.2.93-99
Submitted 27 May 2023
Accepted 16 June 2023
Abstract
Context The ‘inaugural’ Caring for Australian and New Zealanders with Kidney Impairment (CARI) guidelines for First Nations Australians provide recommendations on caring for First Nations Peoples with chronic kidney disease (CKD). Informed by targeted national community consultations, the guidelines include the historical context, detailed advice on culturally safe kidney healthcare, screening and referral of CKD. Public awareness and education initiatives, self-management programs, and models of care are all reported on.
Objectives The CARI guidelines were developed in response to significant challenges and inequities experienced by First Nations Peoples over many years. Specific recommendations and suggestions aim to improve clinicians’ understanding of historical and contemporary factors contributing to the social and health inequities underpinning the over-representation of First Nations Peoples with CKD. These guidelines provide comprehensive support for health professionals in all service and care environments to better respond to the care needs of First Nations Peoples.
Key findings The CARI guidelines highlight the need to provide culturally safe clinical care and explicitly cite the need to address institutional racism and improve cultural safety training for all renal service providers. They specifically recognise the importance of kinship, and equitable access to transport and accommodation services. They also focus on keeping people on Country where possible, including increased nurse-supported and Aboriginal health practitioner-supported dialysis services.
Conclusion The CARI guidelines provide recommendations on how to improve clinical kidney care delivery for and with First Nations Peoples by ensuring more responsive models of care.
Brief statement
We use the term First Nations Peoples within this paper to reflect the diversity of Indigenous nations within Australia. First Nations Peoples in Australia have the longest living continuous culture in the world and are a strong and proud people who have and continue to survive and overcome ongoing colonisation impacts. There are now approximately 700,000 First Nations Peoples in Australia, accounting for 3% of the overall Australian population (Australian Institute of Health and Welfare (AIHW), 2015). Across Australia the treatment rate among First Nations Peoples for chronic kidney disease (CKD) is five times that among non-Indigenous Peoples, and is highest in remote areas (AIHW, 2020).
Background
The devastating impact of kidney disease on First Nations Peoples is a national emergency. The inaugural CARI guidelines for Australian First Nations Peoples with CKD were launched In October 2022 (Tunnicliffe et al., 2022). To our knowledge, these guidelines are the first national clinical guidelines to incorporate community voices and culture with clinical factors. The guidelines have been written to address the challenges and inequities unique to First Nations Peoples resulting from the negative impacts of colonisation and centuries of discrimination and inequities across all determinants of health. Until recently, identifying as a First Nations Australian was listed as a risk factor for the development of CKD. Until 2022 there were no CARI guidelines specifically addressing the treatment and care of First Nations Peoples.
A higher proportion of First Nations Australians live in rural and remote locations compared to non-Indigenous Australians (AIHW, 2021). Therefore, the management of CKD for First Nations Peoples often requires extensive travel and potential relocation for extended periods for kidney replacement therapy (KRT) (Cheikh Hassan et al., 2020). Relocation for treatment significantly impacts people with CKD and their families (Scholes-Robertson et al., 2022; Scholes-Robertson et al., 2020), including high out-of-pocket expenses and dislocation from family, community, culture and Country (Bateman et al., 2022; Kelly et al., 2022; Kidney Health Australia, 2020b; Mick-Ramsamy et al., 2019). For many First Nations Peoples, Country is a living entity; it is home, provides nourishment for body, mind and spirit and heart’s ease, and so to be dislocated from Country can have a detrimental health and wellbeing impact for First Nations Peoples (Rose, 1996) (Figure 1).

Figure 1. Flow & Thrive represents the landscape of living with a kidney condition, reproduced with written permission from CARI guidelines
These new guidelines were developed incorporating a targeted national community consultation process in multiple sites across Australia involving CKD patients, their families, Elders and community, as well as a formal literature review and expert opinion. These guidelines recognise and incorporate the underlying social, environmental and political impacts of historical and current-day inequities and injustices and the multiple levels of racism impacting First Nations Peoples.
Guideline methods
The guidelines have been developed using an adapted evidence to decision framework titled the Four Cs: community voice: clinical evidence; cultural considerations; and cost, capacity, equity and other considerations. The Four Cs emerged as an appropriate framework to underpin these guidelines following extensive discussion within the co-author group. It was agreed by all that the Four Cs provide relevance and recognition of the four domains that reflect the concerns and issues of community, clinicians, policy makers and funders. These are the first national guidelines to utilise this approach. The literature databases, MEDLINE, Embase and Aboriginal Health InfoNet were searched up to May 2022. The guideline recommendations summarised and discussed in this paper have been selected as being the most relevant to renal nursing practice. Access to the full text version of these guidelines can be found at: https://www.cariguidelines.org/first-nations-australian-guidelines/
Focus on community voices
Every which way you look at renal disease in Aboriginal people, the only solutions that will work in the long term are those that are Aboriginal led, culturally responsive, located in Aboriginal organisations and evaluated through an Aboriginal lens – Pat Turner CEO, National Aboriginal community-controlled health organisations (ACCHOs) National Indigenous Dialysis & Transplantation Conference (NIDTC), Alice Springs, 2019.
The guidelines were developed in partnership with First Nations Peoples. The three engagement strategies, published by (Duff et al., 2018), required:
- Engaging a panel of First Nations health clinicians.
- Targeting community engagements that were formally evaluated with locally based First Nations consumers and services.
- Consultation and feedback from Australian national peak organisations in First Nations Peoples health.
National community consultation in multiple sites across Australia drove the development of these guidelines. Kidney Health Australia led Yarning Kidneys, a series of community meetings across most states and territories which gathered the voices of patients, family members and carers. The 2019/20 bushfires and the Coronavirus pandemic limited the ability to travel to all states and jurisdictions; however, all states except Victoria and Tasmania contributed to these community meetings (Kidney Health Australia, 2020b). The Catching Some Air and AKction projects also conducted community consultations that also directly informed the guidelines (Mick-Ramsamy et al., 2019; Kelly et al., 2022).
Whilst each community raised specific recommendations and priorities relevant to their services and locations, a number of themes were common to all sites, including (Kidney Health Australia, 2020b):
- Involve and engage community in key activities.
- Promote prevention and education strategies for better health.
- Address the impact and burden of kidney failure treatment.
- Focus on support for patients and families.
- Support patients to access transplantation.
- Develop a sustainable and appropriate workforce.
- Improve cultural awareness within health services and staff.
- Promote strategies to minimise communication barriers.
- Advocate for better government support for kidney patients.
- Ensure completion and implementation of meaningful guidelines.
Feedback on the final draft of these guidelines from First Nations communities contributing to the Yarning Kidneys sessions was incorporated, along with targeted peer review by individual experts and peak organisations in First Nations kidney health. For further details on the methods underpinning these guidelines development, see the full guidelines online: https://www.cariguidelines.org/first-nations-australian-guidelines/
Guideline recommendations
Culturally safe and responsive kidney healthcare
The first recommendations of the guidelines strongly recommend all treatment and care for First Nations Peoples with CKD be culturally safe and responsive.
Inequity and institutional racism in healthcare
It is recommended that health services evaluate, monitor and act upon institutional racism within their systems. It is also recommended that First Nations Reference Groups advise kidney health services within Australia. There is a strong recommendation against inclusion of Indigenous status as a risk factor for CKD, in recognition that adverse social determinants of health rather than genetics impact progression of CKD.
Decolonising
An active process of decolonising services is strongly recommended. Decolonising strategies begin with all renal workforce exercising critical reflexivity. Other strategies for decolonising kidney services include:
- Enabling reciprocity.
- Transformative practice.
- Recognising and addressing power imbalance.
- Improved two-way communication and understanding between clinicians and patients/families.
- Increased access to culturally shaped care.
- Increasing self-determination and empowerment of patients.
There is a structured evaluation framework included in the Guidelines.
Cultural safety
The provision of culturally safe care is a lifelong shared commitment, with ongoing critical self-reflection for healthcare professionals a key component. Health services are responsible for delivering mandated cultural safety training that prioritises and targets unconscious bias, interpersonal and systemic racism. This training needs to be delivered in a non-threatening and supportive workplace and evaluated for effectiveness, and with opportunities to identify improvements to its implementation.
Figure 2 illustrates requirements and components of providing culturally safe and responsive kidney care. It is recommended that First Nations Peoples be part of the design and delivery of cultural safety training for healthcare staff. The inclusion of First Nations ways of knowing, being and doing is a strong recommendation. An example of this is the use of informal Yarning communication styles. It is recommended that all staff receive effective and responsive cultural safety training with continuous quality improvement strategies to actively address institutional racism.

Figure 2. Cultural safety for healthcare among First Nations Peoples
Family- and community-centred engagement and involvement in managing CKD
Health services are encouraged to better facilitate strategies that support family members to accompany First Nations Peoples when they relocate for management of their CKD. This includes social and psychological support needs. In recognition of strong kinship systems, family and community need to be included in decision making about dialysis and transplantation, as per patient preferences.
Transport and accommodation services for First Nations Peoples
There are strong recommendations that health services develop clear access pathways to ensure transport and accommodation requirements and options be made available to all patients and family members for all healthcare interactions.
First Nations kidney health workforce
The guidelines include a strong recommendation to ensure kidney services involve and support increased numbers of First Nations nurses, allied health and medical professionals, Aboriginal health practitioners and/or Aboriginal health liaison, patient preceptors/navigators and interpreters.
Further recommendations include that First Nations health practitioners receive formal education and training in CKD treatment options and management and that further financial investment is given, and that there is a strategic commitment to implement, evaluate and upscale a multi-disciplinary, community-based First Nations workforce.
Screening and referral of CKD
Early targeted screening is an important and cost-effective strategy to prevent the occurrence and progression of CKD and reduce cardiovascular disease (Kidney Health Australia, 2020a; Okpechi et al., 2021). Concerted efforts to decrease late referrals (less than 3 months between referral and the commencement of KRT) among First Nations Peoples have led to improvements in earlier engagement with specialist services (Australia and New Zealand Dialysis and Transplant Registry, 2021). However, the community consultations reiterated the need to prioritise early detection of CKD to improve management and outcomes for First Nations Peoples (Kidney Health Australia, 2020b; Mick-Ramsamy et al., 2019).
Screening and early detection programmes for CKD
The guidelines strongly recommend that CKD screening be undertaken for all First Nations Australians above 18 years of age as part of Medicare’s Aboriginal and Torres Strait Islander Peoples Health Assessment (Figure 3). The guidelines recommend that CKD screening programmes for First Nations Peoples be community-controlled, and co-designed with community using an integrative multi-disciplinary approach. A further recommendation is that First Nations Peoples receive age-appropriate health assessments (at least) annually. The guidelines suggest earlier referral to nephrology or supported services for earlier detection of CKD through a lower eGFR (≤45mL/min/1.73m2) threshold or sustained rapid decrease in kidney function (eGFR >10mL/min/1.73m2 per year). Figure 4 provides a referral matrix.
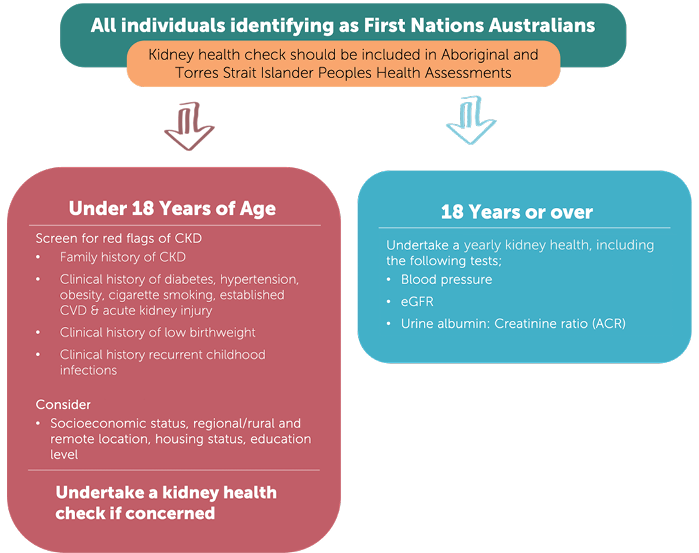
Figure 3. CKD screening matrix for First Nations Australians
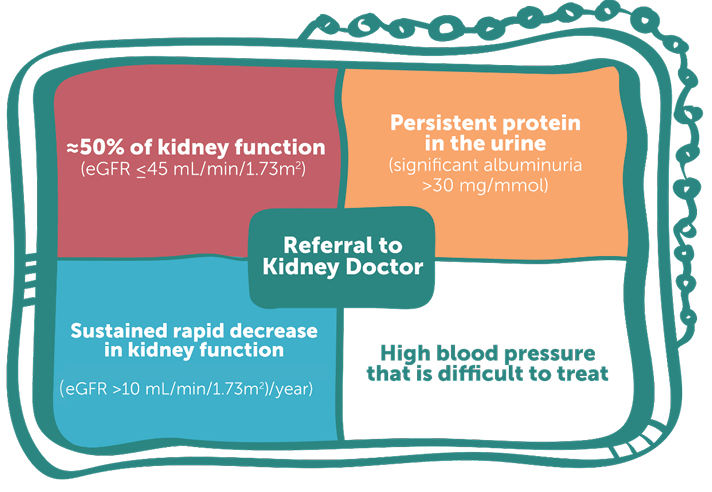
Figure 4. Referral matrix for First Nations Peoples
Public awareness, education and self-management
Public awareness
A strong recommendation is that all health promotion and public awareness campaigns be co-designed with local communities and include First Nations Peoples with lived experience of CKD. Co-design uses First Nations ways of knowing, being and doing and a range of culturally shaped resources/information, including the sharing of stories in community settings. The Sharing our Stories video promoting the guidelines for the launch is one example: https://www.cariguidelines.org/guidelines/management-of-chronic-kidney-disease-among-first-nations/
Education
The guidelines strongly recommend the development and use of community-led and co-designed educational resources that facilitate engagement and self-efficacy in the management of CKD. Strategies to achieve this include:
- Translation and interpretation of education programmes and resources to actively address language barriers.
- Use of a multi-factorial approach to the management of CKD for First Nations Peoples.
- Inclusion of a range of educational programs and techniques with Indigenous ways of knowing, being and doing, for example Yarning circles and storytelling.
- Involvement of Elders and First Nations Peoples with lived experience of CKD and family/community members supporting.
- Inclusion of art and music.
Self-management
A strong recommendation is made for self-management support to be available to First Nations Peoples across all stages of CKD, commencing upon initial engagement with healthcare services. This involves collaborative, ongoing self-management support utilising a whole-person approach that acknowledges the roles and responsibilities for both patients and healthcare professionals / services. Facilitating access to multi-disciplinary services such as exercise physiology, psychology, dietetics, audiology, podiatry, physiotherapy, optometry and oral health/dental services is recommended, according to individual needs.
Another important and strong recommendation is for adequate, sustainable and long-term funding models to support the co-design development, implementation and continuation of culturally safe First Nations-led self-management and behaviour change programs. There are further recommendations linked to culturally appropriate self-management supports (Figure 5).
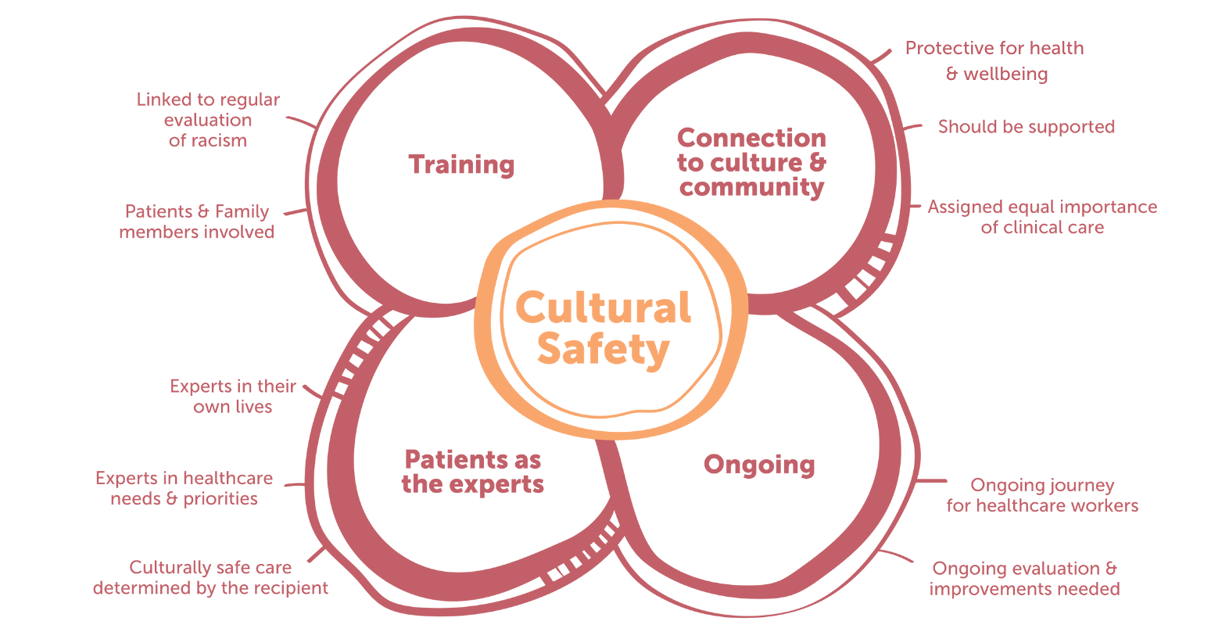
Figure 5. Self-management of CKD among First Nations Peoples
Models of care
There are comprehensive and strong recommendations for CKD models of care for pre-dialysis First Nations patients, progression to kidney failure and access to dialysis on Country, and consideration of further assessment of models of care for transplantation as new data emerges.
Pre-dialysis First Nations patients
An overarching and strong recommendation is for dedicated programmes specific for First Nations Peoples to identify those at risk to increase early detection, diagnosis and management of CKD. Co-design and governance by First Nations communities of programmes that are embedded into existing CKD programmes and services is also strongly recommended. Further, programmes that explicitly identify and address barriers to care, including (but not limited to) institutional racism, cultural and/or social barriers, geographical, transportation and/or other costs of healthcare to patients and families, are strongly recommended.
Progression to kidney failure and access to dialysis on Country
It is strongly recommended that health services work in partnership with ACCHOs to establish community-controlled models of care that address local needs and conditions, enabling First Nations Peoples to access nurse-supported and Aboriginal health practitioners-supported dialysis on Country, particularly in remote areas. Another strong recommendation is that kidney health services equitably provide dialysis services (for example, mobile dialysis) for patients where dialysis is not currently available. This service should include adequate transport, accommodation and workforce support to ensure equity.
The guidelines recommend: supported home- and community-based dialysis models to enable First Nations Peoples to access the benefits of dialysis closer to home; the utilisation of telehealth/video link models to augment face-to-face care for those living and receiving dialysis in regional and remote areas; and the availability of First Nations Peoples specific and co-designed programmes to address the social and emotional wellbeing of people undergoing KRT.
Models of care for transplantation
Kidney transplantation should be considered and discussed as a treatment option for all First Nations Peoples with CKD requiring KRT. There are ongoing studies researching the most appropriate and effective models of care for transplantation that will inform the future development of guideline recommendations. See the full guidelines for further recommendations: https://www.cariguidelines.org/guidelines/management-of-chronic-kidney-disease-among-first-nations/
Guideline overview
The inaugural CARI culturally safe and clinical kidney care guidelines for First Nations Peoples preface the need to address institutionalised racism and improve cultural safety, and these concepts are reiterated throughout. First Nations consumers, community and family voices and priorities reverberate throughout this document, making important steps toward truly working in partnership with consumers, addressing power imbalances, inequities and racism at all stages of kidney care from prevention to KRT. These guidelines strongly recommend the removal of Aboriginal and Torres Strait Islander status as a risk factor for CKD, in recognition that the impacts of colonisation and social, political, cultural and economic determinants of health affect CKD prevalence and outcomes rather than previous evidence of genetic predisposition. The guidelines incorporate formal western biomedical guideline development methods and also the lived experience and preferences of First Nations Peoples and communities with kidney disease. These guidelines include recommendations and ungraded statements directed towards improving nurses’ and health services understanding of the clinical and cultural care priorities of First Nations Peoples with the aim of improving equity within CKD care.
Guideline implementation discussion
These are the first known clinical practice guidelines to give equal weight to cultural, community, clinical and cost considerations. These guidelines highlight the need for co-design of all kidney services and models of care to enable culturally shaped care that responds to First Nations Peoples’ priorities. It is envisaged that other clinical guidelines developed for and with First Nations Peoples will follow. These guidelines aim to address long overdue challenges and barriers to accessing kidney treatment and care that is culturally safe and free from individual and institutional racism and bias. The guideline Working Group recognises that many of the guideline recommendations are relevant to the entire healthcare system, not just kidney health services. Additionally, the CARI guidelines recognise the need for further co-designed implementation of these guidelines to ensure their update and sustained implementation to achieve equitable health outcomes for First Nations Australians with CKD. The co-design process will require the ongoing engagement with First Nations communities across Australia as well as clinical staff, including renal nurses who are often the key driver of kidney care for First Nations Peoples. It is imperative that the knowledge shared by First Nations Peoples throughout the community consultation is valued and that reciprocity from all organisations and professional bodies is continued, thus ensuring improved care and outcomes for First Nations Australians with CKD.
Call to action
We encourage and urge everyone to become familiar with and spread the word about these new guidelines. They can only translate into culturally safer services, with improved accessibility and acceptability of kidney care for First Nations Peoples, if all renal nurses and healthcare disciplines access them. All renal healthcare workers must critically reflect upon their own individual practice and work collaboratively to improve care experiences and outcomes. Addressing institutional racism is a challenging and complex process, requiring the commitment and motivation of all. As renal nurses, we are ideally placed to play a significant role in co-designing culturally safer models of care with First Nations Peoples.
Guideline limitations
Throughout the systematic review process, the CARI Guidelines Working Group identified the lack of intervention studies to improve outcomes for First Nations Peoples. Additionally, most studies have limited reporting of the engagement, governance structures and prioritisation of work undertaken for effective research in partnership with First Nations Peoples (Tunnicliffe et al., 2022). The CARI Guidelines Working Group suggests that future research should be undertaken the right way according to the appropriate standards and the rights and priorities of First Nations communities.
Conclusion
The development of these guidelines was long overdue. If accessed and utilised appropriately within all kidney care service settings, these guidelines have the potential to increase cultural safety for all First Nations Peoples with CKD. First Nations Peoples need and deserve kidney care services with access to equitable treatment and care in culturally responsive and welcoming environments. These recommendations provide a framework for combining community voice, clinical evidence and cultural safety as well as cost, capacity, equity and resource considerations.
The voices I represent are so very tired of small steps without follow through. We have generations of grief and trauma sitting on our shoulders when we look to the future... we want fundamental changes happening NOW to allow us to live longer with our families. We want to not be continually faced by institutionalised and personal racism when we access treatment… here today, and for this point onwards, we all have an opportunity to decolonise our systems and processes together! – Kellie Owen, Kaurna, Narungga & Ngarrindjeri woman at the CARI guideline launch speech, 16 October 2022.
Acknowledgements
We wish to thank the CARI Guidelines Steering Committee – Rathika Krishnasamy, Vincent Lee, Jane Boag, Helen Coolican, Jonathan Craig, Vanessa Cullen, Min Jun, Kelly Lambert, Thu Nguyen, Carla Scuderi, Emily See, Martin Howell, Chandana Guha, Brydee Johnston, Nicole Scholes-Robertson and Andrea Viecelli. We also wish to thank Rochelle (Jungalungin) Pitt for her support of this paper.
Sources of support
These guidelines were developed in partnership with Kidney Health Australia. Kidney Health Australia received funding from the Honourable Ken Wyatt AM, MP, former Minister for Aged Care and Indigenous Health to undertake a process of national community consultations. These then informed the scope and content of the CARI guidelines. Kidney Health Australia also received funding from the Australian Government Department of Health. Caring for Australians with Renal Impairment were commissioned to produce guidelines on the management of CKD among First Nations Australians (Tunnicliffe et al., 2022).
Conflict of interest
All authors have no relevant conflict of interest according to the NHMRC Guidelines for Guidelines. Full details of all Working Group members conflicts of interests are available within the guidelines.
Author(s)
Melissa Arnold-Ujvari * RN MN PhD (candidate),
University of Adelaide, Adelaide, SA, Australia
Liz Rix RN BN PhD (Sydney),
University of Adelaide, Adelaide, SA, Australia
Adela Yip
Sydney School of Public Health, The University of Sydney, Sydney, NSW, Australia
Centre for Kidney Research, The Children’s Hospital at Westmead, Westmead, NSW, Australia.
David J Tunnicliffe PhD
Sydney School of Public Health, The University of Sydney, Sydney, NSW, Australia
Centre for Kidney Research, The Children’s Hospital at Westmead, Westmead, NSW, Australia.
Janet Kelly RN, MN, PhD
University of Adelaide, Adelaide, SA, Australia
Correspondence to Melissa Arnold-Ujvari, University of Adelaide – Adelaide Nursing School, North Terrace, Adelaide, SA 5005, Australia
Email melissa.arnold-ujvari@adelaide.edu.au
References
Australian Institute of Health and Welfare. (2015). The health and welfare of Australia’s Aboriginal and Torres Strait Islander Peoples. Canberra: AIHW.
Australian Institute of Health and Welfare. (2020). Profiles of Aboriginal and Torres Strait Islander People with kidney disease. Canberra: AIHW.
Australia and New Zealand Dialysis and Transplant Registry. (2021). 44th annual report. Retrieved from: https://www.anzdata.org.au
Bateman, S., Arnold-Chamney, M., Jesudason, S., Lester, R., McDonald, S., O’Donnell, K., ... Kelly, J. (2022). Real ways of working together: Co-creating meaningful Aboriginal community consultations to advance kidney care. Australian & New Zealand Journal of Public Health, 46(5), 614–621. https://doi.org/10.1111/1753-6405.13280
Cheikh Hassan, H. I., Chen, J. H., & Murali, K. (2020). Incidence and factors associated with geographical relocation in patients receiving renal replacement therapy. BMC Nephrology, 21(1), 249. https://doi.org/10.1186/s12882-020-01887-6
Duff, D., Jesudason, S., Howell, M., & Hughes, J. T. (2018). A partnership approach to engage Aboriginal and Torres Strait Islander Peoples with clinical guideline development for chronic kidney disease. Renal Society of Australasia Journal, 14(3), 84–88. https://search.informit.org/doi/10.3316/informit.018526878247237
Kelly, J., Stevenson, T., Arnold-Chamney, M., Bateman, S., Jesudason, S., McDonald, S., ... Williamson, I. (2022). Aboriginal patients driving kidney and healthcare improvements: Recommendations from South Australian community consultations. Australian & New Zealand Journal of Public Health, 46(5), 622–629. https://doi.org/10.1111/1753-6405.13279
Kidney Health Australia. (2020a). An update on chronic kidney disease in Aboriginal Australians. Retrieved from: www.kidney.org.au
Kidney Health Australia. (2020b). Executive summary ‘Yarning Kidneys’ community consultations. Retrieved from: https://kidney.org.au/uploads/resources/Executive-Summary-Yarning-Kidneys-Report.pdf
Okpechi, I. G., Caskey, F. J., Gaipov, A., Tannor, E. K., Hamonic, L. N., Ashuntantang, G., ... Jha, V. (2021). Assessing the impact of screening, early identification and intervention programmes for chronic kidney disease: Protocol for a scoping review. BMJ Open, 11(12):e053857. https://doi.org/10.1136/bmjopen-2021-053857. PMID:34916325; PMCID:PMC8679109.
Mick-Ramsamy, L., Kelly, J., Duff, D., Cass, A., Ross, L., Croker, D., ... Hughes, J. T. (2019). Catching some air. Asserting Aboriginal and Torres Strait Islander information rights in renal disease project – The final report. Retrieved from: https://www.menzies.edu.au/icms_docs/307210_Catching_Some_Air.pdf#:~:text=Recommended%20citation%20for%20online%20report,Disease%20Project%2D%20The%20Final%20Report.
Rose, D. B. (1996). Nourishing terrains: Australian Aboriginal views of landscape and wilderness. Canberra: Australian Heritage Commission. Retrieved from: https://www.ceosand.catholic.edu.au/catholicidentity/index.php/sustainability/sustainability-and-aboriginal-education/91-nourishing-terrains/file
Scholes-Robertson, N., Gutman, T., Dominello, A., Howell, M., Craig, J. C., Wong, G., & Jaure, A. (2022). Australian rural caregivers’ experiences in supporting patients with kidney failure to access dialysis and kidney transplantation: A qualitative study. American Journal of Kidney Diseases, 80(6), 773–782.e1. https://doi.org/10.1053/j.ajkd.2022.05.015
Scholes-Robertson, N. J., Howell, M., Gutman, T., Baumgart, A., Sinka, V., Tunnicliffe, D. J., ... Tong, A. (2020). Patients’ and caregivers’ perspectives on access to kidney replacement therapy in rural communities: Systematic review of qualitative studies. BMJ Open, 10(9), e037529. https://doi.org/10.1136/bmjopen-2020-037529
Tunnicliffe, D., Bateman, S., Arnold-Chamney, M., Dwyer K. M., Howell, M., Jesudason, S., ... Phoon, R. K. S. (2022). Recommendations for culturally safe and clinical kidney care for First Nations Australians. Retrieved from: https://www.cariguidelines.org/guidelines/management-of-chronic-kidney-disease-among-first-nations/
