Volume 19 Number 2
Understanding burnout in the current nephrology nursing workforce and health service ‘magnet’ qualities that may help address it: a discreet choice experiment
Kathleen Hill, Kim Neylon, Kate Gunn, Greg Sharplin, Marion Eckert
Keywords burnout, workforce, nurse, nephrology
For referencing Hill K et al. Understanding burnout in the current nephrology nursing workforce and health service ‘magnet’ qualities that may help address it: a discreet choice experiment. Renal Society of Australasia Journal 2023; 19(1):87-92.
DOI
https://doi.org/10.33235/rsaj.19.1.87-92
Submitted 8 May 2023
Accepted 24 June 2023
Abstract
Objective Australia is currently experiencing a shortage of nursing staff that will have a negative impact on nursing specialties. We examined the current Australian and New Zealand nephrology nursing workforce for measures of burnout as well as for the features of ‘magnet’ qualities that can attract staff, support the workforce and reduce attrition.
Methods A co-designed 57-item survey was distributed to the nephrology nursing workforce online through membership of the Renal Society of Australasia. The survey used the Oldenburg Burnout Inventory (OLBI) and included a discreet choice experiment (DCE) in which respondents are offered different choices, blinded to the intention, and asked to rank in order of highest priority what they considered to be the most valuable organisational attributes.
Results The 253 respondents to the OLBI described moderate burnout (mean score 40.4); however, the respondents were mostly still able to describe feeling a sense of achievement most days. For the 143 respondents who completed the DCE, they chose professional educational opportunities to be ranked number one as the most important organisational attribute for recruiting and retaining nephrology nurses, with options for career progression ranked number two.
Conclusion The sustainability of the nephrology nursing profession depends upon organisations recognising burnout in their workforce and taking action to incorporate ‘magnet’ qualities to increase professional education opportunities and career progression opportunities to stabilise the workforce.
Introduction
Australia is experiencing a shortage of qualified nursing staff, as was predicted by Health Workforce Australia nearly a decade ago (Health Workforce Australia, 2014). Shortages have been compounded by the COVID‑19 pandemic which has increased both the demand for nurses and workloads and, as a result, levels of burnout (Mannino et al., 2021). The pressure on the nursing workforce has never been greater, so it is an important time to critically examine strategies to sustain this sector.
Additionally, further examination is needed on how this nursing shortage impacts specialty areas such as nephrology nursing. There has been a steep increase in chronic kidney disease (CKD) in Australia and New Zealand in recent years (Australia and New Zealand Dialysis and Transplant Registry, 2021), likely driven by high rates of comorbid diabetes and an ageing population. When CKD progresses to end stage kidney disease (ESKD), kidney replacement therapy (KRT) is required. Provision of CKD care and KRT (haemodialysis, peritoneal dialysis and transplantation) is a highly specialised nursing field and, in tandem with the overall nursing shortage, there is also a global shortage of trained nephrology nurses able to provide this care (Boyle et al., 2022; Wolfe, 2014). Nephrology nurses cannot simply be replaced by generalist nurses due to the complexity of the role and the advanced practice skills and education grounding required to provide quality care. Existing staff shortages are forcing nephrology trained nurses to do unwanted overtime, work past the end of the shift time, and/or leave important care incomplete (Boyle et al., 2022; Hill et al., 2021). This creates a negative work environment and is likely to increase levels of burnout and compound staff shortages (McKeaveney et al., 2021). Previous research has shown that burnout can lead to unsafe care practices. Mudallal et al. (2017) found that working conditions for nurses contributed most to the quality of patient care, and it has also been demonstrated that nurses experiencing burnout are five times more likely to leave necessary care undone (White et al., 2019).
The burnout seen in dialysis nurses is known to be particularly high (Hayes et al., 2015). Positive organisation factors are known to reduce the impact of stressful working environments and reduce burnout (Hayes et al., 2014; Kavurmacı et al., 2014). Burnout, as defined by the authors of the Oldenburg Burnout Inventory (OLBI), is “the impact of high job demands on exhaustion and the impact of low job resources on disengagement” (Demerouti et al., 2003). This validated tool has been widely used to study the health professions (Demerouti et al., 2000). Burnout in nursing is thought to occur when there is an increase in work pressure, staff shortages, high turnover and a lack of organisational efforts to increase job satisfaction (Gardner et al., 2007; Jones, 2014) resulting in the depersonalisation of the workforce. Organisations with a commitment to the ‘magnet’ qualities of greater job satisfaction, low nursing staff turnover, increased autonomy, educational and career opportunities and sharing in institutional decision making are known to improve patient outcomes and create a superior reputation for the organisation that enhances recruitment and retention (Harolds & Miller, 2020).
Aims
We sought to measure burnout in the current nephrology nursing workforce and to understand the ‘magnet’ quality attributes that might ameliorate this.
Methods
A 57-item survey was co-designed by the multidisciplinary research team; the demographic and work characteristic results from the whole survey have been published previously (Hill et al., 2023). The survey included the OLBI to measure burnout in the current nephrology nursing workforce and a discreet choice methods experiment (DCE), the results of which are described in this manuscript. The 24-item DCE explores the organisational qualities that respondents valued most (Weber, 2019). DCE surveys vary from traditional surveys in that they create options to choose from, allowing the data to identify preferences.
Using binary regression, participants were randomly allocated into two groups to answer 12 questions each. Respondents were asked to choose between two similar organisations (Organisation A or Organisation B) based on four attributes that were presented for each organisation in randomly allocated combinations. These were the three ‘magnet’ qualities of educational opportunities, qualification requirements and opportunities for career progression; location was included as a fourth quality. Through these hypothetical scenarios, the importance of each organisational attribute could be measured and ranked in relation to other attributes. This allowed us to identify qualities to recruit, retain and grow the nephrology nursing workforce. The DCE qualities were determined by the data collected in our previous qualitative work with nephrology nurses (Hill et al., 2021).
The survey was firstly piloted in Qualtrics™ with a small group of nephrology nurses (n=10) for internal and external validity. Changes made based on feedback, and the final survey was then hosted on the Qualtrics™ survey platform for data collection. The survey was then distributed via the Renal Society of Australasia to all members of this professional organisation via their electronic communications. The survey was open to respondents from December 2021 to April 2022.
Ethical considerations
This research was approved by the CALHN HREC reference number 12818.
Results
Summary of demographic and workplace data from the previously reported results (Hill et al., 2023)
A total of 370 respondents completed the larger survey and described a strong professional identity as a nephrology nurse. Working conditions were cited as challenging, with 70% working unpaid overtime and pressured to work overtime or stay past the shift end time. Only 2% reported that their workplace was currently adequately staffed, and half of the respondents reported care “left undone” due to staffing issues. Almost all respondents reported that patients with kidney disease were “sicker” than 10 years ago, almost half were concerned that their patients’ clinical care was “unsafe” at times and one third described the complete erosion of work-based educational opportunities. However, on a positive note, nursing and medical team collegiality was reported as high, known to be a strength of a caring profession (Hill et al., 2023).
Burnout
The OLBI questionnaire was completed by 253 respondents from various locations around Australia and New Zealand. The OLBI includes 16 questions that relate to both ends of the energy continuum (exhaustion – vigour) and identification continuum (cynicism – dedication) (Demerouti et al., 2000; Demerouti et al., 2003). Each question is scored between 1 and 4. Out of between 16 (no burnout) and 64 (highest burnout), the mean score for respondents was 40.4 (range 19–58; SD 8.0). Exhaustion items scored consistently slightly higher than disengagement items, with a mean disengagement score of 18.9 and a mean exhaustion score of 21.5.
Consensus was found for item 2, “there are days when I feel tired before I arrive at work” and item 12 “after working, I usually feel worn out and weary”, with mean scores of 3.24 and 3.16 out of 4 respectively, indicating slightly higher levels of exhaustion than disengagement amongst respondents.
Nevertheless, a sense of achievement was mostly (46.7%) or sometimes (31.9%) felt at the end of the workday by the majority of respondents (mean 2.26; SD 0.77). A total of 15.8% felt a sense of achievement every day. Only 4.7% (n=14) reported to never feel a sense of achievement.
Discreet choice experiment
In relation to the DCE component of this survey, three different criteria were offered for each attribute, providing 16 opportunities to select each criterion. Through these hypothetical scenarios (as described previously), the importance of each organisational attribute could be measured and ranked in relation to other attributes.
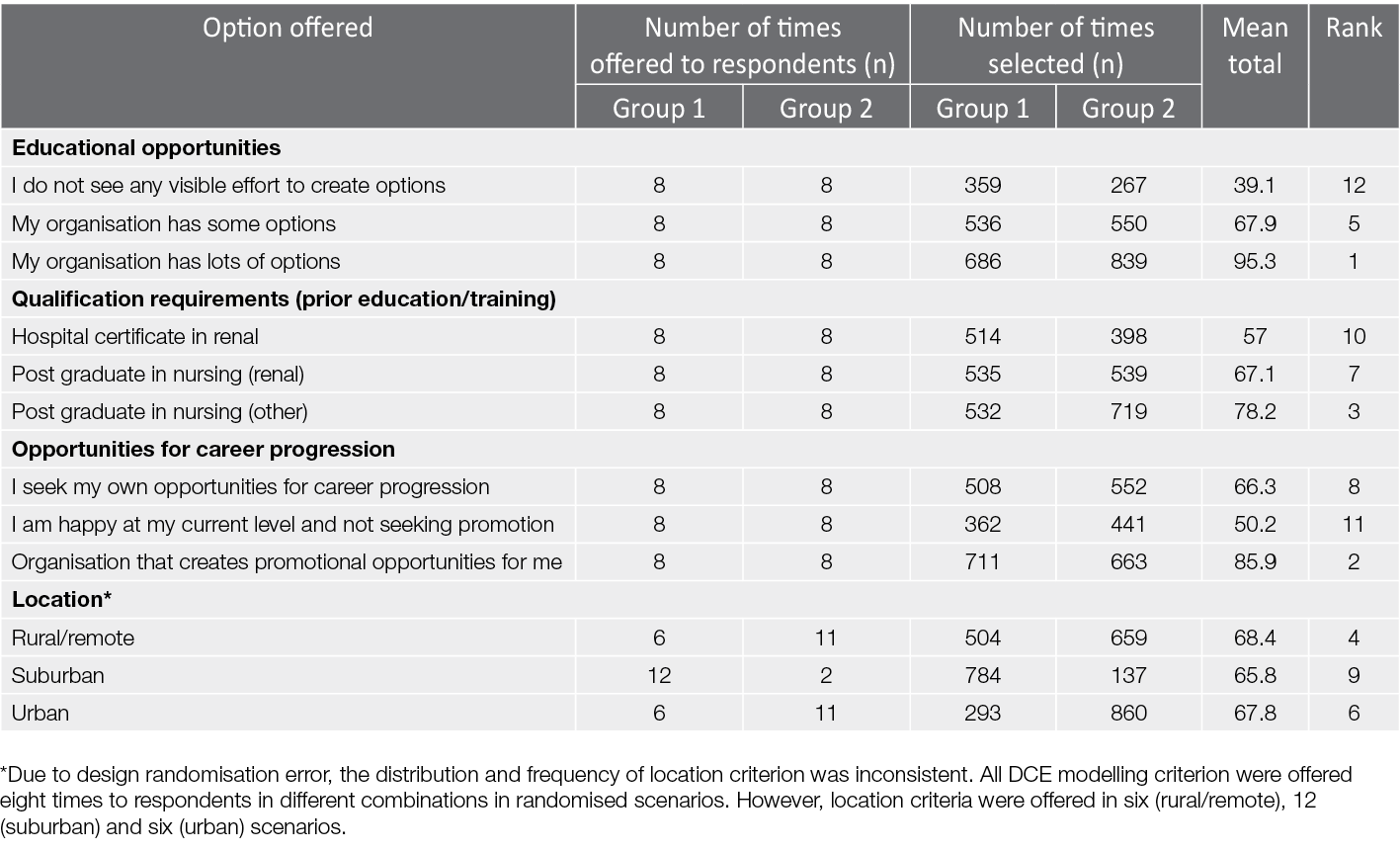
A total of 143 respondents completed this section of the survey. Table 1 illustrates how many times a scenario was selected that contained each attribute. Education was most valued by respondents, with “my organisation has lots of options” for education ranked first in terms of ‘magnet’ qualities, followed by an organisation that supports career progression (“organisation that creates promotional opportunities for me”) ranked second. Similarly, the lowest ranking options were “I do not see any visible effort to create options” for education (12th) and “I am happy at my current level and not seeking promotion” (11th). The requirement for post-graduate qualifications in nursing (other) was rated third, while the requirement of only a hospital certificate in nephrology was ranked lowest (10th). The three locations offered were ranked similarly (2.6 difference) and were therefore not considered as important when selecting scenarios based on these provided organisational attributes.
Overall, the largest consensus in both groups was found in hypothetical scenarios that included “lots” of educational opportunities. For Group 1, scenario 9, where the only variable difference was that the workplace of choice provided lots of educational opportunities, 120 (94.5%) selected “lots” of educational opportunities compared to seven that selected “I do not see any visible effort to create options”. For Group 2, “my organisation has lot of options” for education and “creates promotional opportunities” was selected by 122 respondents (89.1%), whereas no educational opportunities and “I am happy at my current level and not seeking promotions” was selected by only 15 respondents.
Table 1. DCE selection of attributes by respondents
Discussion
Our survey found moderate self-reported burnout among the 253 respondents using the OLBI scale. The average level of burnout (40.4) is slightly higher than reported in a large global study of nursing burnout (37.8) (Itzhaki et al., 2015). Respondents in the larger survey had reported workplace conditions that could be seen to contribute to self-reported burnout levels that related to inadequate staffing and workforce pressure (Hill et al., 2023). While complexity of care is a major driver of workforce pressure, there is little consensus on what an adequate workload is in nursing (Alghamdi, 2016), and the complexity of acuity and care is known to be poorly measured in nephrology nursing care (Australian Nursing and Midwifery Federation (ANMF), 2017). Nevertheless, our respondents reported that increased patient acuity and patient ratios contribute to their professional burnout.
An underlying driver of high stress levels and burnout in nursing is compassion fatigue which is exposure to a continuous cycle of suffering and empathy (Cross, 2019). This can lead to the protective mechanism of detachment and superficial caring (Delgado et al., 2017). As kidney conditions are largely degenerative, this could negatively impact the nephrology nursing workforce (Wolfe, 2014). Other research has found that nurses, when genuinely engaging in deep caring, feel rewarded for their emotional labour (Delgado et al., 2017) which reduces the likelihood of burnout. Almost all participants in the larger survey responded that they valued their long-term relationships with their nephrology patients, indicating that engagement with patients was viewed positively and that, in general, the teams’ internal trust and culture was very positive (Hill et al., 2023) and may therefore reduce perceptions of burnout amongst respondents.
This is further supported by our findings, as exhaustion items were rated higher (indicating more burnout) than disengagement items on the OLBI scale. This indicates that respondents self-reported feeling overworked slightly more than disengaged or dissatisfied with their work in nephrology nursing. These findings align with findings from focus groups with 36 nephrology nurses that were carried out by the research team prior to this national survey (Hill et al., 2021). Nephrology nurses have a strong professional identity and levels of achievement that they find satisfaction in and this, to some extent, ameliorates the perception of burnout (Hill et al., 2021; Hill et al., 2023).
Our respondents showed a tendency towards exhaustion, rather than disconnection, regarding self-reported burnout. This was also evident when most respondents reported that they felt a sense of achievement and fulfilment at least sometimes, although optimism about their jobs and prospects were mixed. Other research has found that, whilst individual nurses may utilise self-care factors to reduce the impact of stress and burnout, organisational efforts are critical to nurses coping with stress, including adequate staffing with an appropriate skill mix and support to manage very unwell patients (Jones, 2014). Without such support, exhaustion and burnout may increase in the workforce. Further institutional support to reduce workload or improve workplace conditions for nurses could improve burnout. However, our respondents in the larger survey indicated that such institutional support was limited in their workplaces (Hill et al., 2023).
Other studies have emphasised the important role of organisational management style and supervisory support on retention and job satisfaction. For example, nurses in general are drawn to organisations that address workloads with appropriate staff-to-patient ratios to provide safe and quality care (Mudallal et al., 2017; White et al., 2019). Managerial efforts to increase the size of a nursing team have also been found to best reduce absenteeism and turnover due to stress (Sant’ana et al., 2019).
Our research in this area has also found that the COVID‑19 pandemic has seen the gradual erosion of workplace education and training opportunities due to staff shortages and social distancing requirements (Hill et al., 2021; Hill et al., 2023); however, this is expressed as the highest workplace priority by the survey respondents (ranked number one). Educational opportunities and tuition benefits are viewed as a ‘magnet’ qualities (Gardner et al., 2007; White et al., 2019). Alarmingly, almost half of all respondents in our study were not optimistic about opportunities for career progression, and a third saw no visible effort to create promotional opportunities. This was despite “opportunities for career progression” being ranked second (behind “provides educational opportunities”) in the DCE section of the survey, highlighting its importance for retention, and therefore the importance of further effort needed in this space.
Our survey found that most respondents saw themselves as part of a cohesive team (Hill et al., 2023). Conveying respect in conversations to avoid stress and fostering a respectful kind culture is also key to reducing workplace stress (Dos Santos et al., 2016; Moreland & Apker, 2016). Nurses also need to be encouraged to practise mindful caring with the people that they care for rather than depersonalisation to reduce the impact of stress (Hunter, 2016).
Implications for clinical practice
The nephrology nursing profession have identified that a rewarding role is the best way to reduce burnout and exhaustion. A sense of purpose is found when the workforce is offered educational opportunities to increase their clinical skill levels and capacity for practice, and when their efforts are rewarded with opportunities for career progression. Health services need to recognise that rather than be defeated by high patient volumes, high acuity and increased workloads, nursing staff can still find personal accomplishment in their roles if active measures are taken to show that they are valued. Professional development is essential for evidence-based practice, is rewarding, contributes to team support and can help to address “spiralling” turnover (Opperman et al., 2022).
Conclusion
This survey of the nephrology nursing workforce has found high levels of exhaustion and moderate levels of burnout consistent with the known challenges facing the nursing profession globally. Importantly, the respondents have told us that professional educational opportunities and prospects of career progression are a highly desired ‘magnet’ quality for retention of this critical specialty workforce.
The nephrology nursing workforce will face important challenges over the next decade and urgent action is needed to address training needs, staff shortages and succession planning. The future growth and success of the nephrology nurse speciality is not just sitting with the individual but aligns with the ‘magnet’ principles. As such, a focus on supporting the professional growth of clinicians as well as building expertise and opportunities for clinical practice and support that relates to a genuine commitment to the infrastructure by the healthcare providers is needed. Organisations should be held accountable for staff wellbeing metrics and monitor them and act.
Conflict of interest
The authors declare no conflicts of interest.
Declaration of funding and acknowledgements
The authors gratefully acknowledge the funding support provided by the Rosemary Bryant Research Foundation and the Hospital Research Foundation that supported this work. We also acknowledge the support of Associate Professor Shilpa Jesudason and the clinical teams in South Australia for their support in shaping the direction of this work.
Data availability statement
The data that support this study cannot be publicly shared due to ethical or privacy reasons.
Author(s)
Kathleen Hill*
University of South Australia, Adelaide, SA, Australia
Kim Neylon
University of South Australia, Adelaide, SA, Australia
Kate Gunn
University of South Australia, Adelaide, SA, Australia
Greg Sharplin
University of South Australia, Adelaide, SA, Australia
Marion Eckert
University of South Australia, Adelaide. SA. Australia
Correspondence to Kathleen Hill, Centennial East Building, Frome Road, Adelaide, SA 5001, Australia
Email kathy.hill@unisa.edu.au
References
Alghamdi, M. G. (2016). Nursing workload: A concept analysis. Journal of Nursing Management, 24(4), 449–57.
Australia and New Zealand Dialysis and Transplant Registry. (2021). 44th annual report. Retrieved from: https://www.anzdata.org.au
Australian Nursing and Midwifery Federation (ANMF). (2017). Staffing renal dialysis unit. Retrieved from: https://www.anmfsa.org.au/
Boyle, S., Washington, R., McCann, P., Koul, S., McLarney, B., Gadegbeku, C. A. (2022). The nephrology nursing shortage: Insights from a pandemic. American Journal of Kidney Disease, 79(1), 113–116.
Cross, L. A. (2019). Compassion fatigue in palliative care nursing: A concept analysis. Journal of Hospice and Palliative Nursing, 21(1), 21–28.
Delgado, C., Upton, D., Ranse, K., Furness, T., & Foster, K. (2017). Nurses’ resilience and the emotional labour of nursing work: An integrative review of empirical literature. International Journal of Nursing Studies, 70, 71–88.
Demerouti, E., Bakker, A. B., Nachreiner, F., & Schaufeli, W. B. (2000). A model of burnout and life satisfaction amongst nurses. Journal of Advanced Nursing, 32(2), 454–464.
Demerouti, E., Bakker, A. B., Vardakou, I., & Kantas, A. (2003). The convergent validity of two burnout instruments: A multitrait-multimethod analysis. European Journal of Psychological Assessment, 19(1), 12–23.
Dos Santos, T. M., Kozasa, E. H., Carmagnani, I. S., Tanaka, L. H., Lacerda, S. S., & Nogueira-Martins, L. A. (2016). Positive effects of a stress reduction program based on mindfulness meditation in Brazilian nursing professionals: Qualitative and quantitative evaluation. Explore: The Journal of Science and Healing, 12(2), 90–99.
Gardner, J., Thomas-Hawkins, C., Fogg, L., & Latham, C. (2007). The relationships between nurses’ perceptions of the hemodialysis unit work environment and nurse turnover, patient satisfaction, and hospitalizations. Nephrology Nursing Journal, 34(3), 271–281.
Harolds, J. A., & Miller, L. B. (2020). Quality and safety in healthcare, part LXXVI: The value of Magnet® hospital recognition. Clinical Nuclear Medicine, 47(2), e218-e220.
Hayes, B., Douglas, C., & Bonner, A. (2014). Predicting emotional exhaustion among haemodialysis nurses: A structural equation model using Kanter’s structural empowerment theory. Journal of Advanced Nursing, 70(12), 2897–2909.
Hayes, B., Douglas, C., & Bonner, A. (2015). Work environment, job satisfaction, stress and burnout among haemodialysis nurses Journal of Nursing Management, 23, 588–598.
Health Workforce Australia. (2014). Australia’s future health workforce – Nurses overview. Retrieved from: https://www.health.gov.au/topics/health-workforce
Hill, K., Neylon, K., Gunn, K., Jesudason, S., Sharplin, G., Britton, A., ... Eckert, M. (2021). Sustaining the renal nursing workforce. Renal Society of Australasia Journal, 17(2), 39–45.
Hill, K., Neylon, K., Gunn, K., Sharplin, G., & Eckert, M. (2023). The Australian and New Zealand nephrology nursing workforce: Clinical pressure and organisational culture. Contemporary Nurse, 1–9. https://doi.org/10.1080/10376178.2023.2172442
Hunter, L. (2016). Making time and space: The impact of mindfulness training on nursing and midwifery practice. A critical interpretative synthesis. Journal of Clinical Nursing, 25(7–8), 918–929.
Itzhaki, M., Treacy, M., Phaladze, N., Rumeu, C., Vernon, R., Marshall, B., ... Nelson, J. (2015). Caring International Research Collaborative: A five-country partnership to measure perception of nursing staffs’ compassion fatigue, burnout, and caring for self. Interdisciplinary Journal of Partnership Studies, 3(1), 1–20.
Jones, C. (2014). Stress and coping strategies in renal staff. Nursing Times, 110(10), 22–25.
Kavurmacı, M., Cantekin, I., & Tan, M. (2014). Burnout levels of hemodialysis nurses. Renal Failure, 36(7), 1038–1042.
Mannino, J. E., Watters, P., Cotter, E., Armstrong, N., Moore, G. A., Bongiorno, A. W., & Kelley, R. (2021). The future capacity of the nursing workforce: COVID‑19 pandemic’s impacts on new nurses and nursing students toward the profession. Nurse Educator, 46(6), 342–348.
McKeaveney, C., Reid, J., Carswell, C., Bonner, A., de Barbieri, I., Johnston, W., ... Noble, H. (2021). Experiences of renal healthcare practitioners during the COVID‑19 pandemic: A multi-methods approach. BMC Nephrology, 22(1), 301–301.
Moreland, J. J., & Apker, J. (2016). Conflict and stress in hospital nursing: Improving communicative responses to enduring professional challenges. Health Communication, 31(7), 815–823.
Mudallal, R. H., Saleh, M. Y. N., Al-Modallal, H. M., & Abdel-Rahman, R. Y. (2017). Quality of nursing care: The influence of work conditions, nurse characteristics and burnout. International Journal of Africa Nursing Sciences, 7, 24–30.
Opperman, C., Liebig, D., Bowling, J., Johnson, C. S., Stiesmeyer, J., & Miller, S. (2022). Measuring return on investment for professional development activities: Pandemic impacts and revised known cost of outcomes. Journal for Nurses in Professional Development, 38(6), 333–339.
Sant’ana, J. L. G., Maldonado, M. U., & Gontijo, L. A. (2019). Dynamics of stress generation and reduction in the nursing team at an oncology center. Revista Latino-Americana de Enfermagem, 27, e3156
Weber, S. (2019). A step-by-step procedure to implement discrete choice experiments in qualtrics. Social Science Computer Review, 39(5), 903–921.
White, E. M., Aiken, L. H., & McHugh, M. D. (2019). Registered nurse burnout, job dissatisfaction, and missed care in nursing homes. Journal of the American Geriatric Society, 67(10), 2065–2071.
Wolfe, W. A. (2014). Are word-of-mouth communications contributing to a shortage of nephrology nurses? Nephrology Nursing Journal, 41(4), 371–378.
