Volume 1 Issue 1
The role of the vascular access nurse practitioner in developing evidence, promoting evidence-based vascular access practice and improving health services
Amanda J Ullman, Tricia Kleidon, Claire M Rickard
Abstract
Complications and failure of intravascular devices place significant burden on nursing workloads, patient outcomes and the health care system. The development and implementation of evidence to improve clinical practice surrounding the insertion and management of intravascular devices is an ongoing challenge to which nurse practitioners (NPs) in vascular access can respond.
NPs use their clinical expertise to lead practice, facilitate change and monitor effectiveness of interventions to prevent complications. This places NPs in an ideal position to incorporate research into practice and lead the development of new research. But the demands and recency of the role means that NPs frequently find themselves inadequately prepared to lead the development and implementation of new research.
Collaborative relationships between NPs and academic researchers, scientific and clinical staff are necessary to promote effective and efficient health services, research and nursing practice. This is especially evident within the field of vascular access. Together, such collaborations are able to create and share knowledge that has meaning for the practitioners, to optimise the NP’s role, and provide a bridge to overcome gaps in knowledge translation and evidence implementation.
This paper aims to explore the research aspects of the vascular access NP role within the context of multidisciplinary health research collaborations. It uses a case study of an NP involved in a health research collaboration within the vascular access specialty to illustrate this development, and further describes the potential impact of NPs upon evidence-based practice development.
INTRODUCTION
The majority of patients who are admitted to hospitals require the insertion of an intravascular device (IVD)1-3. They permit the infusion of medicines into the blood circulatory system, a means to sample blood for diagnostic purposes and the application of invasive haemodynamic monitoring4. IVDs are used across all medical, surgical, palliative and critical care specialties and from hospital to home environments.
Despite their necessity and ubiquity, the insertion, ownership and management of IVDs is frequently haphazard and the devices are prone to failure5. IVD failure prior to the end of therapy is commonly reported in 20–50% of peripheral, central and peripherally inserted central venous devices5-7. The insertion and management of IVDs needs to be based upon existing rigorous evidence that can reduce preventable failure as well as ongoing new research to improve the insertion experience. The multidimensionality and complexity of vascular access, and the variety of patients and health care providers involved in their care provides further challenges to the development and implementation of evidence-based practice in this field.
While advanced practice nursing roles in vascular access exist and contribute to excellence in some health services in Australia8, these roles (for example, clinical nurse consultants) are not regulated in the same way as nurse practitioners (NPs). Since their introduction, NPs have become leaders and innovators in clinical practice, especially within the field of vascular access. Internationally, the NP role was developed as an advanced practice nursing responsibility, with high levels of autonomy, collaboration and a broadened scope of practice compared to other registered nurses9,10. Like other advanced practice nursing roles, NPs are embedded in the health care system and are highly respected by other clinical staff members due to their credibility as local leaders in their specialty area of service provision. NPs use their clinical expertise to lead practice, facilitate change and monitor effectiveness of interventions to prevent complications11, which places NPs in an ideal position to incorporate research into practice through the integration of existing evidence and the development of new evidence9. All NPs have some level of research education and experience, as this is typically required for registration. However, NPs may not have adequate research knowledge and skills to independently critique or synthesise evidence or to design and lead research studies. Research has focused on the NP as the participant — rather than the investigator10,12,13. The role of NPs as research initiators, collaborators and advocates has not been adequately explored.
Collaborative relationships between academic, scientific and clinical staff are necessary to promote effective and efficient health-services research and interdisciplinary practice, within and outside of vascular access14,15. However, the mechanisms for enhancing clinical and academic collaborative relationships, such as joint clinical-academic appointments, rarely exist in health care. Hospitals and universities/research institutes focus principally in concordance with their immediate priorities, that is, clinical throughput and teaching/research respectively. This can contribute to the ‘evidence-practice’ gap, which continues to restrain health care from achieving its optimal efficiency and patient outcomes.
This paper aims to explore the role of NPs within multidisciplinary health research collaborations, to improve vascular access practice. It uses a case study of an NP in Australia involved in a health research collaboration within vascular access to illustrate this development, and further describes the potential impact of NPs upon evidence-based practice development.
RESEARCH AND EVIDENCE-BASED PRACTICE IMPLEMENTATION
Evidence-based vascular access practice requires an interdisciplinary, bench-to-bedside approach. Throughout health care the implementation of evidence-based practice at the bedside is a continuing struggle, with many authors lamenting the challenges associated with replacing traditional nursing habits with evidence-based practice16-19. The Cooksey Report20 from the United Kingdom (UK) distinguishes the varied layers of impediments to evidence-based practice implementation, highlighting the need for strategies which focus on both the first (scientist’s bench to product/process/service) and second gaps (their routine use in practice). The McKeon Report21 from Australia is similarly disparaging of the ‘separation’ of research functions from the hospitals and suggests greater integration of academic health centres. For effective implementation of evidence into practice to be achieved, systems that widely disseminate innovations need to be established and health care staff need to be skilled to critique, apply and evaluate evidence22.
Several studies have demonstrated that clinicians’ beliefs and attitudes about research are indicative of whether they will apply newly created evidence23-25. Clinicians across all health care disciplines also need to be engaged and participatory in the creation of the evidence in order to inform the generation of evidence across specific health disciplines22. To reduce barriers to health care research and evidence implementation, health care leaders have supported the creation of an infrastructure to engage clinicians in evidence-based practice and the research process26. These infrastructure strategies have included journal clubs, evidence-based practice programmes, health care research councils, centres of research excellence, research symposiums, clinical research fellowships and professor-in-residence programmes16,27-29. While innovative, these strategies are rarely effective when adopted in isolation, and without investment and endorsement by locally respected clinical leaders26,30.
COLLABORATIVE RESEARCH GROUPS
Current nursing and health research groups have learned from past programmes where academic groups based in the university sector have undertaken research in isolation and then found their research outcomes were out-of-touch and unacceptable for clinicians15. The Australian Governments’ National Health and Medical Research Council (NHMRC) Strategic Plan31includes a priority action to accelerate the research translation via collaboration between institutions towards research, translation, education and patient care. Both the NHMRC31 and the UK Medical Research Council32 highlight the need to plan implementation of research from the earliest inception of the research design, including involving future decision makers as an active strategy to progress evidence into practice. It is imperative that researchers consider end-users (for example, patients with an IVD and nurses who care for them) and the intricacies involved in implementing research into clinical practice from the outset of trial design. Research will have no impact if clinicians and health care policy makers ignore the results, and, conversely, if researchers do not understand why this occurs. A circular, integrative concept of health care research and implementation was illustrated by the UK Medical Research Council in 200533 (see Figure 1).
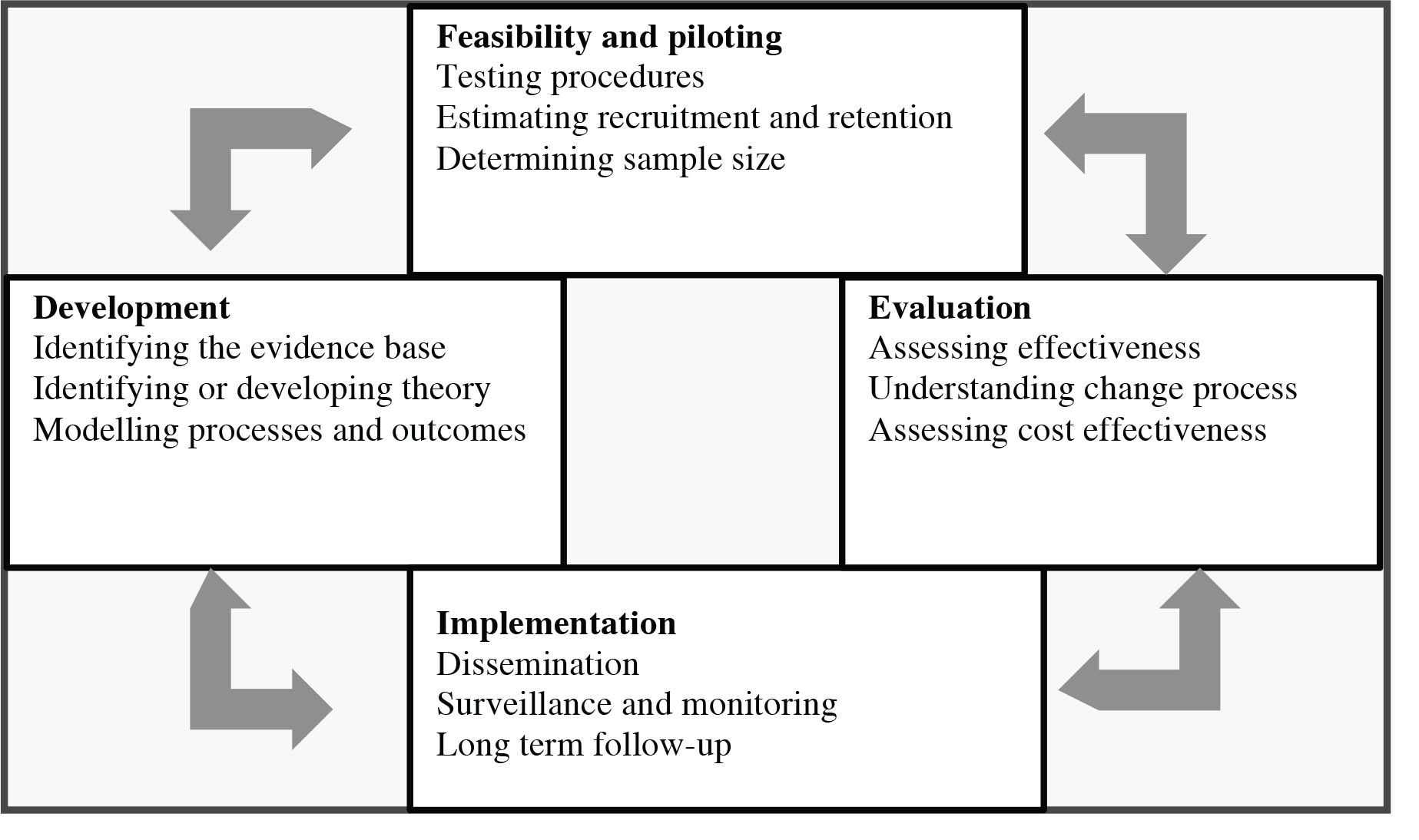
Figure 1. UK Medical Research Council: Key elements of the development and evaluation process.
Reproduced with permission from BMJ.com33
In response to these recommendations, research groups have developed collaborative partnerships between university-based academics and skilled clinical, scientific, administrative and educational staff. These partnerships share common purpose, goals, mutual respect, informed participation and shared decision making and often involve crossing the traditional discipline and sector silos15. They focus on the development, undertaking and implementation of research in a specific field, condition, topic or health care setting (for example, nursing, cystic fibrosis, vascular access, aged care).
Fostering partnerships between academics and clinical staff provides a means to develop and implement research programmes and outcomes. Communities of practice, such as clinical-academic research partnerships, provide a strategy to create and share knowledge which is meaningful for practitioners and increases the likelihood that research outcomes will be successful when implemented14. Each participant in the collaboration provides complementary strengths and capabilities to ensure a well-rounded approach to research development and implementation30. Health care systems are complex, and insufficiencies in health care delivery require the development of multilayered novel solutions32. An integrative, communicative, collaborative research group is required to find, develop and evaluate successful solutions.
THE ROLE OF NURSE PRACTITIONERS
The roles and responsibilities of NPs are expanding daily, with large representation practising within vascular access, predominantly within North America. NPs are now considered expert clinicians, educators, technicians, evidence-based practice advocates, opinion leaders and policy makers, capable of delivering high-quality, cost-effective care in a multitude of practice settings, including vascular access9,13,34. These high aspirations and expectations are supported by the outcomes achieved by this relatively new group of health professionals35-39.
Advanced care nurses and NPs are distinctively positioned to identify gaps in current evidence, as substantiated through their daily practice9. These gaps can inform the development of integrated and clinically orientated research. Internationally, NP training involves the completion of tertiary studies at the Masters or Professional Doctorate level, in the academic sector in collaboration with clinical settings40,41. Frequently the tertiary study includes the completion of research-based content, including research methodology, critique of evidence and the interpretation of statistical analysis42,43. With the training NPs receive during their candidacy, NPs are able to combine their expert clinical knowledge with their research familiarity — using the resources that academic–clinical research collaborations have to offer. This allows them to contribute to the development, undertaking, evaluation and implementation of evidence for practice. NPs can provide an intellectual and logistical bridge between the academic and clinical health care domains, which has benefit for all health care providers and recipients.
NPs do not work in isolation within their clinical practice. They are a familiar and respected resource for the multilayered, interdisciplinary health care team, able to provide knowledge and skills during research projects and beyond. Their advanced verbal and written communication skills used in their clinical practice and service development are invaluable when undertaking collaborative research projects. The skills and multifaceted roles of NPs as expert clinicians, educators, technicians, opinion leaders and policy makers, make them ideal and invaluable research collaborators for academic staff.
NPs have the potential to benefit from the resources available to them within the academic–clinical research collaboration. Academic faculty and clinical staff who are part of the research collaboration become an additional network of support and mentorship for the NP. This includes the availability of faculty with high-level research skills, training opportunities, support for research funding, manuscript preparation and project management expertise. They may also provide access to specialist non-clinical researchers such as statisticians and health economists. The collaboration has the means to be beneficial to all parties; including the patients, family members and health care service.
CASE STUDY: AN AUSTRALIAN NP IN A VASCULAR ACCESS RESEARCH COLLABORATION
After an extensive career in paediatric vascular assessment, insertion and device management in the United Kingdom, and later Australia, Ms Tricia Kleidon became the first NP in vascular access and management in Australia in 2013 at the Royal Children’s Hospital (RCH), Brisbane and since December 2014, the Lady Cilento Children’s Hospital, Brisbane. Her professional career has been dedicated to the development and implementation of evidence-based practice in the multidisciplinary field of paediatric vascular access. Ms Kleidon structures her practices as an NP using the Strong Model of Advanced Practice44. Within this model, five domains are utilised to support the advanced nursing practice role: direct comprehensive care; support of systems; education; research publication; and professional leadership.
To inform and develop her role as an advanced practitioner, Ms Kleidon developed a research collaboration with the Alliance for Vascular Access Teaching and Research (AVATAR) group, led by Professor Claire Rickard from the NHMRC Centre of Research Excellence in Nursing, Griffith Health Institute. Since its launch in 2007, the AVATAR Group has developed to become a truly multidisciplinary, collaborative, clinical and academic, teaching and research group with representatives ranging from nurses and medical practitioners from many clinical specialties (for example, intensive care, anaesthetics, surgery, infectious diseases, paediatrics), microbiologists, researchers, health economists and statisticians. The AVATAR Group’s goal is to develop evidence to ensure venous health and preservation through prevention of complications associated with intravascular access, using a multidimensional approach.
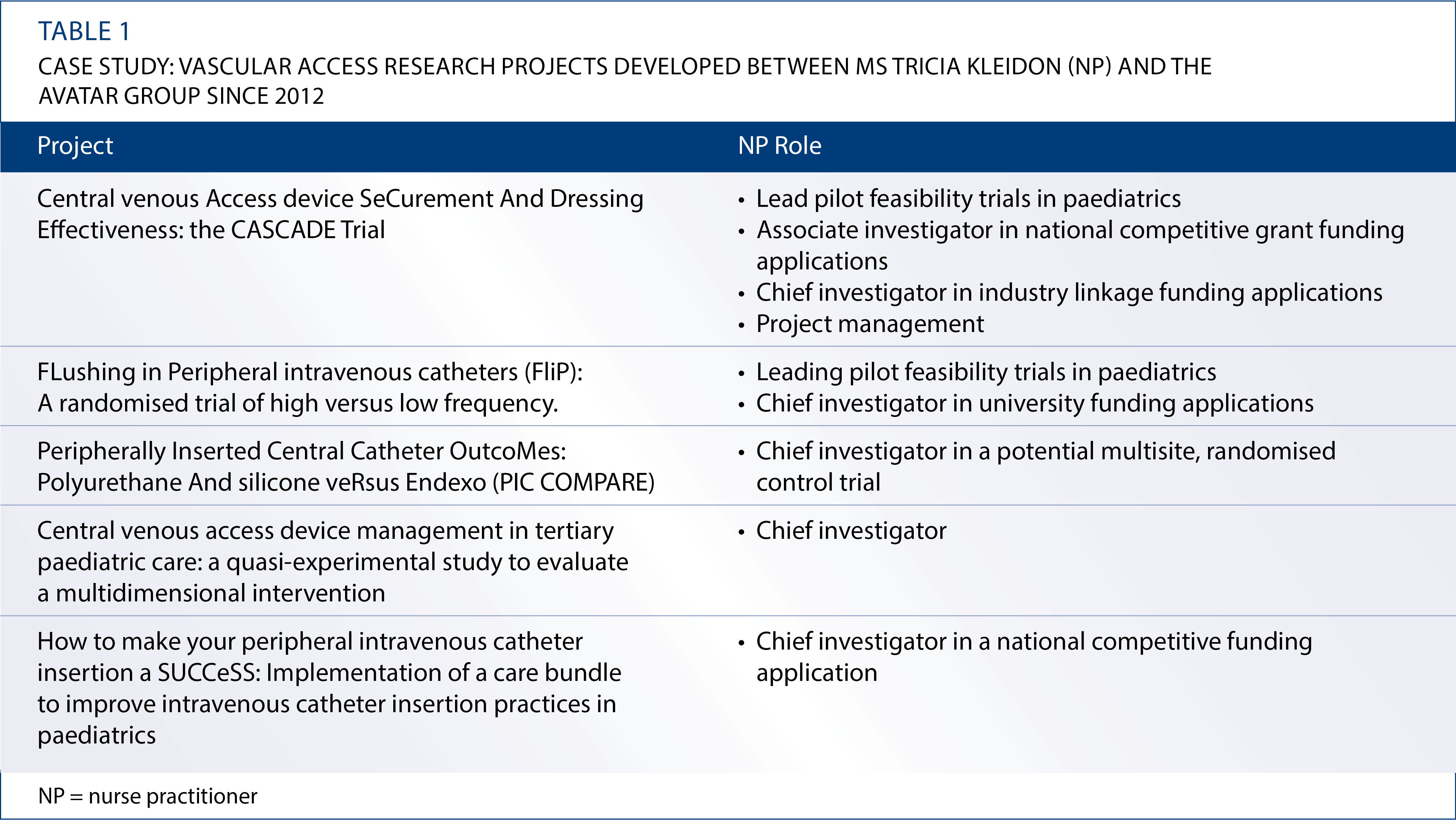
Ms Kleidon initially became involved in single-issue projects within the AVATAR Group, and is now a part-time research fellow within the research collaboration. Both the AVATAR Group and Ms Kleidon have benefited from the partnership, with a range of research projects developed, as seen in Table 1. In addition, Ms Kleidon provided content advice during the development of a postgraduate Master’s subject on vascular access. The AVATAR group has utilised Ms Kleidon’s expert and current clinical knowledge towards the development of research questions, informed research design and problem-solving practicalities regarding the projects’ implementation. The AVATAR Group has also utilised Ms Kleidon’s extensive network within the RCH to improve the feasibility of undertaking research, and to draw in other interested clinicians to work as research nurses, and to join the AVATAR Group. In reciprocation, Ms Kleidon has developed research skills including methodology, writing and project management under the tutelage of research leaders in the field of vascular access. The collaboration has resulted in mutual mentorship, with Ms Kleidon able to mentor researchers in advanced clinical expertise and skills. The health care staff, health care facility and patients at the RCH have benefited from the timely introduction of new vascular access evidence to the bedside. Both the RCH and Griffith University have benefited through the building of research and academic capacity through the mentorship of developing health care researchers.
The evidence-based care facilitation structure enabled by NPs is illustrated in Figure 2. It describes the people, benefits and outcomes that can be achieved by sharing the skills and knowledge available within the academic research group and health care institution domains.
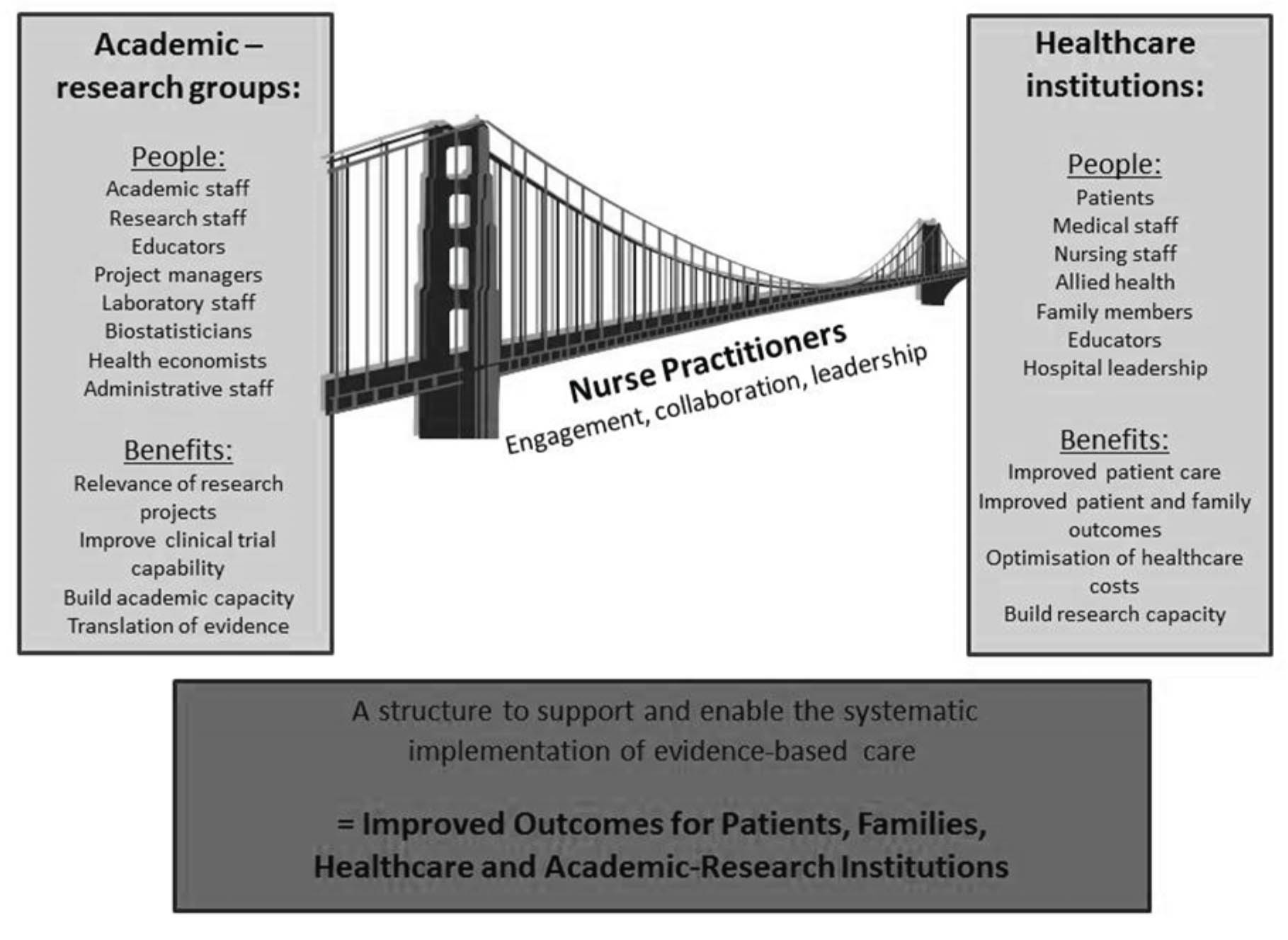
Figure 2. NPs as evidence-based care facilitators: an illustrative model
IMPLICATIONS FOR HEALTH CARE AND ACADEMIC INSTITUTIONS
Barriers to clinicians’ use of research and implementation of evidence are predominantly related to attitudes, challenges in effecting practice change, lack of knowledgeable mentors and insufficient resources (for example, time and personnel) to conduct research26,45,46. Within vascular access and beyond, academic–clinical research collaborations provide the necessary resources and skills that would otherwise make clinical research unachievable and the implementation of evidence impossible. Together these collaborations enable the creation and sharing of knowledge that is meaningful for the practitioners and can bridge the gap in translating knowledge and implementing evidence.
The mutual growth of research capacity has benefits for health care and academic institutions. The research will translate to improve patient care and outcomes and increase the skill set of both clinicians and academics15. Academic staff maintain their programme of research grounded in clinical practice, which is relevant to the bedside15. The implementation of evidence-based practice in the field of vascular access has the ability to save health care funds, through the reduction of preventable complications and wasted resources. A recent Australian example of research-based cost savings in vascular access includes the move from routine to clinically indicated replacement of peripheral IVDs. This is estimated to save A$7.60 per patient and approximately A$5 million over 5 years47. Further savings with the institution of future vascular access research is realistic.
The role of the NPs within these collaborations needs to be further explored and evaluated for effectiveness. Their involvement in research has the potential to drive sustained improvements in health care which are informed by clinical need and supported by the rigour of high-level research. A balance needs to be achieved so that NPs are not overwhelmed with the responsibilities of research to the detriment of their other roles and responsibilities as a clinician. However, the completion of direct patient care is not mutually exclusive from the other important domains of an advanced practice nurse, as some aspects of practice involve multiple characteristics of the roles demands.
Moving forward, NPs and academic health care staff need to seek opportunities to collaborate to ensure they optimise the creation and translation of evidence into clinical practice, especially within the field of vascular access. Together they have an opportunity to discover innovative, clinical- and cost-effective solutions and ensure their rapid and successful implementation at the bedside.
CONCLUSION
The prevention of complications associated with IVDs (for example, catheter-related bloodstream infection, occlusion and venous thrombosis) requires the development of rigorous evidence and the coordinated implementation of the outcomes of this research. This paper has outlined a model for the development and integration of vascular access research, which invigorates both NP roles and clinical-academic research groups based on collaboration, mutual respect and complementary knowledge and skills. As NP roles increasingly proliferate in the health care system, models such as these must become more visible and productive to progress consistent, evidence-based care, and clinically relevant, scientifically rigorous projects that have benefits to the community and the health sector.
CONFLICT OF INTERESTS
The authors have received funding from government, university and commercial entities for their research unrelated to this paper. The authors declare that there are no conflicts of interests regarding the publication of this paper.
ACKNOWLEDGEMENTS
The authors would like to thank the AVATAR group, the NHMRC Centre of Research Excellence in Nursing, and the RCH Nursing Directors for their support in developing this research collaboration.
Author(s)
Amanda J Ullman RN, GCert PICU, MAppSci a,b, Tricia Kleidon RN, MNursPrac a,b,c, Claire M Rickard RN, PhD a,b a. NHMRC Centre of Research Excellence in Nursing, Griffith University, Nathan Campus, Qld, Australia b. Centre for Health Practice Innovation, Nathan Campus, Menzies Health Institute Queensland, Griffith University, Qld, Australia c. Royal Children’s Hospital, Herston, Brisbane, Qld, Australia
References
- Maki DG, Kluger DM & Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc 2006; 81(9):1159–71.
- Pérez-Granda MJ, Guembe MR, RincÓn C, Muňoz P & Bouza E. A prevalence survey of intravascular catheter use in a general hospital. J Vasc Access 2014 Nov–Dec; 15(6):524–8. DOI: 10.5301/jva.5000272. Epub 2014 Jul 8.
- Australian Institute of Health and Welfare. Australian Hospital Statistics. In: AIHW, ed. Canberra: AIHW, 2014.
- Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014; 86 Suppl 1:S1–70.
- Rickard CM, Webster J, Wallis MC, Marsh N, McGrail MR, French V et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet 2012; 380:1066–74.
- Lim MY, Al-Kali A, Ashrani AA, Begna KH, Elliott MA, Hogan WJ et al. Comparison of complication rates of Hickman((R)) catheters versus peripherally inserted central catheters in patients with acute myeloid leukemia undergoing induction chemotherapy. Leuk Lymphoma 2013; 54(6):1263–7.
- Napalkov P, Felici DM, Chu LK, Jacobs JR & Begelman SM. Incidence of catheter-related complications in patients with central venous or hemodialysis catheters: a health care claims database analysis. BMC Cardiovasc Disord 2013; 13(1):86.
- Alexandrou E, Spencer TR, Frost SA, Mifflin N, Davidson PM & Hillman KM. Central venous catheter placement by advanced practice nurses demonstrates low procedural complication and infection rates — a report from 13 years of service*. Crit Care Med 2014; 42(3):536–43.
- Archibald MM & Fraser K. The potential for nurse practitioners in health care reform. J Prof Nurs 2013; 29(5):270–5.
- MacLellan L, Higgins I & Levett-Jones T. Medical acceptance of the nurse practitioner role in Australia: A decade on. J Am Assoc Nurse Pract 2014.
- Franks H. The contribution of nurse consultants in England to the public health leadership agenda. J Clin Nurs 2014.
- Fox K. The role of the acute care nurse practitioner in the implementation of the commission on cancer’s standards on palliative care. Clin J Oncol Nurs 2014; 18 Suppl:39–44.
- ter Maten-Speksnijder A, Grypdonck M, Pool A, Meurs P & van Staa AL. A literature review of the Dutch debate on the nurse practitioner role: efficiency vs. professional development. Int Nurs Rev 2014; 61(1):44–54.
- Campbell S, Prater M, Schwartz C & Ridenour N. Building an empowering academic and practice partnership model. Nurs Adm Q 2001; 26(1):35–44.
- Bowland MG, Kaamikawa C, Inouye J, Latimer R & Marshall S. Partnership to build research capacity. Nurs Economic$ 2010; 28(5):314–21.
- Ravert P & Merrill KC. Hospital nursing research program: partnership of service and academia. J Prof Nurs 2008; 24(1):54–8.
- Bohnenkamp S, Pelton N, Rishel CJ & Kurtin S. Implementing evidence-based practice using an interprofessional team approach. Oncol Nurs Forum 2014; 41(4):434–7.
- Wuchner SS. Integrative review of implementation strategies for translation of research-based evidence by nurses. Clin Nurse Spec 2014; 28(4):214–23.
- Squires JE, Hutchinson AM, Bostrom AM, O’Rourke HM, Cobban SJ & Estabrooks CA. To what extent do nurses use research in clinical practice? A systematic review. Implement Sci 2011; 6:21.
- Cooksey D. A review of UK health research funding. London, UK: HM Treasury, 2006.
- Government A. Strategic Review of Health and Medical Research in Australia — Better Health Through Research. In: Ageing DoHa, editor. Canberra, Australia: Commonwealth of Australia, 2013.
- Holzhauser K, Cooke M, Winch S, Finucane J & Davis C. Developing a research-active clinical environment within the emergency department: a case study. J Prof Nurs 2008; 24(1):36–41.
- Profetto-McGrath J, Hesketh KL, Lang S & Estabrooks CA. A study of critical thinking and research utilization among nurses. West J Nurs Res 2003; 25(3):322–37.
- Profetto-McGrath J, Smith KB, Hugo K, Patel A & Dussault B. Nurse educators’ critical thinking dispositions and research utilization. Nurse Educ Pract 2009; 9(3):199–208.
- Chaudoir SR, Dugan AG & Barr CH. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci 2013; 8:22.
- Atkinson M, Turkel M & Cashy J. Overcoming barriers to research in a Magnet community hospital. J Nurs Care Qual 2008; 23(4):362–8.
- Milne DJ, Krishnasamy M, Johnston L & Aranda S. Promoting evidence-based care through a clinical research fellowship programme. J Clin Nurs 2007; 16(9):1629–39.
- Schulman CS. Strategies for starting a successful evidence-based practice program. AACN Adv Crit Care 2008; 19(3):301–11; quiz 12–3.
- Forrester DA, O’Keefe T & Torres S. Professor in residence program: a nursing faculty practice. J Prof Nurs 2008; 24(5):275–80.
- Lasker R, Weiss E & Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Q 2001; 79(2):179–205.
- Australian Government. NHMRC Strategic Plan: 2013–2015. In: Council NHaMR, ed. Canberra: Commonwealth of Australia, 2012.
- Medical Research Council. Developing and evaluating complex interventions: new guidance. In: Council MR, ed. UK, 2006.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I & Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008; 337:a1655.
- Fawdon H & Adams J. Advanced clinical practitioner role in the emergency department. Nurs Stand 2013; 28(16–18):48–51.
- McDevitt J & Melby V. An evaluation of the quality of emergency nurse practitioner services for patients presenting with minor injuries to one rural urgent care centre in the UK: a descriptive study. J Clin Nurs; 2014.
- Kapu AN, Thomson-Smith C & Jones P. NPs in the ICU: the Vanderbilt initiative. Nurse Pract 2012;37(8):46-52.
- Skinner H, Skoyles J, Redfearn S, Jutley R, Mitchell I & Richens D. Advanced care nurse practitioners can safely provide sole resident cover for level three patients: impact on outcomes, cost and work patterns in a cardiac surgery programme. Eur J Cardiothorac Surg 2013; 43(1):19–22.
- Lau LH, Kerr D, Law I & Ritchie P. Nurse practitioners treating ankle and foot injuries using the Ottawa Ankle Rules: a comparative study in the emergency department. Australas Emerg Nurs J 2013; 16(3):110–5.
- Kapu AN, Kleinpell R & Pilon B. Quality and financial impact of adding nurse practitioners to inpatient care teams. J Nurs Adm 2014; 44(2):87–96.
- Middleton S, Gardner A, Gardner G & Della PR. The status of Australian nurse practitioners: the second national census. Aust Health Rev 2011; 35(4):448–54.
- Smith NJ. Professional doctorates and nursing practice contribution: a systematic literature search and descriptive synthesis. J Nurs Manage 2013; 21(2):314–26.
- Burman ME, Hart AM, Conley V, Brown J, Sherard P & Clarke PN. Reconceptualizing the core of nurse practitioner education and practice. J Am Acad Nurse Pract 2009; 21(1):11–7.
- Brar K, Boschma G & McCuaig F. The development of nurse practitioner preparation beyond the master’s level: what is the debate about? Int J Nurs Educ Scholarsh 2010; 7:Article9.
- Mick DJ & Ackerman MH. Advanced practice nursing role delineation in acute and critical care: application of the strong model of advanced practice. Heart Lung 2000; 29(3):210–21.
- Schoonover H. Barriers to research utilization among registered nurses practicing in a community hospital. J Nurses Staff Dev 2009; 25(4):199–212.
- Strickland RJ & O’Leary-Kelley C. Clinical nurse educators’ perceptions of research utilization: barriers and facilitators to change. J Nurses Staff Dev 2009; 25(4):164–71; quiz 72–3.
- Tuffaha H, Rickard C, Webster J, Marsh N, Gordon L, Wallis MC et al. Cost-effectiveness analysis of clinically indicated versus routine replacement of peripheral intravenous catheters. Applied Health Economics and Heath Policy, 2014; epub ahead of print.
