Volume 1 Issue 2
Association between multiple IV attempts and perceived pain levels in the emergency department
J. Matthew Fields, Nicole E. Piela, Bon S. Ku
Abstract
Purpose: Intravenous (IV) access is the most commonly performed procedure in the emergency department (ED). Patients with difficult venous access require multiple needlesticks (MNS) for successful IV cannulation and may experience increased pain with many attempts.
Objective: To determine the association between number of IV attempts and overall pain experienced by the patient from IV placement.
Methods: Cross-sectional observational study on consecutive patients undergoing IV placement with a 20-gauge IV in the upper extremity in an urban academic hospital. Exclusion criteria included refusal to participate or fully complete all survey questions. The total number of IV attempts and patient pain scores marked on a standardized visual analog scale was recorded. Mean pain scores of two groups, single needlestick (SNS) and MNS, were compared using Student’s t-test.
Results: A total of 760 patients were approached, of whom 31 were excluded, leaving 729 patients in the analysis; 556 with SNS (76%) and 173 with MNS (24%). The mean pain score (95% CI) was 51 mm (46-55 mm) for the MNS group and 25 mm (23-28 mm) for the SNS group, p<0.001. Compared to patients who underwent one IV attempt, patients with two and three attempts had an average 19 mm and 33 mm increase in pain scores, respectively, with the highest average pain associated with five attempts. A total of 58% of MNS patients rated IV placement as the most painful experience while in the ED.
Conclusions: Patients experience increased pain in association with multiple IV attempts.
Key words: Difficult venous access, Pain, Peripheral intravenous catheter, Procedure
Reprinted from J Vasc Access 2014 ; 15 (6 ): 514 -518 with permission of the Publisher.
INTRODUCTION
Intravenous (IV) access is the most commonly performed procedure in the emergency department (ED), ranging between 26% and 32% of all patients seen in the ED (1). In the 2010 National Hospital Ambulatory Medical Care Survey database, approximately 27% of all ED visits required IV placement for parenteral fluid administration (2). The pain inflicted by IV placement is typically accepted as an unavoidable consequence in delivering emergency care. However, pain associated with IV access might be higher than expected (3-6). Interventions designed to mitigate this pain have been shown to have varying success (6, 7).
The pain associated with IV placement may be more significant in patients who have to experience it repetitively. Patients with difficult venous access (DVA), by definition, require multiple needlesticks (MNS) for successful IV cannulation. Approximately 25% of patients undergoing IV placement in an emergency setting require more than one IV attempt (8, 9). While it is reasonable to expect that pain experienced with IV placement would increase when multiple attempts are required, this phenomenon has never been studied. Decreasing the pain and anxiety in patients who receive IV access may be a worthwhile pursuit especially with the increasing availability of technologies such as infrared vein detectors and portable ultrasound machines. The current study set out to determine the correlation between number of IV attempts and overall pain experienced by patients. We hypothesized that patients undergoing MNS will have higher pain scores than those who have successful IV placement on the first attempt.
MATERIALS AND METHODS
Study design and setting
This was a cross-sectional observational study of patients undergoing IV placement conducted from July 2012 to February 2013. The institutional review board granted study approval. The study was conducted in an urban
academic hospital with an active emergency medicine residency program and an annual census of 65,000.
Selection of participants
This study included adult patients presenting to the ED who required IV placement. Consecutive stable patients who had a 20 gauge IV placed or attempted in the upper extremity during their ED stay were enrolled during periods of block enrollment between July and October 2012. Trained research associates screened and enrolled patients 16 hours a day, 7 days a week. All patients underwent informed verbal consent. Patients who refused IV placement or data collection were excluded from the analysis. Research associates visited each ED treatment space sequentially and consecutively to determine when a patient had an IV placed or attempted. A patient was consented and enrolled only after an IV was successfully placed or attempts at inserting an IV ceased.
Methods and measurements
The total number of IV attempts was confirmed with nursing and technician staff. For assessment of pain patients marked on a 10 cm visual analog scale similar to other studies assessing pain from IV placement (3-6). Patients were asked to rate the pain associated with the entire process of IV placement. The participants were also asked to rate whether IV placement was the most painful event experienced during their ED stay as well as to comment on their overall satisfaction with the ED visit on a scale from 1 to 10 (with 1 being “very dissatisfied” and 10 being “very satisfied.”)
Outcomes
The primary outcome was the highest level of pain experienced during the entire IV placement (all attempts). Secondary variables included patient characteristics, whether the patient rated the IV placement as the most painful experience during their ED visit and overall satisfaction with their ED experience. A previous study has shown that a change of 13 mm on a visual analog scale is associated with a “significant” increase in pain (10). Given that average pain in patients undergoing a single IV attempt was 33 mm (SD 29 mm) in a previous study (3) and we wanted to detect a 13 mm increase, we required approximately 105 patients in each group, assuming an alpha of 0.05 and power of 0.9. We made a conservative estimate that 15% of patients enrolled would undergo multiple IV attempts requiring a total enrollment of approximately 700 patients. Final goal enrollment was 750 to ensure that final sample size was adequate after any exclusions or incomplete data.
Analysis
Data were entered into an Excel spreadsheet (Microsoft Excel Version 14) and imported into a Stata (StataCorp 2009; Stata Statistical Software: Release 11, College Station, TX) for statistical analysis. Patients were divided into two groups for analysis: single needlestick (SNS) and MNS. All variables were tested for normality. Results are reported as frequencies with inter-quartile ranges or means with standard deviations. Comparisons between the groups were performed using chi-squared, student’s t-test and Mann-Whitney U-test, where appropriate. Previous studies have linked age <65 years and a history of depression with having higher pain scores with IV placement and a post hoc analysis was performed to determine if these associations were also present in this dataset.
RESULTS
A total of 760 patients were enrolled in this study of whom 31 were excluded due to incomplete data, leaving 729 meeting inclusion criteria. Of the 729 included, 556 (76%) underwent SNS and 173 (24%) underwent MNS for IV access. Demographic data (including age, race and levels of education for both groups) are represented in Table I.
Pain scores were higher in the MNS group (Fig. 1). The mean pain score (95% CI) was 51mm (46-55mm) for the MNS group and 25mm (23-28mm) for the SNS group, p<0.001. Compared to patients who underwent only one IV attempt, reported pain was on average 19 mm higher in patients who had a total of two IV attempts and 33 mm higher in patients who underwent three or more attempts, with the highest average pain reported in those who underwent five attempts (Fig. 2). In addition, 58% of the patients in the MNS group rated IV placement as the most painful experience while in the ED, compared to 48% of patients in the SNS group, p=0.01. Overall ED satisfaction was slightly lower in the MNS group (8.4, 95% CI 8.1-8.7) than the SNS group (8.8, 95% CI 8.7-9.0), p<0.01.
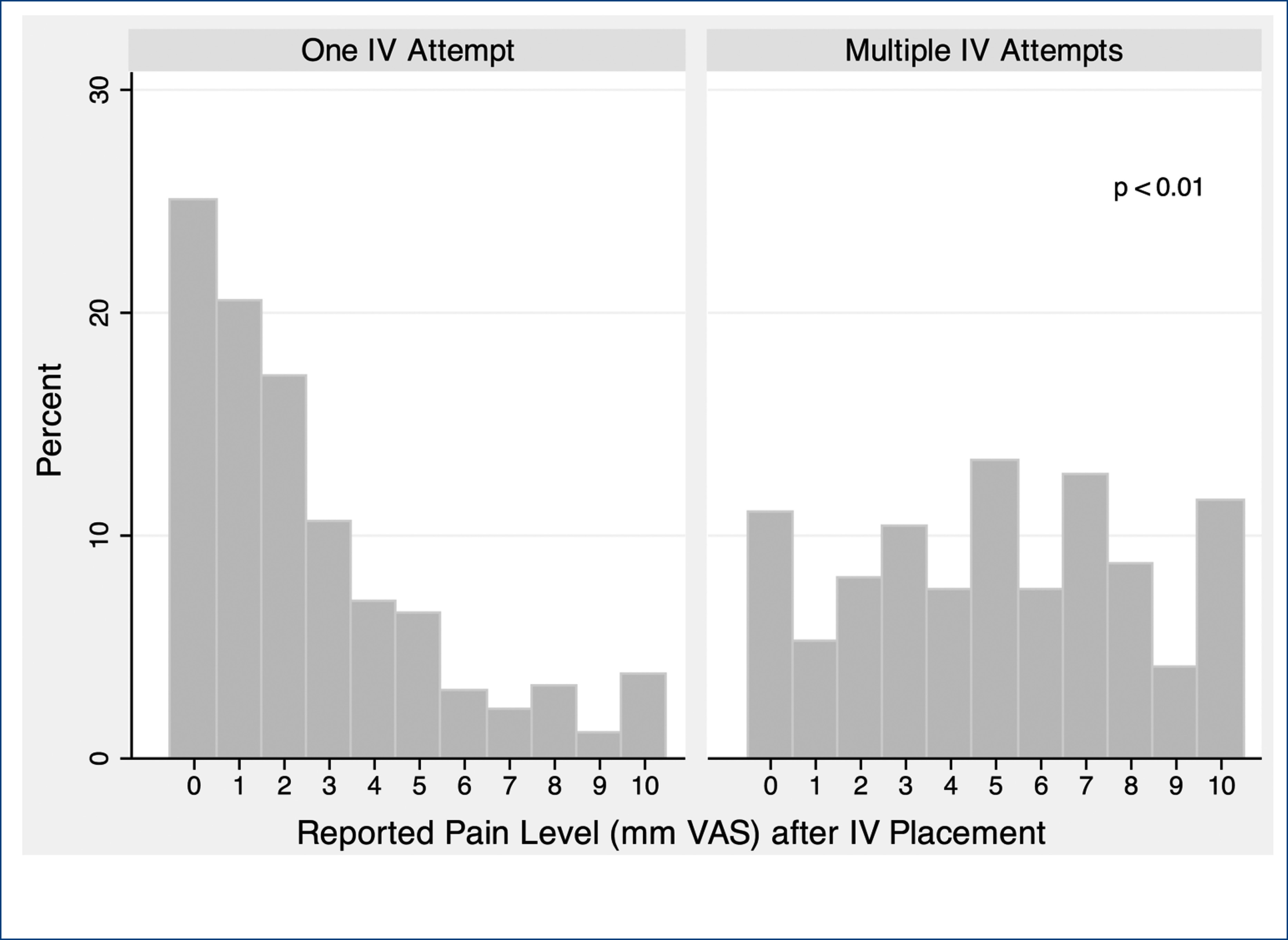
Fig. 1. Histograms of patient pain levels from IV placement.
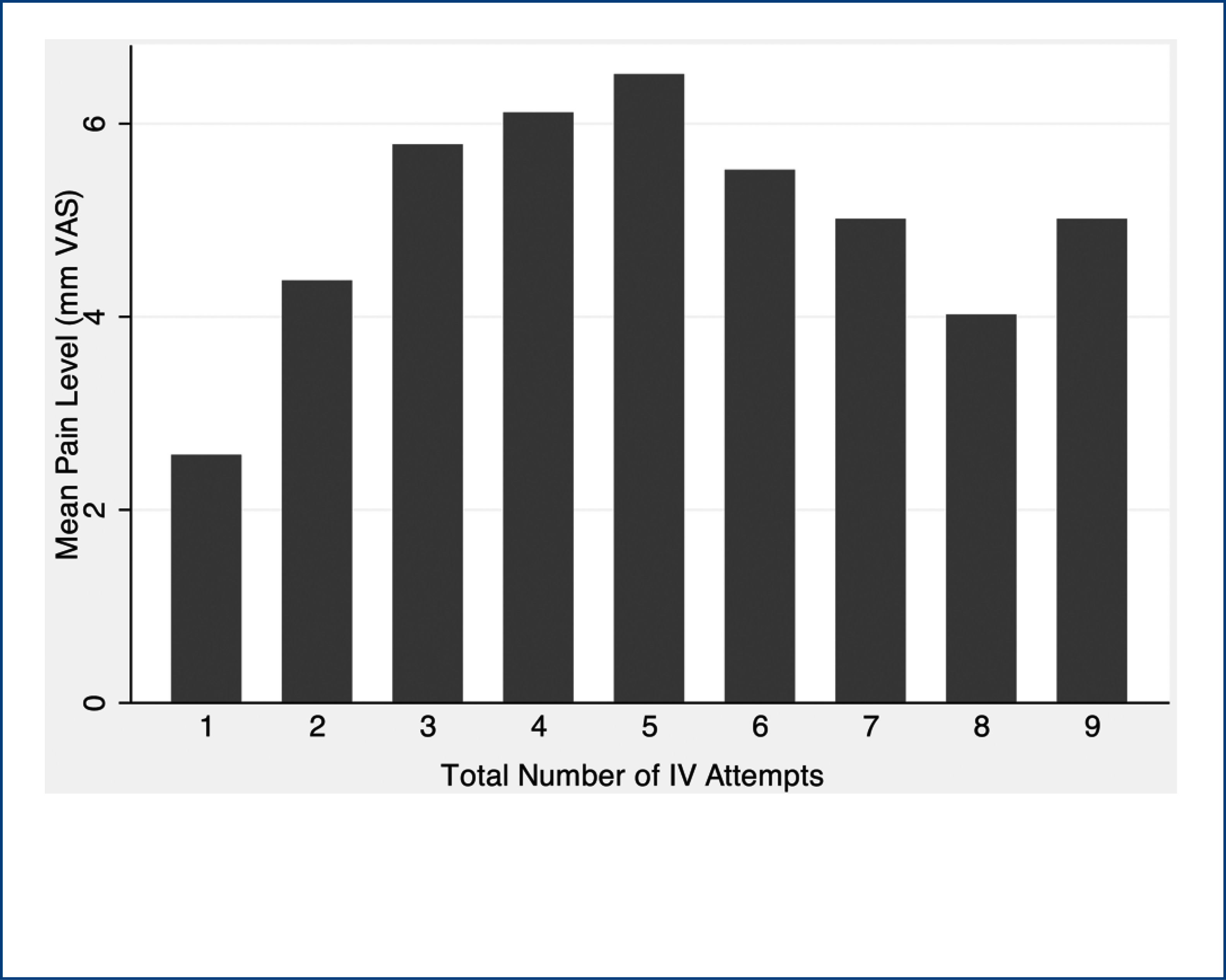
Fig. 2. Mean reported pain levels after IV replacement
Elderly patients (age > 64 years) were found to have lower pain scores, mean 24 mm (95% CI 20-29 mm) from IV placement, compared to non-elderly patients, mean 33 mm (95% CI 31-35 mm). Other variables such as gender, race, education level and history of depression did not have a significant effect on pain levels. In a multivariate ordered logistic regression, the effect of multiple IV attempts on pain levels was still present when controlling for age.
DISCUSSION
Healthcare providers seek to minimize pain in their patients but this is often difficult to do in EDs where many invasive procedures are performed. A study by Singer et al showed that nasogastric tube placement, abscess drainage and fracture reduction were the most painful procedures performed in the ED (11). Even though the pain associated with IV placement was not near the top of the list of most painful procedures, IV access still deserves special attention because it is the most commonly performed procedure. In our study the majority of patients tolerated a single IV attempt; however, repeated IV attempts caused a measurable increase on a pain visual analog scale. Previous studies have determined that a 13 mm increase in pain on a visual analog scale represents a clinically significant increase (10). We found that patients who underwent two IV attempts versus just one attempt had a 19 mm higher average pain score from the procedure, suggesting that even one failed attempt can cause significant pain.
Previous studies have explored potential factors associated with pain and IV placement. A study by Li et al found elderly patients tended to report lower pain scores from IV placement and a study by Marco et al found that a history of depression was associated with higher reported pain levels (5, 12). A third study found that pain from IV placement was specifically not influenced by baseline pain, race, gender or IV location (3). The current study further contributes to this knowledge base by demonstrating that the association with pain and repeat IV attempts was strongly significant. An additional finding from our study is that the largest increase in pain occurs with the initial additional attempts and upon reaching four to five attempts pain levels start to plateau and do not continue to increase. A possible explanation to this phenomenon is that repetitive IV attempts can lead to central sensitization to afferent pain fibers resulting in lower perceived pain.
Various techniques have been studied to decrease pain from IV placement including ice, topical analgesics and coolant sprays (7, 13). A different problem arises in patients with DVA as repeat attempts lead to incremental pain from the procedure and techniques to increase first stick success rates are warranted. Standard protocol to increase regional blood flow involves placing a tourniquet; hanging the arm in a dependent position; having the patient pump his fist or inflating a blood pressure cuff on the arm. Alternatively, other areas of the body such as the neck, legs or feet are used for venous access. Infrared technology has led to some improvement over initial techniques (14) and ultrasound guidance has enabled better localization of deeper veins and improved IV insertion. Multiple studies have demonstrated that physicians, nurses and technicians have been able to reduce the number of IV attempts and subsequent need for central venous catheters with sonographic guidance (15-18). While there was a slightly higher ED satisfaction rate in patients with a single IV attempt over those with multiple attempts, it is unclear whether interventions to reduce IV attempts will result in higher satisfaction levels.
There are several limitations to the current study. This was a single-center study in an urban ED and results may not be applicable to other settings. Because patients were asked about pain and satisfaction after IV placement, recall bias may have occurred. In addition, overall ED satisfaction is likely multifactorial and data on other factors that may have influenced this variable (wait time, provider interactions, etc.) were not collected. The finding of increased pain levels in patients undergoing multiple IV attempts may have been by association only. Further study is required to determine if the needlesticks themselves lead to the increased pain level or if this cohort of patients tends to report higher pain levels.
CONCLUSION
Patients experience increased and potentially significant pain in association with multiple IV attempts. Efforts to reduce the number of needlesticks experienced by patients may result in reduced pain from IV placement and may impact patient satisfaction.
Financial support: None.
Conflict of interest: The authors have no commercial associations or sources of support that might pose a conflict of interest.
Address for correspondence:
J. Matthew Fields, MD
Department of Emergency Medicine
1020 Sansom Street
Thompson Building
Suite 239, Philadelphia
PA 19107, USA
matthewfields@gmail.com
Author(s)
J. Matthew Fields, Nicole E. Piela, Bon S. Ku Department of Emergency Medicine, Thomas Jefferson University and Hospitals, Philadelphia, PA - USA
References
- Henderson RA, Thomson DP, Bahrs BA, Norman MP. Unnecessary intravenous access in the emergency setting. Prehosp Emerg Care. 1998;2(4):312-316.
- Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Report. 2010;(26):1-31.
- Li SF, Greenwald PW. How distracting is distracting pain? Am J Emerg Med. 2003;21(1):43-44.
- Soysal S, Topacoglu H, Karcioglu O, Serinken M, Koyuncu N, Sarikaya S. Analysis of factors affecting pain in intravenous catheter placement: a survey of 925 patients. Int J Clin Pract. 2005;59(6):675-679.
- Li SF, Greenwald PW, Gennis P, Bijur PE, Gallagher EJ. Effect of age on acute pain perception of a standardized stimulus in the emergency department. Ann Emerg Med. 2001;38(6):644-647.
- Hartstein BH, Barry JD. Mitigation of pain during intravenous catheter placement using a topical skin coolant in the emergency department. Emerg Med J. 2008;25(5):257-261.
- Eidelman A, Weiss JM, Lau J, Carr DB. Topical anesthetics for dermal instrumentation: a systematic review of randomized, controlled trials. Ann Emerg Med. 2005;46(4):
343-351. - Lapostolle F, Catineau J, Garrigue B, et al. Prospective evaluation of peripheral venous access difficulty in emergency care. Intensive Care Med. 2007;33(8):1452-1457.
- Sebbane M, Claret PG, Lefebvre S, et al. Predicting peripheral venous access difficulty in the emergency department using body mass index and a clinical evaluation of venous accessibility. J Emerg Med. 2013;44(2):299-305.
- Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001; 38(6):633-638.
- Singer AJ, Richman PB, Kowalska A, Thode HC Jr. Comparison of patient and practitioner assessments of pain from commonly performed emergency department procedures. Ann Emerg Med. 1999;33(6):652-658.
- Marco CA, Nagel J, Klink E, Baehren D. Factors associated with self-reported pain scores among ED patients. Am J Emerg Med. 2012;30(2):331-337.
- Page DE, Taylor DM. Vapocoolant spray vs subcutaneous lidocaine injection for reducing the pain of intravenous cannulation: a randomized, controlled, clinical trial. Br J Anaesth. 2010;105(4):519-525.
- Perry AM, Caviness AC, Hsu DC. Efficacy of a near-infrared light device in pediatric intravenous cannulation:
a randomized controlled trial. Pediatr Emerg Care. 2011;27(1):5-10. - Au AK, Rotte MJ, Grzybowski RJ, Ku BS, Fields JM.
Decrease in central venous catheter placement due to use of ultrasound guidance for peripheral intravenous catheters. Am J Emerg Med. 2012;30(9):1950-1954. - Bauman M, Braude D, Crandall C. Ultrasound-guidance vs. standard technique in difficult vascular access patients by ED technicians. Am J Emerg Med. 2009;27(2):
135-140. - Blaivas M, Lyon M. The effect of ultrasound guidance on the perceived difficulty of emergency nurse-obtained peripheral IV access. J Emerg Med. 2006;31(4):407-410.
- Brannam L, Blaivas M, Lyon M, Flake M. Emergency nurses’ utilization of ultrasound guidance for placement of peripheral intravenous lines in difficult-access patients. Acad Emerg Med. 2004;11(12):1361-1363.
