Volume 4 Issue 2
Pain upon inserting a peripheral intravenous catheter: Size does not matter
Fredericus HJ van Loon, Wesly H van Aarle, Angelique TM Dierick-van Daele, Arthur RA Bouwman
Abstract
Background: Approximately 1.2 billion peripheral intravenous catheters are inserted across the world annually. It is known that intravenous cannulation may be a painful procedure, which affects cognitive abilities by increasing anxiety and discomfort.
Aim: We hypothesised that inserting a smaller sized peripheral intravenous catheter has a lower level of pain sensation compared to a larger sized catheter.
Methods: This observational, cross-sectional study was conducted between May and October 2016, in which surgical patients, aged 18 years or older, were eligible to participate. Experienced anaesthesiologists and nurse anaesthetists routinely obtained peripheral intravenous access according to the standards of care. The primary outcome was pain (verbal numeric rating scale, 0–10) upon intravenous cannulation.
Results: A total of 1063 patients were included and they were divided into four groups: group 1, 22 gauge (N = 29); group 2, 20 gauge (N = 447); group 3, 18 gauge (N = 531); and group 4, sized over 18 gauge (N = 56). Inserting an 18-gauge peripheral intravenous catheter resulted in the lowest pain score (3.2 ± 2.0). As a result of the multivariate linear analysis, five factors were significantly associated with pain upon inserting a peripheral intravenous catheter (sex, American Society of Anesthesiology classification, a patient's risk profile on the A-DIVA scale, site of cannulation on the extremity, and whether or not the attempt was successful); however, the size of the inserted peripheral intravenous catheter had no significant relation to the primary outcome.
Conclusion: Inserting a smaller sized peripheral intravenous catheter did not result in a lower pain sensation. Moreover, to prevent pain upon inserting a peripheral intravenous catheter, an unsuccessful attempt must be avoided.
Keywords: Catheterisation, peripheral, pain, vascular access devices.
Date received: 6 January 2017; accepted: 6 November 2017.
Republished with permission: The Journal of Vascular Access 2018; 19(3):258–265. © The Author(s) 2018
Reprints and permissions: sagepub.co.uk/journalsPermissions.nav DOI: 10.1177/1129729817747531
https://doi.org/10.1177/1129729817747531 journals.sagepub.com/home/jva
![]()
INTRODUCTION
It has been reported that approximately 1.2 billion peripheral intravenous catheters (PIVCs) are inserted in hospitalised patients across the world annually1. Moreover, nearly four out of five patients admitted to the hospital receive a PIVC, which makes PIVC insertion one of the most commonly practiced invasive procedures by both medical and nursing staff2–4. Furthermore, intravenous cannulation is usually the first procedure performed by anaesthesiologists and nurse anaesthetists on patients presenting for procedures that require anesthesia or procedural sedation.
A PIVC is a small hollow catheter that is advanced over a needle into a peripheral vein through the skin. PIVC placement is indicated for short-term use in many clinical situations, such as administration of intravenous medications, fluids, antibiotics, or blood products. Common sites of cannulation are the cephalic or basilic veins of the upper extremity, of which the antecubital fossa and the dorsum of the hand are commonly preferred sites for routine intravenous cannulation5,6. The superficial veins of the lower limbs may also be cannulated; however, these tend to be avoided because they are associated with a higher risk of infection, phlebitis, and embolism5,7,8.
Factors influencing the site selection for PIVC placement are the general condition of the vein, types of drugs to be administered, duration of intended therapy, and size of the catheter versus size of the vein5,7. In clinical anesthesia practice, the size of the inserted PIVC depends on the clinical situation, while a larger sized PIVC has an increased speed of administration of intravenous fluids2,9. The size of the chosen catheter is normally determined by the expected surgical complexity, complications, and blood loss, ranging between 22 and 14 gauge in clinical practice2,10.
It is common for PIVC insertion to be a painful and invasive procedure, which therefore increases the anxiety and discomfort experienced by patients11–14. This affects their cognitive abilities and causes discomfort both mentally and physically15. To add to this, the anticipated pain prior to and upon cannulation significantly elevates a patient’s level of anxiety6. Moreover, as concluded by Macario et al.16, discomfort from PIVC insertion was found to be the fifth most important clinical problem in anesthesia practice.
However, it seems trivial that inserting a PIVC with a smaller diameter is thought to be less painful compared to a larger sized PIVC; no consensus was reached regarding this statement2,9. Thus, we hypothesise that inserting a smaller sized PIVC has a lower level of pain sensation compared to a larger sized PIVC when no additional analgesic technique has been applied. In addition to this hypothesis, we propose to identify factors that have an impact on pain during peripheral intravenous cannulation.
MATERIALS AND METHODS
Design
This observational, cross-sectional study was conducted between May and October 2016 and was performed in the operating theatre complex of Catharina Hospital (Eindhoven, The Netherlands). The institutional review board (Catharina Hospital, Eindhoven, The Netherlands) approved the study protocol (ref: 2013–59), and written informed consent was obtained from all patients.
Participants
Inclusion criteria are as follows: patients 18 years or older were eligible to participate in this study if scheduled for any surgical procedure, regardless of their American Society of Anesthesiology (ASA) classification, demographics, and medical history. Exclusion criteria are as follows: patients were excluded if they did not understand or answer the questionnaire (due to physical or communicational disorders), were unresponsive, or when a PIVC had already been inserted. Patients received usual care throughout the study and were consecutively included by independent practitioners during the study period. As a part of hospital policy, patients received premedication, consisting of 1g acetaminophen administered orally, approximately 60 min before cannulation, and no sedative premedication was administered.
Outcome measures
The primary outcome measure was pain felt during peripheral intravenous cannulation with the size of the inserted PIVC. Pain was scored on the verbal numeric rating scale (VNRS) for pain, which is a one-dimensional measurement scale for pain intensity in adults and is a segmented numeric version of the visual analog scale (VAS). The pain VNRS is a single 11-point numeric scale with “0” representing no pain and “10” representing the worst pain imaginable. Although a valid and reliable scale to measure pain intensity, the pain VNRS evaluates only one component of the pain experience and pain intensity17. Nevertheless, VNRS is an appropriate scale to measure pain upon intravenous cannulation and is simple to administer18,19. As secondary outcomes, this study tried to identify which, if any, of the independent variables of patient’s demographics (sex, age, body mass index (BMI), and ASA classification) or data related to the procedure of inserting a PIVC (puncture in the dominant site, site of cannulation on the extremity, diameter of the target vein, practitioner, whether or not the puncture was successful, and a patient’s risk for a difficult intravenous access as measured on the A-DIVA scale had a relation to pain upon inserting a PIVC10. Data were collected by the depending anaesthesiologist or nurse anaesthetist during performing the procedure of intravenous cannulation, by asking the patient or from the preoperative anesthesia chart, and registered on score forms; completed score forms were included in the dataset and analysed. To minimise bias and to maximise the validity of the results, both practitioners and patients were not aware of the primary outcome, and for that reason were blinded to the outcome measure pain during intravenous cannulation20. The pain scores were collected and recorded directly after performing each attempt by the dependent practitioner.
Procedure
Experienced anaesthesiologists and nurse anaesthetists routinely obtained peripheral intravenous access. PIVCs sized 14–22 gauge were inserted, and the size of the inserted catheter depended on the clinical situation and was chosen by the practitioner (Venflon Pro Safety; BD Infusion Therapy AB, Helsingborg, Sweden). Intravenous cannulation was performed according to practice guidelines, as described in a previous publication by Gorski8 and van Loon et al.10. Veins on the dorsal and ventral surfaces of the upper extremity were considered for peripheral cannulation, including the metacarpal, cephalic, basilic, and median veins. Peripheral intravenous cannulation was defined as successful if the practitioner was able to inject a saline flush without signs of extravasation or infiltration in the surrounding tissues5,8.
Statistical analyses
A difference in experienced pain felt during intravenous cannulation of at least a relative 30% of difference on the VNRS between the study groups was denoted to be clinically relevant21. The sample size needed was calculated as at least 41 patients for each group, assuming a mean difference of 30% regarding the baseline pain score from a previous study at α = 0.05 and β = 0.80.10 The post hoc power was calculated as 0.80. Power analysis was performed using G*Power (G*Power version 3.1.9.2; Christian Albrechts Universität, Kiel, Germany)22. The Kolmogorov–Smirnov test assessed the normality assumption for continuous variables. Continuous variables with a normal distribution were expressed as the mean and standard deviation, while those without a normal distribution were expressed the median and interquartile range. Discrete variables were expressed as frequencies with percentages. Comparison of variables between the study groups of inserted PIVCs was performed using one-way analysis of variance (ANOVA) testing (with Bonferroni post hoc analyses) or Chi-square testing, as appropriate. Stepwise multivariate linear regression technique was used to provide correlations between variables, in which items with a significant relationship to the primary outcome from a univariate linear regression technique were entered to determine the significance of the relationships between variables with the primary outcome. The stepwise method was utilised as the primary method of regression analysis in order to remove independent variables that did not make a significant contribution to the primary outcome variable. Items were removed from this model using a backward elimination process, with the removal criteria set at an α value of 0.01 as the level of significance, to obtain a model with a minimal set of variables and a maximal correlation coefficient (R2). Throughout the study, a p value less than 0.05 was denoted to be statistically significant. SPSS (version 21.0; SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
RESULTS
A total of 1063 patients were included in this study, whose demographic characteristics are represented in Table 1. Throughout the study, 1408 peripheral intravenous punctures were carried out with a first-attempt success ratio of 83%. For the analysis, patients were retrospectively subdivided into study groups based on the size of the inserted PIVC after an successful attempt, of which four groups were created: group 1, 22-gauge PIVC (N = 29); group 2, 20-gauge PIVC (N = 447); group 3, 18-gauge PIVC (N = 531); and group 4, PIVC sized over 18 gauge, including 17- and 14-gauge PIVCs (N = 56).
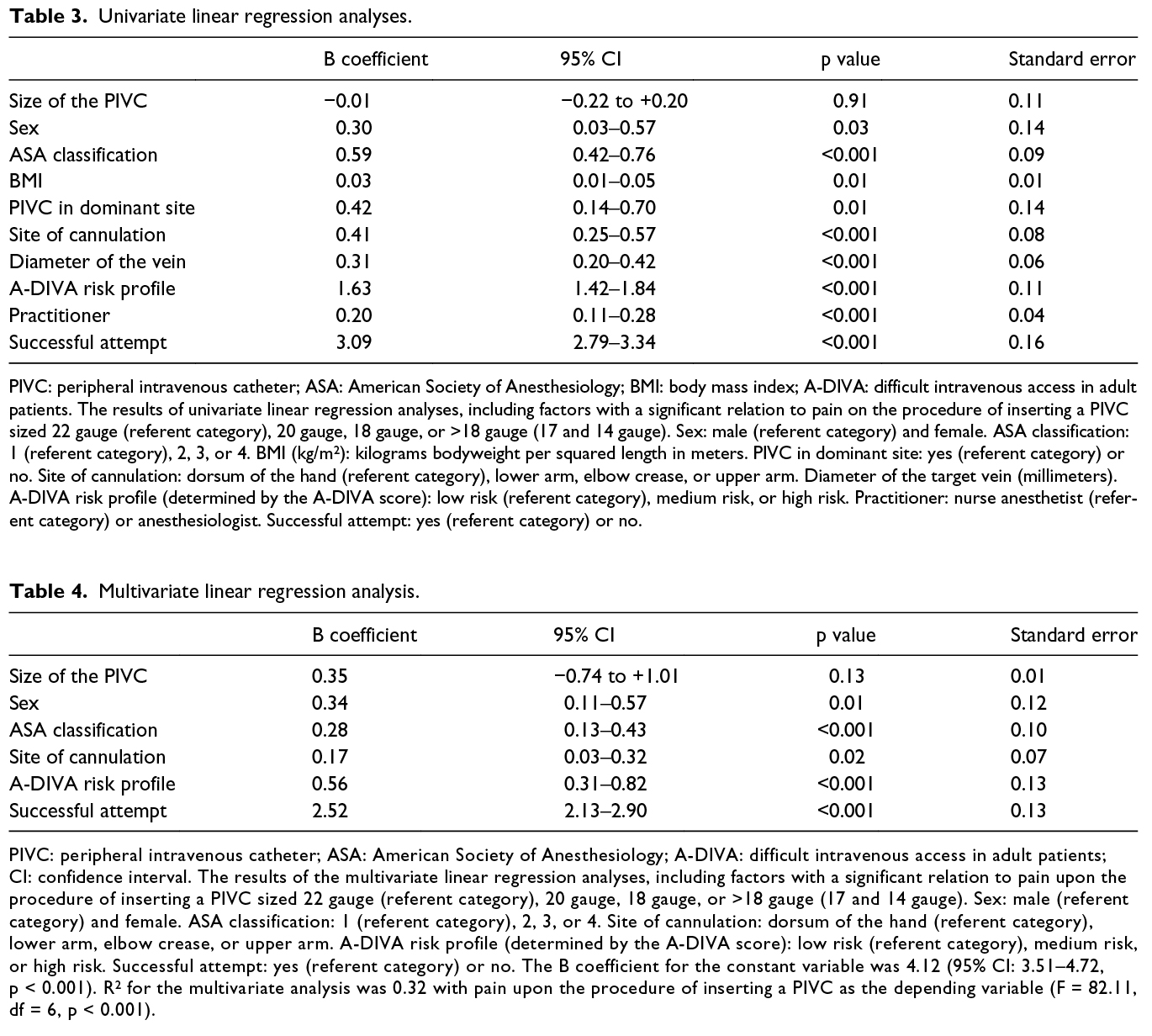
Inserting an 18-gauge PIVC resulted in a statistically significant lowest pain score of 3.2 ± 2.0, compared to other size PIVCs (F = 7.04, df = 3, p < 0.001), as shown in Table 2. Notwithstanding the statistically significant difference in pain sensation upon cannulation with an 18-gauge PIVC, a clinically significant difference was only detected in patients in whom an 18-gauge PIVC was inserted, compared to a 22-gauge PIVC or a PIVC sized over 18 gauge. The mean pain score of the total study cohort was 3.3 ± 2.2.
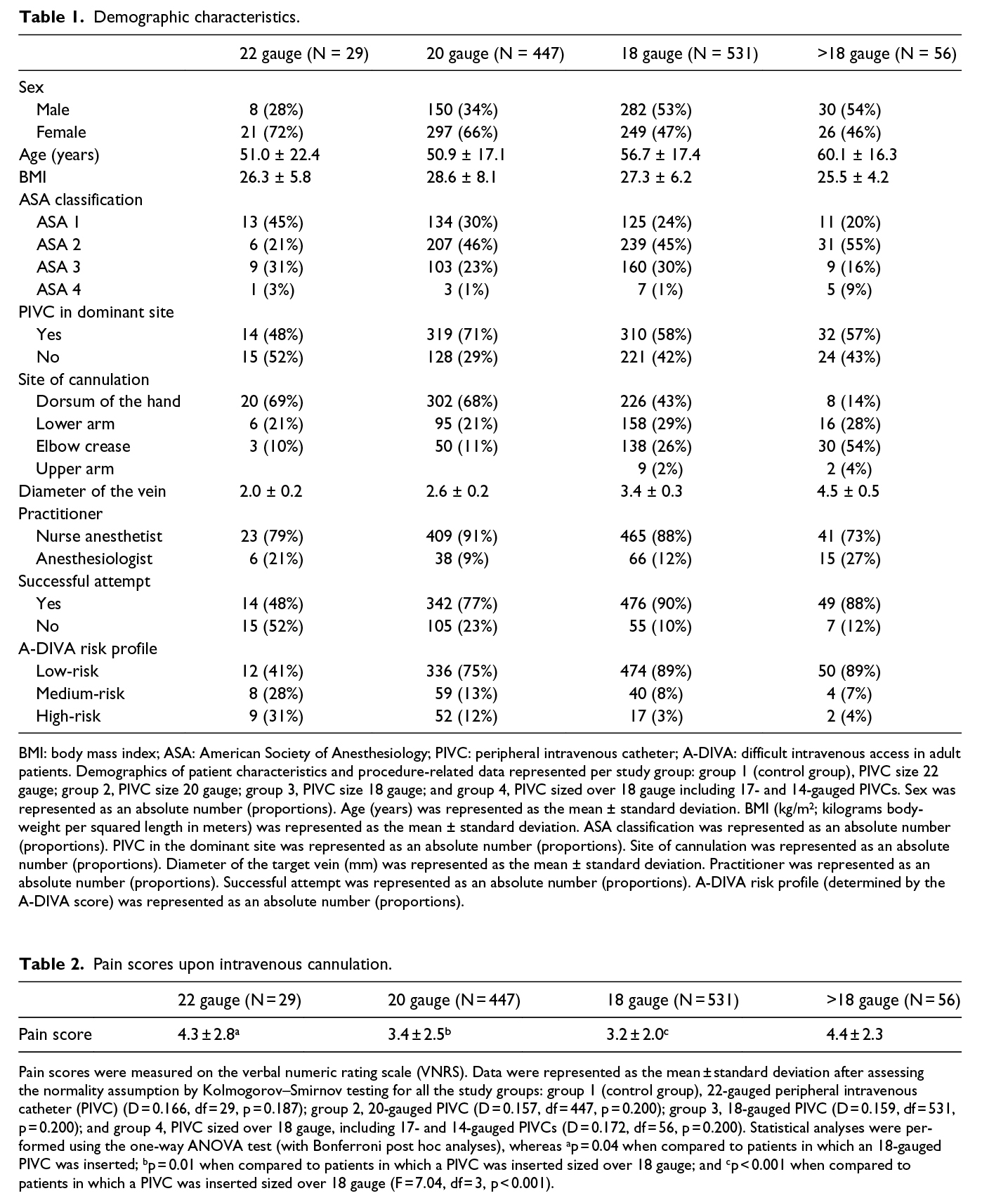
As a result of the univariate linear regression analyses, a total of nine variables had a significant relation to the outcome of interest (pain upon cannulation): sex; ASA classification; BMI; PIVC in the dominant site; site of cannulation on the extremity; diameter of the vein; practitioner; A-DIVA risk profile; and whether or not the attempt was successful (Table 3). Nonetheless, no significant relationship could be detected between pain upon cannulation and the size of the inserted PIVC as a result of this univariate analysis (B = 0.01 (95% confidence interval (CI) = 0.22 to +0.20), p = 0.91, standard error (SE) = 0.11). These significant variables from the univariate analyses were included in a multivariate linear regression analysis, including the variable size of the inserted PIVC. As a result of this analysis, five factors were significantly associated with the pain experienced upon inserting a PIVC (sex, ASA classification, site of cannulation on the extremity, A-DIVA risk profile, and whether or not the attempt was successful), as shown in Table 4. Actually, inserting a PIVC successfully at the first attempt on the dorsum of the hand in male patients with an ASA classification 1 and a low-risk profile on the A-DIVA scale resulted in the lowest pain score (R2 = 0.32, F = 82.11, df = 6, p < 0.001). In contrast, the size of the inserted PIVC had no significant relation to the primary outcome within this multivariate analysis.
DISCUSSION
The aim of this observational study was to demonstrate whether or not inserting a smaller sized PIVC has a lower level of pain sensation compared to a larger sized PIVC, when no additional analgesic technique has been applied. Additionally, we proposed to identify factors that had an impact on pain during peripheral intravenous cannulation. The hypothesis was rejected as a result of this study, concluding that inserting an 18-gauge PIVC resulted in the lowest pain score (3.2 ± 2.0). Both the smallest (22-gauge) and the biggest sized (over 18-gauge) PIVCs resulted in the highest pain scores during intravenous cannulation, with pain scores of 4.3 ± 2.8 and 4.4 ± 2.3, respectively. As a result of regression analyses, five factors were significantly associated with pain upon intravenous cannulation and had an independent relation to this outcome of interest: sex; ASA classification; A-DIVA risk profile; site of cannulation on the extremity; and whether or not the attempt was successful. The size of the inserted PIVC had no significant relation to the primary outcome.
The lowest pain score was registered in patients in whom the PIVC was inserted successfully at the first attempt on the dorsum of the hand in male patients with an ASA classification 1 and a low-risk profile on the A-DIVA scale. Noteworthy is the decent influence of an unsuccessful attempt on the level of pain sensation, which had an apparently higher impact on pain sensation compared to the other variables. However, the five variables in the multivariate analyses had a statistically significant relation to the outcome of interest independently, while only inserting a PIVC successfully at the first attempt had a clinically significant effect on pain sensation upon intravenous cannulation. The effect size of the other variables on the level of pain sensation upon inserting a PIVC was limited.
As concluded by Rivera et al.2, it is generally agreed that a larger sized PIVC allows faster transfusion with less haemolysis or risk for thrombosis, but carries a higher risk for pain and phlebitis. Smaller gauges, in contrast, are thought to have exactly the opposite advantage for array and risk profile. The presented pain scores of PIVCs sized over 18 gauge, as a result of our study, are in accordance with the study of Rivera et al.2. However, we were not able to prove the statement about lower pain scores in smaller sized catheters, as was concluded in the volunteer-based study by Brown9. In addition, we believe that pain, as experienced during intravenous cannulation, depends more on the cannulation site and patient characteristics than on the inserted size of the PIVC.
The clarifications for differences in the experienced pain between the sites of intravenous cannulation are unclear. Nevertheless, cannulation on the dorsum of the hand was thought to be more painful compared to the antecubital fossa due to the tougher skin and greater density of nociceptors on this site6,23,24. However, this study showed the opposite results while suggesting insertion of a PIVC on the dorsum of the hand in an effort to minimise pain during the procedure. Nevertheless, the risk for accidental removal and occlusion seems to be higher on the dorsum of the hand, as concluded by the trial of Wallis et al.25. To add to this, Bregenzer et al.26 even showed a higher incidence of PIVC obstruction in patients with a PIVC inserted on the dorsum of the hand compared to other cannulation sites on the upper extremity. Thus, it seems that catheter insertion in high-mobility areas contribute to the development of traumatic phlebitis or complications, which should be taken into account before choosing a cannulation site27,28. Site selection should likewise be determined based on the indication for PIVC placement, the time needed for intravenous treatment, the diameter of the vein, patients’ preferences, and the risk of complications due to the cannulation site.
An unsuccessful first attempt at inserting a PIVC is more often seen in patients in whom a smaller sized PIVC was inserted. This was in line with the predicted A-DIVA score; patients in whom a smaller sized PIVC was inserted were more often classified in a high-risk profile10. The A-DIVA score is based on the five variable additive A-DIVA scale, which is a reliable predictive rule that implies the probability to identify patients with a difficult intravenous access prospectively. Logically, the diameter of the target vein was smaller in the group of patients with the highest A-DIVA score compared to those with a low-risk profile. As shown in this study, a successful first attempt resulted in both statistically and clinically significant lower pain scores compared to unsuccessful attempts. Moreover, pain as experienced by patients increased with further attempts to insert a PIVC. Possibly, this is a result of the relationship between fear or anxiety and pain as experienced by the patient, of which it is known that pain levels are higher in patients experiencing fear or anxiety upon an invasive procedure29–31. Successful PIVC placement at the first attempt was mostly seen in patients in whom an 18-gauge sized catheter was used, in comparison to the higher failure ratio in those patients with a 22-gauge PIVC inserted. This can be explained by the fact that a smaller sized PIVC was used in patients with a predicted difficult intravenous access, and thus, in those patients, a failed first attempt at inserting a PIVC could likewise be expected, because of smaller peripheral veins, for instance. Based on these findings, attention must be paid to patients with a high-risk profile according to the A-DIVA scale, and thus to those with a predicted difficult intravenous access, to avoid an unsuccessful attempt.
As stated in the results, male patients had a lower level of pain sensation compared to female patients, although there is no clear and consistent pattern of sex differences in human pain sensitivity32. Despite this, a possible clarification can be that male patients had bigger sized veins and a lower risk profile on the A-DIVA scale against females. It is known that patients with a high ASA physical status are at an increased risk for intraoperative mortality, and the complexity of both the surgical procedure and anesthesia increases simultaneously with an increasing ASA classification33,34. For this reason, larger sized PIVCs were more frequently inserted in this group of patients to achieve faster administration of fluids, which can explain the lower pain scores in patients with a lower ASA physical status.
As stated before, needle-related procedures induce anxiety, fear, and distress in patients due to pain from the intravenous puncture12,13. To reduce this pain, several techniques had been studied in which anaesthetic agents seem to play an important role. The ideal agent for pain upon intravenous cannulation should be effective, quick, pain-free, and cheap and would cause no side effects35. Injected local and topical anaesthetics are most commonly used for analgesic effects36. Topical anaesthetic cream, although effective for smaller cannulas, and adjuvant delivery methods, such as heat, iontophoresis, and ultrasound, have been explored, but are not commonly used12,36. Newer anaesthetic delivery methods, such as use of a pressured aerosolised spray, may be quick and effective but remain costly36. Ethyl chloride and other vapocoolants are likely to have an analgesic effect in reducing pain during intravenous cannulation and are not likely to make cannulation more difficult or cause serious adverse events35. No analgesic techniques were applied in this study, because, first, we proved the baseline level of pain as experienced during intravenous cannulation and identify patient- and procedure-related factors for pain upon inserting a PIVC, and second, because we applied an easy and practical approach without additional techniques. However, combining the results of this study with the most effective and efficient analgesic technique will possibly result in an approach with lower pain scores.
Pain is a subjective experience; every individual uses the word pain based on their own experience with tissue damage37. According to this statement, it seems trivial that pain scores differ between patients, but is present in every intravenous puncture due to a local damage of the tissue. Pain induces a stress response, while the human stress response is innately tied to the immune function through a cascade of hormonal releases driven by the autonomic nervous system38. Increased stress can lead to elevated levels of hormones, which may inhibit immune response and wound healing. Pain and anxiety have also been linked to lowered pain thresholds through increased activation of the entorhinal cortex of the hippocampal formation. Consequently, pain and anxiety can contribute to a number of negative medical outcomes, including longer recovery times15,39,40. As so stated, reducing the level of experienced pain can simply increase a patient’s degree of comfort41.
Limitations
In spite of the large number of patients included in this study, they were not equally distributed among the different study groups. The smaller number of patients included in the 22-gauge and over 18-gauge PIVC groups was not consistent with the number of patients in the 20-gauge and 18-gauge PIVC groups, which can influence the statistical power of the analysis. Hence, attention must be paid to the risk for type I errors. With such a large sample size, it is more likely that the hypothesis test will detect a small difference anyway. For this reason, this study focused on clinically significant results. However, the total cohort of patients included in this study, with respect to their distribution according to the inserted PIVC sizes, was representative of the clinical situation. The dependent practitioner determined the inserted size of the PIVC based on the expected surgical complexity and blood loss and the diameter of the target vein. To increase the level of evidence of research upon the studied subject, controlled trials and blinded studies should be created, while keeping ethical considerations in mind. Nonetheless, our results seem to be of clinical relevance and applicable due to the large population of included patients. The proper choice of the cannulation site can be a simple and effective method of pain reduction upon intravenous cannulation, but further research should focus on validation of the results of this study in combination with the most effective and efficient analgesic technique. We believe that combining analgesic techniques with the anatomical and physiological aspects of a patient can create a more painless cannulation upon PIVC placement. Furthermore, multiple attempts to insert a PIVC increased the pain significantly. Predicting the risk for a difficult intravenous access in the individual patient with the A-DIVA scale can guide the use of additional techniques (such as ultrasound) and, on that account, increase the success ratio of inserting a PIVC. We suggest further research to focus on increasing the success ratio for PIVC placement, in combination with the results on experienced pain during PIVC placement.
CONCLUSION
In summary, inserting a smaller sized PIVC did not result in a lower pain sensation. Nevertheless, the lowest pain score was registered in patients in whom the PIVC was inserted successfully at the first attempt on the dorsum of the hand in male patients with an ASA classification 1 and a low-risk profile on the A-DIVA scale. To prevent pain on inserting a PIVC, an unsuccessful attempt must be avoided, especially in those patients with a predicted high-risk profile on the A-DIVA scale. However, choosing less painful sites will help to gain the confidence and cooperation of the patient. The appropriate size of the PIVC as well as the cannulation site should be carefully selected based on the indication for PIVC placement, the diameter of the vein, and the risk of complications after placement.
ACKNOWLEDGEMENTS
The authors thank the anesthesia personnel for help with the data collection and taking care of patients. FL is the main investigator and involved in study conception and design, drafting of the article, and analysis and interpretation of data. LP and WA helped in collecting data and critical revision of the article. AD participated in critical revision of the article. AB is involved in study conception and design, collecting data, and critical revision of the article.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author(s)
*Fredericus HJ van Loon Department of Research and Education, Catharina Hospital, Eindhoven, The Netherlands Fontys University of Applied Sciences, Eindhoven, The Netherlands Department of Anesthesiology, Pain Medicine and Intensive Care, Catharina Hospital, Michelangelolaan 2 5623 EJ Eindhoven, The Netherlands. Email: rick.v.loon@catharinaziekenhuis.nl Lisette APM Puijn Department of Anesthesiology, Pain Medicine and Intensive Care, Catharina Hospital, Eindhoven, The Netherlands Wesly H van Aarle Department of Anesthesiology, Pain Medicine and Intensive Care, Catharina Hospital, Eindhoven, The Netherlands Angelique TM Dierick-van Daele Department of Research and Education, Catharina Hospital, Eindhoven, The Netherlands Fontys University of Applied Sciences, Eindhoven, The Netherlands Arthur RA Bouwman Department of Anesthesiology, Pain Medicine and Intensive Care, Catharina Hospital, Eindhoven, The Netherlands Department of Signal Processing Systems and Electrical Engineering, Eindhoven University of Technology (TU/e) Eindhoven, The Netherlands *Corresponding author Pages 8-13
References
- Zingg W & Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents 2009; 34(Suppl. 4):S38–S42.
- Rivera AM, Strauss KW, van Zundert AAJ et al. Matching the peripheral intravenous catheter to the individual patient. Acta Anaesthesiol Belg 2007; 58(1):19–25.
- Wilkinson R. Nurses’ concerns about IV therapy and devices. Nurs Stand 1996; 10(35):35–37.
- Rickard CM, Webster J, Wallis MC et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet 2012; 380(9847):1066–1074.
- Lavery I & Smith E. Venepuncture practice and the 2008 Nursing and Midwifery Council Code. Br J Nurs 2008; 17(13):824–828.
- Goudra BG, Galvin E, Singh PM et al. Effect of site selection on pain of intravenous cannula insertion: a prospective randomised study. Indian J Anaesth 2014; 58(6):732–735.
- Scales K. A practical guide to venepuncture and blood sampling. Nurs Stand 2008; 22(29):29–36.
- Gorski LA. The 2016 infusion therapy standards of practice. Home Healthc Now 2017; 35(1):10–18.
- Brown JM. Comparison of pain from insertion of venous cannulae; a volunteer study. Anaesthesia 1998; 53(5):495–496.
- Van Loon FHJ, van Puijn LA, Houterman S et al. Development of the A-DIVA scale: a clinical predictive scale to identify difficult intravenous access in adult patients based on clinical observations. Medicine 2016; 95(16):e3428.
- Fields JM, Piela NE & Ku BS. Association between multiple IV attempts and perceived pain levels in the emergency department. J Vasc Access 2014; 15(6):514–518.
- Lander JA, Weltman BJ & So SS. EMLA and amethocaine for reduction of children’s pain associated with needle insertion. Cochrane Database Syst Rev 2006; 3:CD004236.
- Uman LS, Birnie KA, Noel M et al. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev 2013; 10:CD005179.
- Kennedy RM & Luhmann JD. The “ouchless emergency department.” Getting closer: advances in decreasing distress during painful procedures in the emergency department. Pediatr Clin North Am 1999; 46(6):1215–1247, vii–viii.
- Vaughn F, Wichowski H & Bosworth G. Does preoperative anxiety level predict postoperative pain? AORN J 2007; 85(3):589–604.
- Macario A, Weinger M, Truong P et al. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesth Analg 1999; 88(5):1085–1091.
- Hawker GA, Mian S, Kendzerska T et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res 2011; 63(Suppl. 1):S240–S252.
- Dutt-Gupta J, Bown T & Cyna AM. Effect of communication on pain during intravenous cannulation: a randomized controlled trial. Br J Anaesth 2007; 99(6):871–875.
- Schug SA, Palmer GM, Scott DA et al. Acute pain management: scientific evidence, fourth edition, 2015. Med J Aust 2016; 204:315–317.
- Karanicolas PJ, Farrokhyar F & Bhandari M. Practical tips for surgical research: blinding: who, what, when, why, how? Can J Surg 2010; 53(5):345–348.
- Farrar JT, Young JPJ, LaMoreaux L et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001; 94(2):149–158.
- Faul F, Erdfelder E, Lang A-G et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39(2):175–191.
- Dauch JR, Lindblad CN, Hayes JM et al. Three-dimensional imaging of nociceptive intraepidermal nerve fibers in human skin biopsies. J Vis Exp 2013(74):e50331.
- Frahm KS, Morch CD, Grill WM et al. Activation of peripheral nerve fibers by electrical stimulation in the sole of the foot. BMC Neurosci 2013; 14:116.
- Wallis MC, McGrail M, Webster J et al. Risk factors for peripheral intravenous catheter failure: a multivariate analysis of data from a randomized controlled trial. Infect Control Hosp Epidemiol 2014; 35(1):63–68.
- Bregenzer T, Conen D, Sakmann P et al. Is routine replacement of peripheral intravenous catheters necessary? Arch Intern Med 1998; 158(2):151–156.
- Do Rego Furtado LC. Maintenance of peripheral venous access and its impact on the development of phlebitis: a survey of 186 catheters in a general surgery department in Portugal. J Infus Nurs 2011; 34(6):382–390.
- Dychter SS, Gold DA, Carson D et al. Intravenous therapy: a review of complications and economic considerations of peripheral access. J Infus Nurs 2012; 35(2):84–91.
- Williams AE & Rhudy JL. The influence of conditioned fear on human pain thresholds: does preparedness play a role? J Pain 2007; 8(7):598–606.
- Hoeger Bement M, Weyer A, Keller M et al. Anxiety and stress can predict pain perception following a cognitive stress. Physiol Behav 2010; 101(1):87–92.
- Rhudy JL & Meagher MW. Fear and anxiety: divergent effects on human pain thresholds. Pain 2000; 84(1):65–75.
- Racine M, Tousignant-Laflamme Y, Kloda LA et al. A systematic literature review of 10 years of research on sex/gender and experimental pain perception — part 1: are there really differences between women and men? Pain 2012; 153(3):602–618.
- Menke H, Klein A, John KD et al. Predictive value of ASA classification for the assessment of the perioperative risk. Int Surg 1993; 78(3):266–270.
- Visnjevac O, Davari-Farid S, Lee J, et al. The effect of add-ing functional classification to ASA status for predicting 30-day mortality. Anesth Analg 2015; 121(1): 110–116.
- Griffith RJ, Jordan V, Herd D, et al. Vapocoolants (cold spray) for pain treatment during intravenous cannulation. Cochrane Database Syst Rev 2016; 4: CD009484.
- Zempsky WT. Pharmacologic approaches for reducing venous access pain in children. Pediatrics 2008; 122 (Suppl. 3): S140–S153.
- Merskey H. The taxonomy of pain. Med Clin North Am 2007; 91(1): 13–20,vii.
- Padgett DA and Glaser R. How stress influences the immune response. Trends Immunol 2003; 24(8): 444–448.
- Ploghaus A, Narain C, Beckmann CF, et al. Exacerbation of pain by anxiety is associated with activity in a hippocampal network. J Neurosci 2001; 21(24): 9896–9903.
- Jamison RN, Parris WC and Maxson WS. Psychological factors influencing recovery from outpatient surgery. Behav Res Ther 1987; 25(1): 31–37.
- Morse JM, Bottorff JL and Hutchinson S. The paradox of comfort. Nurs Res 1995; 44(1): 14–19.
