Volume 7 Issue 1
Peripheral venous access using the Seldinger wire technique and short cannulas in patients with difficult venous access: a case series
Brendan Smith-Hanratty
Keywords cannulation, intravenous, difficult vascular access, DIVA, DIV, peripheral intravenous cannulation, Seldinger, short peripheral, leadercath
For referencing Smith-Hanratty B. Peripheral venous access using the Seldinger wire technique and short cannulas in patients with difficult venous access: a case series. Vascular Access 2021; 7(1):12-15.
DOI https://doi.org/10.33235/va.7.1.12-15
Abstract
Patients with ‘difficult’ vascular access often experience delays in care, multiple attempts at obtaining vascular access, and more frequent central line insertions due to inability to obtain peripheral access. Intravenous (IV) cannulation using ultrasound and a Seldinger approach is an established method of obtaining reliable IV access when standard approaches fail in this patient group; however, the majority of the literature focuses on ‘long peripheral’ or midline catheters. While these studies demonstrate excellent results, these devices are not always available and specific training in their use is often required, limiting the use of this technique.
This article describes the use of short Seldinger-style catheters (such as those often used for arterial lines) for ultrasound-guided peripheral venous access and reports on a series of five patients who underwent this procedure. First pass success rates were 100%, there were no complications, and catheter survival was above average with no premature catheter failures. Patient satisfaction with this procedure was also high, finding it preferable to the alternatives – multiple failed attempts at peripheral cannulation, frequent cannula failures, midline, or even central line insertion.
This case series demonstrates that, despite the known advantages of longer cannulas, shorter or standard length Seldinger inserted devices are also an effective solution for short-term vascular access, provided the target vessel is <1cm deep at point of insertion. These devices are ubiquitous in critical care and emergency settings for use in arterial cannulation and therefore this opens up this vascular access technique to any clinician trained in insertion of an arterial catheter.
Introduction
Obtaining vascular access can often be challenging, particularly when patients have been in hospital for extended periods of time, have had multiple venepunctures and cannulations, are obese, dehydrated, critically ill, or have a history of chemotherapy or intravenous (IV) drug use.1,2 Patients with difficult vascular access often undergo multiple, repeated attempts at obtaining peripheral vascular access, experience delays in care,3 and not infrequently undergo central line or intraosseous needle insertion, when peripheral access is not possible,1,4–7 which carry higher risks of procedural complication8 and infection than peripheral access.9 Vascular access using the traditional catheter over needle approach can often be challenging in patients with difficult access using traditional methods (defined as blind insertion using touch and feel, without vein‐locating technology).10
Ultrasound guidance provides a huge advantage here in terms of locating deeper, or non-palpable veins,11 but accessing these veins can still be a challenge; once the needle tip enters the vessel and flashback of blood is seen, the catheter and needle assembly must be advanced slightly further to ensure that the tip of the catheter is within the vessel before it is advanced over the needle. This can be difficult when attempting to access deep or very small veins, even with the ultrasound in long access view where the tip of the needle can be seen within the vessel lumen, and is a common point of failure.
Utilising a Seldinger wire device has been shown to be an effective way of negating this problem and obtaining venous access where traditional methods have failed5 as once flashback of blood is seen in the finder needle the guide wire can be inserted immediately without further manipulation of the needle. Harvey and Cave12 and Stone4 described an approach to venous cannulation using catheter over needle devices with integral short guidewires (a modified or simplified Seldinger method), which goes some way towards rectifying this problem. However, flashback of blood is often delayed by the presence of the wire within the lumen.
The other major issue in ultrasound-guided cannulation is that of catheter length accessing deeper vessels resulting in less catheter in vein when standard 30–40mm length catheters are used and, therefore, an increased premature failure rate.13 To overcome this issue there has been growing interest in the use of ‘long peripheral’ and midline catheters (of generally between 8–16cm length), particularly for ultrasound-guided cannulation,7,14 and while this literature demonstrates excellent results in terms of both complication rates and catheter survivability, it is not always an appropriate or available solution. There is not always a suitable vessel to accommodate these longer catheters, it may be preferable to avoid these veins in cases of local trauma or infection, or it may be preferable to preserve these vessels for a planned central line insertion or vascular procedure at a later date.10
In addition, these longer devices are not commonly available in all clinical areas, are often significantly more expensive, and often require specific training; therefore, it is not always possible to access this equipment, or a clinician trained in its use, in a timely manner. There may also be policy and procedural or logistical reasons that prevent insertion of a central venous device in general ward areas. Short peripheral Seldinger catheters, on the other hand, are commonly used for arterial cannulation in emergency departments and critical care areas and many clinicians are familiar with their use.
What this paper adds
This article describes a series of five patients who underwent peripheral IV cannulation using these short/standard Seldinger-style catheters, and demonstrates that they can be used for IV access without risking an increased rate of premature failure or complication in vessels <1cm deep and that longer catheters are not always required. This is a useful option for short-term IV access when a longer catheter or extended dwell device such as a peripherally inserted central catheter (PICC) or midline is either not appropriate or not available. The wider use of this method has the potential to improve the management of patients with difficult venous access.
Method
This report describes a method of obtaining peripheral venous access using ultrasound guidance and short Seldinger wire catheters (Leadercath, 20g, 40mm Vygon, Ecouen, France) typically used for arterial access but designed for use in a range of venous and arterial applications. Ethics approval was not required per the institution’s ethics committee regulations, but written consent to use patient records for publication was; this was gained at the time of performing the procedure. All patients were aged between 30–85 years old and were considered to have ‘difficult vascular access’, having either had at least two failed attempts at access on that occasion using the standard method by an experienced provider, no easily palpable peripheral veins in the upper limbs, a history of requiring ultrasound-guided cannulation, multiple failed attempts, or previous central line placement due to difficulty obtaining peripheral access. All were either inpatients on the general medical ward or the emergency department of a regional hospital in NSW Australia. Each catheter was followed up daily until removal and was monitored for development of phlebitis by nursing staff at least three times a day using a standardised assessment tool (VIP score).15
To perform the procedure, a tourniquet was applied to the upper arm and the skin cleaned with chlorhexidine 2%/alcohol 70% as per facility policy for IV cannulation. Sterile gloves were worn and a sterile fenestrated drape used. An appropriate site was located using ultrasound (sterile probe cover and transmission gel). The vessel was assessed for patency by simply checking for compressibility in transverse axis view, at the insertion point and for 2–3cm proximal to this point. Vessels over 1cm deep will result in <65% of the catheter residing in the vein (assuming a 40mm catheter and relatively steep 45 degree insertion angle) and, therefore, will be prone to premature failure.13 In this situation, either an alternative site or a longer catheter should be used.
Once a suitable site was located, the needle was inserted under ultrasound guidance. When blood flow was seen at the needle hub, the guide wire was inserted without any further repositioning of the needle, the needle was then removed, and the catheter was inserted over the wire. Once the catheter was inserted into the hub, the wire was removed and a bung or extension set applied. To prevent dislodgement, it is important to remove all transmission gel and ensure the skin is dry before the dressing is applied.
Results
Table 1 below shows a series of five consecutive patients who were cannulated using this method. All attempts were successful on the first pass, all lines were inserted at or distal to the antecubital fossa (thus preserving the vessels of the upper arm for any potential PICC insertion), and remained in situ for between 1 and 4 days. There were no complications reported, no device failed prematurely, and all remained functional and in place for the duration of IV therapy, although one was removed and resited on Day 4 as institution policy currently prohibits peripheral intravenous catheters (PIVCs) from remaining in place longer than this. As per usual care, each shift nursing staff assessed cannula sites for phlebitis or other complications, using the VIP (visual infusion phlebitis) score15; there were no reports of a VIP score of greater than 0 (indicating no evidence of phlebitis).
Table 1. Details of each procedure in case series
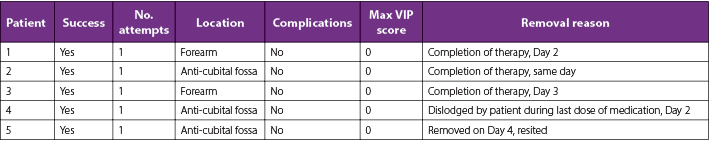
Patients found this procedure to be easily tolerated, usually taking under 10 minutes from set up to completion, and they reported that it was significantly less painful and faster than cannulation via standard methods. One patient reported a clinician ‘digging around for an hour’ in order to obtain access, which failed in less than 4 hours, whereas Leadercath insertion took minutes and remained functional for a number of days. Most patients felt they would have liked to be cannulated using this method from the outset rather than waiting until they had had multiple failed attempts
Discussion and conclusions
Although the numbers in this series are low, it demonstrates that short Seldinger cannulas are an effective short-term vascular access solution in patients with difficult vascular access; indeed, 100% patients were cannulated on the first attempt and all cannulas remained functional for the duration of therapy without complication, occlusion, phlebitis, or extravasation, which is well above average for this patient group. Dargin and colleagues16 report a premature failure rate of 50% with a median survival of only 26 hours for standard length ultrasound-guided cannulas in difficult access patients.
The results of this series indicate that wider use of these devices, which are commonly available in emergency departments and critical care areas, for IV access may help avoid repeated cannulation, multiple failed attempts, iatrogenic complications stemming from failed attempts, delays in care, and some midline or central line insertions, all of which lead to better vessel health and preservation and an improved patient experience for this patient group.
While the author acknowledges that in many cases it is difficult to predict the required duration of IV therapy, it is worth noting that 80% of patients in this series completed IV therapy within 4 days, a duration of therapy that generally would not warrant a central line or extended dwell device such as a midline or PICC, which, had this short Seldinger catheter not been an option, likely would have been the only alternatives, and would be associated with huge increase in both potential risk to the patient and cost to the health service.
This procedure warrants further discussion and investigation with a larger trial comparing this approach to ultrasound-guided cannulation with standard short peripheral cannulas, and perhaps including exploration of other commercially available similar products. The Vygon Leadercath was used for this series; however, the author sees no reason that other similar products would not produce similar results. Disadvantages of this device are that the 20g Leadercath is not power injectable, therefore unsuitable for some CT contrast injections, shorter catheters are limited to vessels <1cm deep and, while cheaper than a central line or midline, is still significantly more expensive than a standard peripheral IV cannula.
About the author
Brendan Smith-Hanratty, Dip HE N, BSc (Hons) N, PgCert Global Heath, PgCert Clin Prac, is a clinical nurse educator working in a medical/surgical and close observation unit at the Blue Mountains District ANZAC Memorial Hospital in Katoomba NSW, Australia. He has a certificate in allied health performed ultrasound vascular access, and is currently studying for a MScN(NP) at the University of Sydney NSW, Australia.
Conflict of interest
The author declares no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author(s)
Brendan Smith-Hanratty
Medical/Surgical and Close Observation Unit, Blue Mountains District ANZAC Memorial Hospital, Katoomba NSW, Australia
For correspondence Brendan.Smithhanratty@health.nsw.gov.au or Brendanhanratty@hotmail.co.uk
References
- Leidel BA, Kirchhoff C, Bogner V, Stegmaier J, Mutschler W, Kanz K-G, et al. Is the intraosseous access route fast and efficacious compared to conventional central venous catheterization in adult patients under resuscitation in the emergency department? A prospective observational pilot study. Patient Saf Surg. 2009;3(1):24–.
- Piredda M, Fiorini J, Facchinetti G, Biagioli V, Marchetti A, Conti F, et al. Risk factors for a difficult intravenous access: a multicentre study comparing nurses’ beliefs to evidence. J Clin Nurs. 2019;28(19–20):3492–504.
- Witting MD. IV access difficulty: incidence and delays in an urban emergency department. J Emerg Med. 2012;42(4):483–7.
- Stone Bradley A, M.D. Ultrasound guidance for peripheral venous access: a simplified Seldinger technique. Anesthesiology. 2007;106(1):195–.
- Meyer P, Cronier P, Rousseau H, Vicaut E, Choukroun G, Chergui K, et al. Difficult peripheral venous access: clinical evaluation of a catheter inserted with the Seldinger method under ultrasound guidance. J Crit Care. 2014;29(5):823–7.
- Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81(9):1159–71.
- Fabiani A, Dreas L, Sanson G. Ultrasound-guided deep-arm veins insertion of long peripheral catheters in patients with difficult venous access after cardiac surgery. Heart Lung. 2017;46(1):46–53.
- Kornbau C, Lee KC, Hughes GD, Firstenberg MS. Central line complications. Int J Crit Illn Inj Sci. 2015;5(3):170–8.
- Mermel LA. Short-term peripheral venous catheter-related bloodstream infections: a systematic review. Clin Infect Dis. 2017;65(10):1757–62.
- Fiorini J, Venturini G, Conti F, Funaro E, Caruso R, Kangasniemi M, et al. Vessel health and preservation: an integrative review. J Clin Nurs. 2019;28(7–8):1039–49.
- Paladini A, Chiaretti A, Sellasie KW, Pittiruti M, Vento G. Ultrasound-guided placement of long peripheral cannulas in children over the age of 10 years admitted to the emergency department: a pilot study. BMJ Paediatr Open. 2018;2(1):e000244-e.
- Harvey M, Cave G. Ultrasound-guided peripheral venous cannulation using the Seldinger technique. Emerg Med J. 2011;28(4):338.
- Pandurangadu AV, Tucker J, Brackney AR, Bahl A. Ultrasound-guided intravenous catheter survival impacted by amount of catheter residing in the vein. Emerg Med J. 2018;35(9):550.
- Qin KR, Ensor N, Barnes R, Englin A, Nataraja RM, Pacilli M. Long peripheral catheters for intravenous access in adults and children: a systematic review of the literature. J Vasc Access. 2020:1129729820927272.
- Gallant P, Schultz AA. Evaluation of a visual infusion phlebitis scale for determining appropriate discontinuation of peripheral intravenous catheters. J Infus Nurs. 2006;29(6):338–45.
- Dargin JM, Rebholz CM, Lowenstein RA, Mitchell PM, Feldman JA. Ultrasonography-guided peripheral intravenous catheter survival in ED patients with difficult access. Am J Emerg Med. 2010;28(1):1–7.
