Volume 39 Number 1
Validation and inter-rater reliability of inexpensive, mini, no-touch infrared surface thermometry devices as an assessment tool for prediction of wound-related deep and surrounding infection
Hiske Smart, Eman Al Jahmi, Ebrahim Buhiji and Sally-Anne Smart
For referencing Smart H et al. Validation and inter-rater reliability of inexpensive, mini, no-touch infrared surface thermometry devices as an assessment tool for prediction of wound-related deep and surrounding infection. WCET® Journal 2019; 39(1):18-22
DOI https://doi.org/10.33235/wcet.39.1.18-22
Abstract
Industrial infrared thermometry devices are large and, despite being less expensive than the current gold standard Exergen Dermatemp medical infrared thermometer, are still not affordable enough to ensure unrestricted and consistent use of this assessment modality in regular wound-related day-to-day practice. An increased skin surface temperature differentiation of 3°F associated with a wound has a positive predictive ability to detect deep or surrounding wound infection. This study hypothesised that inexpensive, pen- or pocket-sized, no-touch surface infrared thermometry devices will be equal in ability to detect a 3oF increased skin temperature compared to the Exergen Dermatemp infrared device and be reliable in the hands of any wound assessor. The odds of the control and other thermometers to detect a 3oF temperature difference, irrespective of the raters, were achieved in all five of the mini thermometers tested, with a correct temperature difference prediction that occurred in 90.933% of the times (odds determined 9/10). As a result of this study mini, no-touch infrared thermometry, to detect a 3oF temperature difference in wound assessment to determine tendency, could be implemented into primary health care clinics, rural clinics, day-to-day hospital practice and standard outpatients departments at a small financial cost, regardless of which thermometer is put to use.
Introduction
The use of no-touch infrared surface thermometry is validated in the assessment of wounds to determine the status of bacterial burden and a subsequent provoked host response, by determining an increased 3 degree Fahrenheit (3°F) surface difference when measured against an opposing limb or body area, as determined by Fierheller1. Medical-grade infrared surface thermometry devices are large and expensive, putting routine use of this assessment modality into advanced wound care units only and out of reach for clinicians in everyday practice. A recent study by Mufti, Coutts and Sibbald2 has validated the use of industrial hand-held surface infra-red thermometers against the current gold standard Exergen Dermatemp device. Industrial devices are large and, despite being less expensive than this medical infrared thermometer, are still not affordable enough to ensure unrestricted and consistent use of this assessment modality in regular wound-related day-to-day practice. In validating inexpensive, pen- or pocket-sized, no-touch infrared devices, this modality can be made accessible to any clinician (interprofessional) dealing with wounds on a regular basis, without compromising on infection control measures.
Background
The challenge to clinicians in a subgroup of patients with an impaired inflammatory response is that clinical markers of localised infection (redness, swelling, exudate, lack of movement, pain, heat), present only when the infection is already overwhelming the patient’s host response3,4. In the validation study to determine superficial and deep tissue infection markers for the chronic wound5, the highest significance to detect deep tissue infection, was achieved by identifying an increased skin surface temperature differentiation of 3°F. This marker achieved an eight times more likely predictive ability to detect deep tissue infection than any other marker in the STONEES© criteria set (size increased, temperature difference, Os probing to bone, new breakdown and necrotic tissue, erythema flare, exudate or smell)5.
The temperature differentiation is done by obtaining the highest skin surface temperature reading, 1cm away from the skin in a perpendicular position, measured on the wound edge. That reading is then compared to a reading taken in the same manner on a similar area of an opposing limb or skin area1. This method establishes a temperature difference tendency. The increased surface temperature obtained, with two additional other criteria added from the STONEES© set is validated to be predictive of deep or surrounding wound infection5 opposed to critical colonisation6.
In validating the least costly and most readily available skin surface thermometry devices against the Exergen Dermatemp in a similar design to Mufti et al.2, the quick assessment ability of wound-related deep tissue infection can be made available to all clinicians, regardless of resource restrictions that may apply to certain clinical environments.
It is important to note that infrared skin surface measurement is different from physiological infrared measurement used to detect fever, which in adults7 is less reliable than in the paediatric population8. Infrared surface thermometry is done without a physiological conversion factor built into the modality; it is utilised in engineering, electromechanical environments and the building industry and has been well-researched since the early 1960s. Currently industrial research is focussed on nuclear reactor safety9, operational machine surface temperatures and critical deviations as part of safety measures.
The clinical grade Exergen Dermatemp infrared surface thermometer is sold at a price that ranges from US$700 to US$900 (BD 265–340) per piece. The industrial thermometers tested by Mufti et al.2 ranged from US$80to US$100 (BD 30–37) per piece. The devices used in this study cost no more than US$20 (BD 7.5), with three devices priced at US$10 or less (BD 3.6). Due to the cost of one Exergen Dermatemp, clinicians have overlooked their ability to ensure fast and efficient wound assessment for identification of wound surface bacterial burden reaction. By having access to a more affordable modality, timely intervention can be quicker to prevent wound deterioration due to a deep wound infection being identified too late.
Method, design and sampling
Hypothesis
Inexpensive, mini (pen- or pocket-sized), no-touch surface infrared thermometry devices are equal in ability to detect a 3°F increased skin temperature compared to the gold standard Exergen Dermatemp infrared device.
Objectives of the study
- To compare five inexpensive no-touch surface infrared thermometers (Mastercraft 0574568-4, Infrared 68199, Infrared EM512, Infrared DT8220 and Infrared H10140 with a distance to spot ratio of 1:1 or more) against the Exergen Dermatemp clinical infrared surface thermometer (distance to spot ratio 1:1).
- To determine the precision of measurement of the inexpensive, pen- or pocket-sized, no-touch surface infrared thermometry devices compared to the skin temperature obtained by the Exergen Dermatemp device. (This would predict if the inexpensive devices are similar to the Exergen Dermatemp in measurement).
- To determine the accuracy of inexpensive, pen- or pocket-sized, no-touch surface infrared thermometry devices in detecting a 3°F increased skin temperature compared to the Exergen Dermatemp device. (This would predict if the difference detected by the Exergen Dermatemp can be detected by the inexpensive devices as well).
- To determine the inter-rater reliability of professionals using this modality by measuring consistency of temperature difference obtained by three investigators. (This would predict the chance/odds of any clinician to obtain a correct assessment compared to the control).
The study took place in the hyperbaric and wound care unit of King Hamad University Hospital, in the Kingdom of Bahrain, where the use of no-touch infrared skin surface thermometry is a standard assessment modality with every dressing change procedure. This was a prospective cross-sectional study that included all consecutive consenting patients with either a new wound or an existing wound treated as part of the patient load of this unit for a period of one month. Three clinicians were doing six measurements (one control and five test devices) per patient at the same time. They followed one after the other, after the hot spot and contra-lateral spot was identified by rater 1, who is the clinical specialist of the unit. The two other raters were a doctor and a registered nurse, both working in the wound care unit.
Study sample inclusion and exclusion criteria
Inclusion: All patients with a wound who attend for a regular dressing change at the unit were eligible for a once-only inclusion into this study.
Exclusion: Patients who were unable due to their condition or unwilling due to time constraints to give signed informed consent for five added measurements being done apart from the standard Exergen Dermatemp infrared reading that is mandatory for every visit. Patients who were already assessed with the five devices compared to the Exergen Dermatemp and already included in the study.
Design and sample size
The sample size reached 100 patients with 300 thermometer readings obtained for each device and 1800 thermometer measurements done in total.
Data Collection methods, instruments used and measurements
Patients who have given signed and informed consent had all previous dressing materials removed and all exudate wiped clean from the wound bed with all standard wound care procedural preparations in place as per standard dressing change protocol.
Data collection procedure
- The Dermatemp measurement was done on the wound edge in Fahrenheit before any cleansing of the wound bed occurs to prevent cooling down of the wound edges due to the cleansing fluid. The highest reading obtained by the first rater at the wound edge on intact skin served as the test reading and was recorded on the data collection sheet. The warmest spot was marked on the skin with a small dot from an operating room pen.
- The reading on the exact mirror image side of the limb or body part was taken as reading two, recorded as reading opposing limb and was marked with a small dot to determine the temperature differentiation.
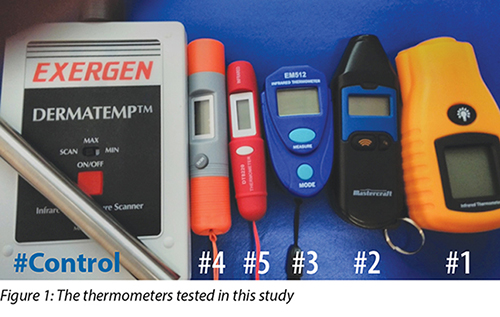
- All five of the small devices marked 1–5 were set to measure surface temperature in Fahrenheit and were then respectively used in the order 1–5, with the first measurement on dot 1 and second reading on dot 2 for each thermometer. Each temperature reading recorded in the same manner as for the Exergen Dermatemp on the data collection sheet until readings from all six devices were collected for one patient (see Figure 1).
- In order to determine inter-rater reliability and inter-professional variations, this procedure was then to be repeated two times more times to include three testers (two RNs, one MD) who stayed consistent for the duration of the study.
- Added data on the collection sheet was patient gender, age, diagnosis and any important adverse factors affecting healing for later analysis.
Results
The help of a statistician was acquired for data analysis as more than one statistical method was needed to determine the fine variations of both the devices and the inter-rater reliability testing.
Comparison of infrared thermometers
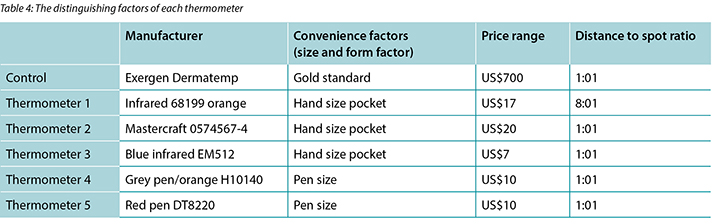
When the raw temperature measurement variation observed by each thermometer was compared to each other using a paired T-test (test to determine whether mean values are significantly different from one another) the p-values observed showed some deviation (depicted in Table 1).
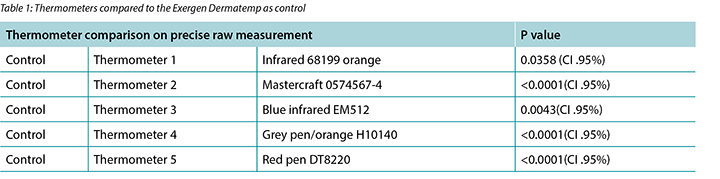
With each of these five T-tests, the null hypothesis (that the measurement of the control is not significantly different from any other thermometer) is rejected in thermometers 2, 4 and 5 at a 95% significance level. Thus, we can conclude that in absolute precision there was deviation and significant variation in the exact performance of these thermometers.
As the assessment of elevated skin temperature to determine deep and surrounding infection forms part of a bundle (NERDS© and STONEES©)5, the aim of infrared thermometry is to determine a greater than 3°F difference to have a positive test result. Therefore, the thermometers tested do not have to reproduce the exact raw temperature value compared to the control, but should definitely be able detect a temperature difference of 3°F to make it a viable measurement modality in a clinical practice setting. That was the next test done on this dataset.
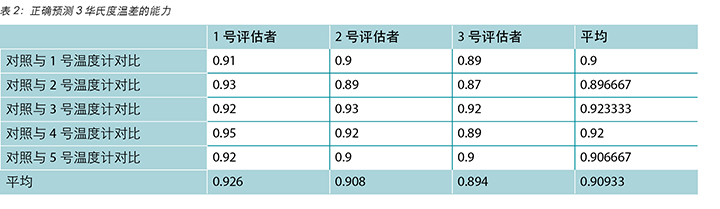
The odds of the control and other thermometers to detect a 3°F temperature difference (either both >=3 or both<3) for each of the respective raters is depicted in Table 2. The finding was that, irrespective of the raters, all five of the mini thermometers were able to make the correct call to detect a 3°F temperature difference in 90.933% of the times, giving it a success odd of 9/10.
Interpretability of thermometers
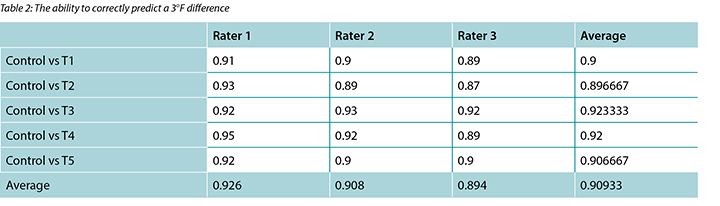
Paired T-tests were performed to determine whether there were statistically significant differences in the averages achieved by the three raters (test to determine whether mean values are significantly different from one another) as depicted in Table 3. The p-values were recorded in the table and had to be more than 0.05 to show consistency and similarity.
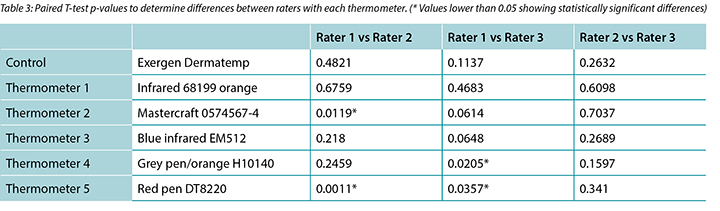
In the control measurement and each of the measurements of thermometers 1 and 3, there were no statistically significant differences detected in the mean observed by the three raters. There were statistically significant differences in the measurements from thermometer 2 (rater 1 and 2), thermometer 4 (rater 1 and 3) and thermometer 5 (rater 1 and 2; rater 1 and 3).
The best performing thermometers, in relation to the Exergen Dermatemp, were thermometers 1 and 3 with performance that was consistent irrespective of the user. Variations based on the user were, however, observed for thermometers 2, 4 and 5 shown in p-values lower than 0.05.
Discussion
The high odds of the mini infrared thermometer devices to detect a 3°F temperature difference and the level of inter-rater reliability achieved to determine that difference in this study opens more clinical options to incorporate this modality into standard wound care practice for comprehensive wound assessment. With minimal teaching given to the raters, apart from reading the brochure of the device, our raters could achieve a clinically correct thermometry assessment compared to the gold standard device 9 out of 10 times.
Of the mini devices tested (Table 4) there were two that were more consistent between users and compared very favourably to the control thermometer value, both on raw temperature measurement precision and 3°F prediction ability. Thermometer 1 had a distance to spot range of 8:1 (best as well for infection control maintenance) that could have added in the precision of measurement and a very comfortable hand grip that had added to stability. Thermometer 3, despite having a distance to spot ratio of 1:1, had performed consistently as well. Despite being small and compact, it fitted the hand of the clinician snugly that added to device stability when aiming to obtain the measurement. Both of these devices also had legible numerical displays for easy reading of a value from a distance.
The pen-type thermometers all had a distance to spot ratio of 1:1, had the largest deviations between raters and highest error factor on precision. These devices have very small display screens that made it difficult to read accurately from a distance. Most of the mini devices used button batteries that added to cost over the longer term as the life time of the batteries was limited and depleted by the end of the study.
When it came down to accuracy in the ability to detect a 3°F temperature difference, all of the thermometers as well as all of the raters could achieve that 90.9% of the time (odds 9/10). These cost-conscious, mini infrared devices could be used to start to bridge a gap in practice and empower the clinician in resource-restrained environments to also be able to utilise non-invasive surface thermometry in assessment for the presence of deep and surrounding wound infection. This would substitute the subjective assessment of clinicians who are using the back of their hand as a touch indicator on patient skin to detect temperature differences10, by providing a quantifiable and comparable alternative.
Conclusion
Mini, no-touch infrared thermometers could be used to detect a 3°F temperature difference to add in comprehensive wound assessment, regardless of which device is chosen. There is a high reliability that the clinician will detect that difference with 90.9% accuracy each time, regardless of which mini infrared device is used.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
廉价微型非接触式红外线表面温度测量仪用于预测伤口深层和周围感染评估时的有效性和评估者间可信度
Hiske Smart, Eman Al Jahmi, Ebrahim Buhiji and Sally-Anne Smart
DOI: https://doi.org/10.33235/wcet.39.1.18-22
摘要
工业用红外线温度测量仪的体积比较大,尽管比目前的黄金标准Exergen Dermatemp医用红外线温度计便宜,但价格仍然不够低,无法在常规伤口日常护理中无限制和持续地使用。伤口皮肤表面温度检测出3华氏度的升高,则代表检测伤口深层或周围感染的阳性预测能力。本研究假设,平价笔式或袖珍非接触式红外线表面温度测量仪与Exergen Dermatemp医用红外线温度计一样,也可以检测皮肤温度升高3华氏度,可以可靠地由任何伤口评估人员使用。无论由谁评估,所测试的全部五种微型温度计中,对照温度计和其他温度计均可以检测皮肤温度升高3华氏度,正确预测温度差的几率达到90.933%(几率为9/10)。本研究的结果是,微型非接触式红外线温度测量仪可以在伤口评估时检测出3华氏度的温差,以确定温度趋势,因此可以以较低经济成本应用于初级医疗诊所、乡村诊所、医院日常实践和普通门诊科,无论使用哪种温度计。
前言
通过确定在测量对侧肢体或身体部位时表面温度增加3华氏度(3°F),如由Fierheller所确定,在伤口评估中采用非接触式红外线温度测量仪以检测细菌负荷状态和随后引起的宿主反应已得到验证。1医用红外线表面温度测量仪的体积较大而且价格昂贵,这种评估方法只能在高级伤口护理科室常规使用,无法在临床人员的日常工作中使用。Mufti、Coutts和Sibbald2最近开展了一项研究,通过与目前的黄金标准Exergen Dermatemp装置比较,验证了工业用手持式红外线表面温度测量仪的有效性。工业用装置的体积比较大,尽管比此医用红外线温度计便宜,但价格仍然不够低,无法在常规伤口日常护理中无限制和持续地使用。经验证,这种平价笔式或袖珍非接触红外线装置可供所有临床人员(跨专业)在常规性处理伤口时使用,不会影响感染控制措施。
背景
临床人员在治疗一组有炎症反应受损的患者时面临的挑战是,局部感染的临床标志物(红肿、渗出、无法移动、疼痛、温热)只有在感染已经超出患者宿主反应时才会出现3,4。在此项旨在确定慢性伤口的表浅和深层组织感染标志物的验证研究中5,能够检测到皮肤表面温度升高3华氏度对于检测深层组织感染具有最重要意义。此标志物检测对深层组织感染的预测能力比STONEES©标准组合(体积增加、温差、骨髓炎骨探查、新分解和坏死组织、红斑复发、渗出或异味)中的任何标志物高八倍5。
测量温差时,在距离伤口边缘垂直位置1厘米处测量皮肤表面最高温度。将此测量值与采取相同方法在对侧肢体的类似部位或皮肤部位的测量值相比较1。此方法可以确定温差趋势。通过与临界定植比较验证,测量到的表面温度升高6,连同来自STONEES©标准组合的另外两项标准,证实可以预测深层或周围感染5。
本研究采用与Mufti等人2的设计类似的设计,通过与Exergen Dermatemp装置比较来验证最廉价和最容易获得的皮肤表面温度测量仪。研究表明,所有临床人员都可以采用这种方法快速评估伤口深层感染,无论某些临床环境中资源是否有限。
需要注意的一点是,红外线皮肤表面测量与用于检测发烧的生理学红外线测量不同,后者在成人人群7中的可靠性不如儿童人群8。红外线表面温度测量未采用本方法自带的生理学转换因子,它被用于工程、机电环境和建筑行业,自上世纪60年代以来已经被充分研究。目前的工业研究侧重于核反应堆安全性9,运行时机器表面温度和临界偏差均属于安全性监测指标。
医用Exergen Dermatemp红外线表面温度测量仪的售价为每件700至900美元。Mufti等人2测试的工业用温度计的售价为每件80至100美元。本研究使用的装置售价不超过20美元,其中三件装置的售价不超过10美元。考虑到Exergen Dermatemp装置的成本,临床人员忽视了他们能够通过快速有效地进行伤口评估检测伤口表面细菌负荷反应。如果有一种更平价的方法,就可以更快地及时实施干预,防止由于未及时发现伤口深层感染而造成的伤口
恶化。
方法、设计和采样
假设
平价微型(笔式或袖珍)非接触式红外线表面温度测量装置与黄金标准Exergen Dermatemp红外线装置一样,都有相同的能力检测皮肤温度升高3华氏度。
研究目的
- 将五种平价非接触式红外线表面温度计(Mastercraft 0574568-4、 Infrared 68199、Infrared EM512、Infrared DT8220和Infrared H10140,测量距离与测量点大小之比为1:1或以上)与Exergen Dermatemp临床红外线表面温度计(测量距离与测量点大小之比为1:1)比较。
- 通过与黄金标准Exergen Dermatemp装置测量的皮肤温度比较,确定平价笔式或袖珍非接触式红外线表面温度测量装置的测量精确度。(这可以预测这些平价装置与Exergen Dermatemp装置的测量结果相似)。
- 通过与黄金标准Exergen Dermatemp装置比较,确定平价笔式或袖珍非接触式红外线表面温度测量装置在检测皮肤温度升高3华氏度时的准确度。(这可以预测这些平价装置检测到的温差是否与Exergen Dermatemp装置检测到的温差一致)。
- 由三位研究人员采用此方法测量温差,通过查看温差的一致性来确定专业评估者间的可信度。(通过与对照比较,这可以预测临床人员获得正确评估的几率)。
本研究在巴林王国哈迈德国王大学医院高压氧和伤口护理科进行。采用非接触式红外线皮肤表面温度测量仪是该科室每次更换敷料时的标准评估方法。这是一项前瞻性横向研究,包括的患者为该科室一个月内的连续患者,所有患者均提供同意书,有新伤口或既有伤口。每位患者由三位临床人员在同一时间完成六次测量(一次为对照装置和五次为受测装置)。第一位评估者为该科室的临床专家,由其确定待测量的热点和对侧点后,三位评估者一个接一个地完成测量。另外两位评估者中,一位是医生,另外一位是注册护士,均在伤口护理科工作。
研究样本的纳入和排除标准
纳入标准:前来本科室定期更换伤口敷料的所有带伤口的患者都可以参加本研究,但只能参加一次。
排除标准:除了每次就诊必须接受的标准Exergen Dermatemp装置测量之外,由于病情不能或由于时间限制不愿意提供知情同意书以便接受额外五次测量的患者。已经纳入在本研究中,并且已经采用五种装置评估以便与Exergen Dermatemp装置比较的患者。
设计与样本量
样本量已达100位患者,每个装置获得300次温度测量,总共完成1800次温度测量。
数据采集方法、使用的仪器和测量
在患者已经签字并提供知情同意书后,根据标准的敷料更换方案,遵循所有标准的伤口护理操作注意事项,患者的所有既往敷料都被拆除,伤口床的所有渗出物都被擦净。
数据采集程序
- 在清理伤口床之前,采用Dermatemp装置以华氏温度测量伤口边缘温度,以免清洗液造成伤口边缘温度下降。第一位评估者在完整皮肤的伤口边缘获得的最高测量值作为测试测量值,记录在数据采集表中。用手术室笔在皮肤上画一个小点,标记温度最高的热点。
- 在对应的对侧肢体或身体部位上获得的测量值为第二测量值,记录为对侧肢体测量值,用一个小点标记,以便确定温差。
- 全部五个小型测量装置分别被标记为1至5号,设定成以华氏温度测量表面温度,然后分别按1至5的顺序使用,每个温度计的第一个测量值在第一个点上,第二测量值在第二个点上。在数据采集表上记录每个温度测量值,记录方式同 Exergen Dermatemp装置,直至为每位患者使用所有六个装置采集测量值(见图1)。

- 为确定评估者之间的可信度和专业人员之间的差异,重复此操作两次,以包括三位评估者(两位注册护士,一位医生)。三位评估者一直参加整个研究期间。
- 数据采集表上包括患者的性别、年龄、诊断和影响愈合的其他重要不良因素,以备日后分析。
结果
由于需要一种以上统计学方法来确定装置之间和评估者之间可信度测试的精细变化,请求了一位统计师的帮助以进行数据分析。
红外线温度计比较
使用配对T检验(用于确定平均值是否彼此有显著差异)将每个温度计获得的原始温度测量差异相互比较时,观察到的P值显示出一定偏差(见表1)。

在五次T检验的每一次中,都在2、4和5号温度计中以95%的显著水平拒绝了零假设(对照测量值与其他温度计测量值无显著差异)。我们因此可以得出结论,在绝对精度方面,这些温度计的精确性能存在偏差和显着变化。
鉴于通过皮肤温度升高的评估来确定伤口深层和周围感染属于NERDS© 和STONEES©5,红外线温度测量的目的是确定3华氏度以上的温差属于阳性测试结果。因此,受测温度计获得的原始温度值不需要与对照温度计完全相同,但绝对应该能够检测出3华氏度的温差,这样才能成为临床实践环境中的可行测量方法。这是在此数据集上进行的下一个测试。
每位评估者使用对照温度计和其他温度计检测到3华氏度温差的几率(要么均>=3 或均<3)见表2。结果表明,无论是哪位评估者,全部五种微型温度计都可以在90.933%的情况下正确检测到3华氏度温差,成功几率为9/10。
温度计的可解读性
采用配对T检验确定三位评估者获得的平均值是否有统计学显著性差异(检验旨在确定评估者之间的平均值是否有显著差异),结果见表3。P值记录于表中,且它必须大于0.05才能表明一致性和类似性。
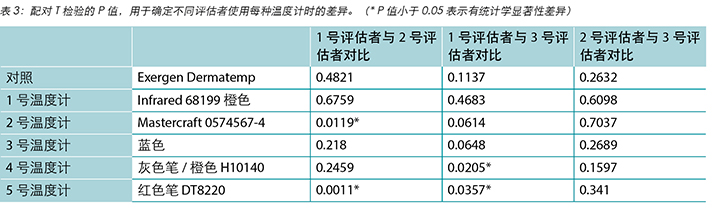
在对照测量和采用1号和3号温度计的每次测量中,三位评估者获得的平均值没有统计学显著性差异。采用2号温度计(1号和2号评估者)、4号温度计(1号和3号评估者)和5号温度计(1号和2号评估者;1号和3号评估者)获得测量值有统计学显著性差异。
相对于Exergen Dermatemp,性能最好的温度计是1号和3号温度计,无论是哪位评估者都可以获得一致测量值。但是,不同评估者使用2号、4号和5号温度计获得的测量值有差异,其中P值小于0.05。
讨论
在本研究中,微型红外线温度计检测到3华氏度温差的几率较高,评估者之间确定温差的可信度较高。这为将此方法纳入标准伤口护理实践中以便全面进行伤口评估提供了更多选择。除了阅读设备的使用说明之外,评估者只需接受简单培训就可以完成正确的临床温度测量评估,与黄金标准装置相比,成功几率为9/10。
在测试的微型温度计中(表4),两种温度计由不同评估者使用时测量值更一致,原始温度测量精密度和检测3华氏度温差的能力与对照温度计相比均非常好。1号温度计的测量距离与测量点大小之比为8:1(也最适合感染的控制),不仅测量精密度高,而且手柄握持舒适度高,有助于保持稳定。虽然3号温度计的测量距离与测量点大小之比为1:1,但也可以获得一致性的测量值。尽管体积小,但是临床人员可以很好地将其握在手中,在对准测量时可以增加稳定性。这两种温度计还具有清晰的数字显示,便于从远处轻易读取测量值。
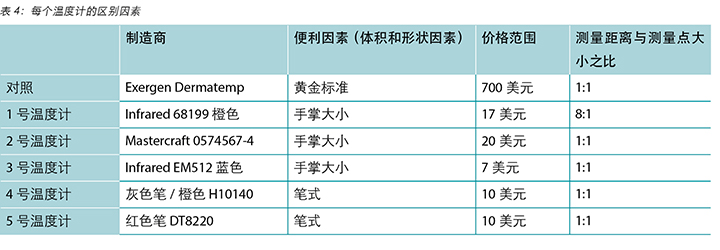
笔式温度计的测量距离与测量点大小之比均为1:1,评估者之间的差异最大,精密度误差因子最高。这些温度计的显示屏均较小,难以从远处精确读取测量值。大多数微型温度计使用纽扣电池,这增加了长期使用成本,因为电池寿命有限,研究结束时电力已经耗尽。
在检测3华氏度温差能力的准确度方面,所有温度计和所有评估者都可以在90.0%的情况下获得准确的测量(成功几率9/10)。这些平价微型红外线装置可以开始填补临床实践中的空白,能让临床人员在资源有限的环境下使用非侵入式表面温度测量装置来评估伤口是否存在深层和周围感染。这是一种可定量和可比较替代方法,将取代临床人员的主观评估,即,使用其手背触摸患者皮肤来判断温差10。
结论
无论选择哪种微型非接触式红外线温度计,它们都可以在全面伤口评估中检测3华氏度温差。无论使用哪种微型红外线温度计,临床人员都可以非常可靠地检测到温差,每次准确度达90.9%。
利益冲突
作者声明没有利益冲突。
资助
作者未因该项研究收到任何资助。
Author(s)
Hiske Smart
RN, MA(Nur), PG Dip WHTR (UK), IIWCC(Can)
Clinical Nurse Specialist, Wound Care and Hyperbaric Oxygen Therapy Unit, King Hamad University Hospital, Kingdom of Bahrain
Eman Al Jahmi
RN, MSc(Nur), IIWCC (South Africa)
Wound Care Practitioner, Wound Care and Hyperbaric Oxygen Therapy Unit, King Hamad University Hospital, Kingdom of Bahrain
Ebrahim Buhiji
MD, MB (Egypt), MSc Wound Management (UK), IIWCC(UAE) Wound Care and Hyperbaric Oxygen Therapy Unit, King Hamad University Hospital, Kingdom of Bahrain
Sally-Anne Smart
BSc Hons (Actuarial Science), BSc (Actuarial & Financial Mathematics), TASSA, University of Pretoria, South Africa (MSc Candidate Actuarial Science)
Correspondence to: Hiske Smart
Email hiske.smart@khuh.org.bh
References
- Fierheller M. A clinical investigation into the relationship between increased peri-wound skin temperature and local wound infection in patients with chronic leg ulcers. Adv Skin Wound care 2010 Aug; 23(8):369–79.
- Mufti A, Coutts P & Sibbald RG. Validation of commercially available infrared thermometers for measuring skin surface temperature associated with deep and surrounding wound infection. Adv Skin Wound Care 2015 Jan; 28(1):11–16.
- Sibbald RG, Goodman L, Woo KY et al. Special considerations in wound bed preparation 2011: an update©. Adv Skin Wound Care 2011 Sep; 24(9):415–36.
- Gardner SE, Frantz RA & Doebbeling BN. The validity of the clinical signs and symptoms used to identify localized chronic wound infection. Wound Repair Regen 2001; 9:178–86.
- Woo K & Sibbald RG. A cross-sectional validation study of using NERDS and STONEES to assess bacterial burden. Ostomy Wound Manage 2009; 55(8):40–8.
- Hurlow J & Bowler PG. Clinical experience with wound biofilm and management: a case series. Ostomy Wound Manage 2009; 55(4):38–49.
- Vernon GI. Non-contact infrared thermometers. Br J Gen Pract 2014 Dec; 64(629):615.
- Teran C, Torrez-Llanos J, Teran-Miranda T, Balderrama C, Shah N & Villarroel P. Clinical accuracy of a non-contact infrared skin thermometer in pediatric practice. Child Care Health Dev 2012; 38:471–6.
- Habera J, Kashida MN, Borhanib N et al. Infrared imaging of temperature profiles in microreactors for fast and exothermic reactions. Chem Eng J 2013; 214:97–105.
- Murff RT, Armstrong DG, Lanctot D, Lavery LA & Athanasiou KA. How effective is manual palpation in detecting subtle temperature differences? Clin Podiatr Med Surg 1998; 15:151–4.


