Volume 40 Number 3
Preventing facial pressure injury for healthcare providers adhering to COVID-19 personal protective equipment requirements
Hiske Smart, Francis Byron Opinion, Issam Darwich, Manal Aly Elnawasany and Chaitanya Kodange
Keywords COVID-19, personal protective equipment, coronavirus, enabler, facial injury, friction, medical device-related pressure injury, N95 mask, oxygen saturation, silicone dressing, skin
For referencing Smart H et al. Preventing facial pressure injury for healthcare providers adhering to COVID-19 personal protective equipment requirements. WCET® Journal 2020;40(3):9-18.
DOI https://doi.org/10.33235/wcet.40.3.9-18
Abstract
Objective To determine if a repurposed silicone-based dressing used underneath an N95 mask is a safe and beneficial option for facial skin injury prevention without compromising the mask’s seal.
Methods Since February 21, 2020, staff in high-risk areas such as the ED and ICU of King Hamad University Hospital have worn N95 masks when doing aerosol-generating procedures to protect against the novel coronavirus 2019. At that time, without education enablers or resources that could be directly translated into practice, the hospital’s Pressure Injury Prevention Committee explored and created a stepwise process to protect the skin under these masks. This procedure was developed over time and tested to make sure that it did not interfere with the effectiveness of the N95 mask seal.
Results Skin protection was achieved by repurposing a readily available silicone border dressing cut into strips. This was tested on 10 volunteer staff members of various skin types and both sexes who became part of this evidence generation project. Oxygen saturation values taken before and after the 4-hour wear test confirmed that well-fitted facial protection did not compromise the mask seal, but rather improved it. An added advantage was increased comfort with less friction as self-reported by the staff. An educational enabler to prevent medical device-related pressure injuries from N95 mask wear was an important additional resource for the staff.
Conclusions This creative and novel stepwise process of developing a safe skin protection method by which staff could apply a repurposed silicone border dressing beneath an N95 mask was largely effective and aided by the creation of the enabler.
Introduction
The global impact of the novel coronavirus 2019 (COVID-19) has had severe implications for frontline healthcare providers (HCPs). The safety of HCPs requires consistent and adequate use of personal protective equipment (PPE). In particular, the use of facial protective equipment against aerosolized transfer of COVID-19 droplets is a key recommendation worldwide.1 It requires the use of a protective filtering respirator such as an N95 mask, eye protection such as glasses, fitted facial shields, and/or specially designed protective suits. Facilities have noted an attendant increase in medical device-related pressure injuries among frontline HCPs wearing facial PPE protection that requires risk mitigation. Guidelines are being rapidly developed all over the world to ensure that the best solution for each setting can be implemented.
The staff of the King Hamad University Hospital (KHUH) includes many ethnicities and various skin types. As in many other facilities, these HCPs have been wearing PPE with N95 masks in high-risk areas since February 2020 as protection against COVID-19 (first confirmed case, February 21, 2020).2 Early on, the Pressure Injury Prevention and Nursing Quality Committees of the KHUH agreed that PPE-related pressure and skin injury protection of all staff fell under their purview. Bundled pressure injury prevention interventions3 such as the INTACT SKIN bundle are supported by the best evidence for patient pressure injury prevention; the use of these bundles is well documented in high-risk settings. Accordingly, the Nursing Quality Committee advised the Pressure Injury Prevention Committee to follow this approach in developing and testing a skin care bundle specifically applicable to the work environment of KHUH for those HCPs providing acute COVID-19 care.
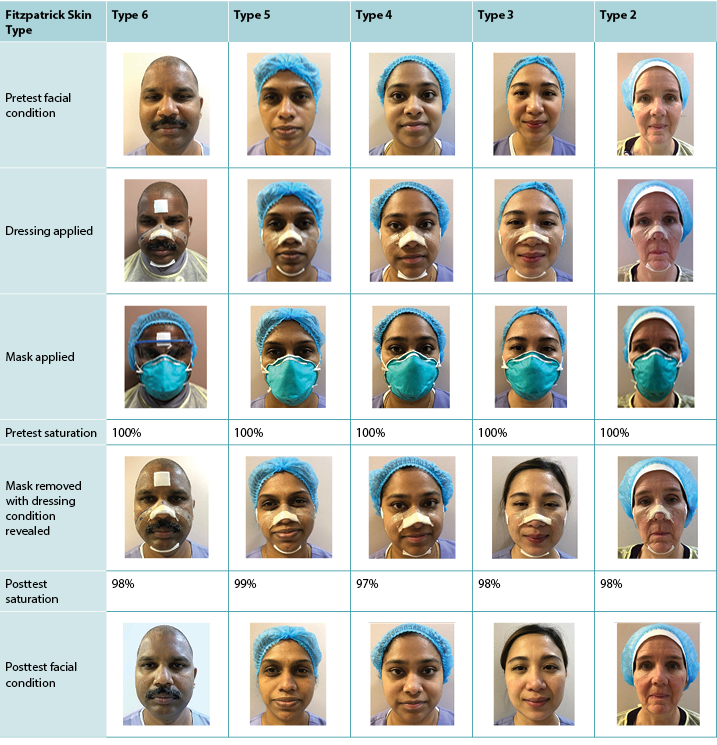
A mnemonic-based approach4 was used to enhance knowledge retention, with a one-word reminder of the importance of self-care: HELP. This mnemonic was designed to help HCPs remember the new rules and procedures that had been implemented in a very short time. This led to the creation of the HELP enabler, which emphasizes 10 evidence-based points to improve HCP prevention of facial mask injuries (Figure 1). The key message is to help yourself first, before helping others. Elements such as sufficient hydration5 and nutrition6 to support a 4-hour shift, emptying bladders before donning PPE,7 keeping an eye on the amount of time spent in PPE,1,3,8 good skin hygiene,9 and the importance of mask leak tests1 form the basis of this care bundle. Additional recommendations include using an acrylate lotion10 or a protective dressing11 for facial protection under PPE.
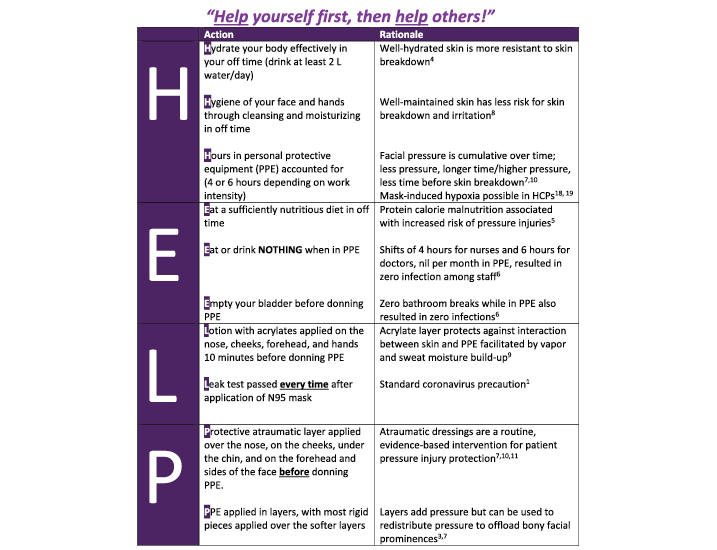
Figure 1. Help enabler © Smart 2020.
Because adhesives increase the risk of skin stripping and subsequent skin tear injuries,12 the use of an atraumatic silicone dressing on the face also was proposed. The Pressure Injury Prevention Committee repurposed a readily available dressing for facial pressure injury prevention in the absence of existing evidence. However, the team had to establish that this use would not compromise the N95 seal efficacy, and facial skin would remain intact under the dressing. Further, because this study had to address skin safety for all staff, skin type variation had to be taken into account; for this, researchers used the Fitzpatrick skin type classification.
The Fitzpatrick skin type classification13 was developed in the 1980s to measure the impact of sunburn injury on different skin types and is deemed the criterion standard for skin type classification. The classification comprises six skin types ranging from light skin (type 1, which burns easily and never tans, and type 2, which usually burns and tans slightly) to olive/medium brown skin (type 3, which initially burns and tans well, and type 4, which usually tans) and finally to dark brown and black skin (types 5 and 6).13 In this study, no HCP with type 1 (extremely light Caucasian skin) could be included because there are no nursing staff with that skin type at KHUH.
Methods
This prospective observational cohort study was divided into five steps to establish the appropriateness, efficacy, and safety of each phase. It involved wear-time tests culminating in a final 4-hour crossover experiment. Developing the protocol and assembling key departments (nursing, infection control, quality assurance representatives, COVID-19 hospital committee) to discuss and approve the proposed skin protection protocol took time; this practice innovation began in March 2020 and was tested in the first 2 weeks of April 2020.
Institutional review board approval was received because the study involved human participants (reference #20-334). Because N95 mask wear is mandatory for COVID-19 frontline care provider safety, any facial injuries sustained as a result were not deemed an ethical objection for this experiment. Essentially, facial injury was the real-life risk this study tried to mitigate. Participants signed an informed consent form to take part in the study and for all photographs to be used in subsequent publication with no parts of faces obscured.
Phase 1. Ascertain how to repurpose an atraumatic silicone border dressing (Mepilex border sacrum; Mölnlycke, Norcross, Georgia) to cover bony facial prominences without compromising the N95 particulate respirator and surgical mask fit (3M type 1860, Minneapolis, Minnesota) using only one small dressing per day for the duration of a shift (this allows for the most stringent interpretation of infection control practice).
Phase 2. Fit eight participating staff members with various skin types who volunteered for this project with a protective dressing layer. Have infection control staff conduct an N95 fit test according to international best practice.
Phase 3. Continue the use of facial protection for 1 hour after the fit test and examine the condition of the facial skin thereafter.
Phase 4. Determine the efficacy and stability of the dressing underneath a fitted N95 mask after 3 hours and examine facial quality thereafter. (Only one participant was included in this phase.)
Phase 5. Compare the difference in facial skin quality and metabolic oxygen saturation values (Spo2) as determined by a fingertip applied pulse oximeter with and without facial protection applied in a 4-hour shift period on a normal working day among five participants. This test took place over 2 days in a work environment not actively caring for patients who were COVID-19 positive. Facial skin evaluation and Spo2 values before and after removal of the mask were repeated.
Results
Phase 1
During the study development period (March 2020), relevant guidelines on this topic were scarce. A process of creative problem solving was therefore followed to determine how facial skin injuries in HCPs in the authors’ setting could be addressed in the most efficient and cost-effective manner. Because staff would have to remove the protective dressing at the end of each shift, it was clear that any product with aggressive adhesion would soon strip the outer layer of the skin12 and that the additional pressure exerted by the N95 mask on the barrier would enhance adhesion. Pain on removal and skin injury over time would be likely.12 Therefore, an atraumatic dressing was required.
At the KHUH, an atraumatic silicone sacrum dressing is routinely used for pressure injury prevention in high-risk hospitalized patients11 as part of the standard pressure injury prevention skin care bundle.3 It is the only type of atraumatic silicone dressing available in the authors’ setting; each dressing is similar in cost to a take-away coffee. The aim was to repurpose a single 10 × 10 dressing for frontline HCPs during each shift to provide facial protection and limit cost for the institution.
Figure 2 illustrates how the dressing was repurposed. The application technique includes the bridge of the nose, with the open edge of the dressing facing the nose tip and sides of the nose. Another piece is placed underneath the jaw with the open end facing forward on the chin edge, and other pieces are placed over the cheek bones. The Supplemental Table provides a step-by-step overview of dressing application (http://links.lww.com/NSW/A##).
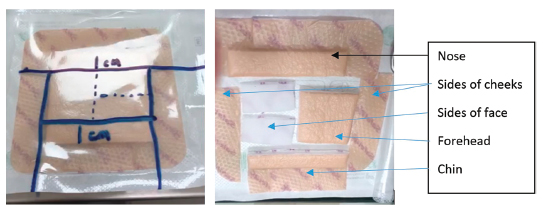
Figure 2. Repurposing the dressing
Earlier testing revealed that the dressing edge could catch on to the N95 mask sponge and create an interlocking mechanism to position two offloading areas next to each other rather than on top of each other. This enhances the distribution of pressure over a larger area and prevents additional pressure on any given area by stacking multiple layers. The rationale was that if pressure was equally distributed over the nose with the interlocking fit of the N95 mask sponge on the dressing edge, the cheekbones were only in need of friction control (maintaining mask integrity without adding bulk). Further, this placement was successful even with some small facial hair stubble present on the cheeks and chins of male staff members; the dressing sat snugly despite being applied over chin hair, and removal was painless.
There was a square piece left for the forehead that could be used as pressure relief underneath protective eye shields or goggles resting on the forehead. Two additional small pieces remained to offset the pressure from the elastic band of the N95 mask touching the sides of the face close to the ears (Figure 3).
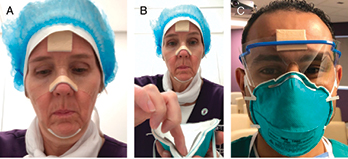
Figure 3. Dressing application and personal protective equipment fit
Phase 2
To ensure each person uses the correct N95 mask size, a standardized initial fit test in accordance with international guidelines is required. The KHUH infection control team conducted the leak tests in late January and early February using the hood method.14,15 The method involves placing a see-through polymer hood with an applicator window in front of the face and a tight-fitting seal around the HCP’s neck. To determine a participant’s individual sensitivity, a distinct smell (denatonium benzoate) is serially sprayed into the hood to determine at what point (after how many sprays) a smell is observed. Next, the hood is removed, and the participant is instructed to rinse his/her mouth and wait 15 minutes. Then, an N95 mask is donned, and the procedure repeated. The mask fit is deemed effective when no smell is observed if half of the sprays required during the sensitivity test are applied. The infection control team documents each time a person passes the fit test (smell only observed after more than the threshold number of sprays). A person who fails the fit test is fitted with a different-sized mask, and the spray test is repeated until passing; however, it only needs to be completed once per person.14
Leak testing is the responsibility of each staff member and involves positioning the N95 mask on the head and fitting it around the nose by applying two fingers on either side of the nose and pressing the mask tight while breathing in. Next, hands are placed over the middle of the mask (without adjusting its position), and the staff member exhales sharply. If air escapes from the sides of the mask, the mask should be adjusted, and all of the steps repeated until exhaled air exits only through the middle of the mask and no leaks occur on inhalation or exhalation. This process is repeated twice every single time an N95 mask is applied.16 Where limited reuse of N95 masks is practiced, it is done in accordance with the KHUH infection control protocols governing mask functionality/cross-contamination prevention and not to exceed five uses per person.17
Eight volunteer staff members (four male and four female) with various Fitzpatrick skin types were included in this phase. Two work in the ED, two in ICU, one in a male surgical ward, and three in the wound care unit. All participants had previously passed the official N95 fit test. All staff previously wore N95 masks without skin protection. Participants applied the repurposed, separated atraumatic dressing segments on their own faces after an initial demonstration. The application took less than 5 minutes, inclusive of the time required to cut up the dressing. They then donned N95 masks and conducted manual leak tests.16 All eight participants achieved the same mask positioning with the applied dressing beneath their mask as without.
Infection control then conducted another fit test. Staff all reported only a slight smell after four sprays, and this was consistent up to six sprays. Therefore, 95% blockage was achieved with this mask configuration. This outcome was certified by infection control as conforming to international standards—that is, all eight participants passed the fit test while using the atraumatic dressing.
Phase 3: Wear Comfort
Staff were instructed to maintain that exact PPE configuration for the next hour without repositioning or removal. Once the hour was over, they had to remove the mask and the facial dressing themselves, take a photograph of their face, and present it to the research team. All photographs were time stamped to ensure masks were not removed before the period was completed.
Staff also had to report on this experience compared with their previous experience/original fit tests. There were no negative comments from the staff, despite application over hair in some men. In fact, some staff noticed that the nose dressing prevented mask movement they had previously experienced when looking up or down. This interlock also helped to minimize the perpendicular pressure of the N95 mask exerted on the nasal crest; all participants commented on improved nose comfort, as well as the absence of facial irritation caused by the direct contact of mask fibers to the cheeks. Comfort underneath the chin was also noted; itching and moisture vapor build-up appeared to be absent in this configuration. When asked if the dressing was worth the application time, the answer was a unanimous yes.
The immediate facial condition of all staff with protective dressings can be seen in Figure 4. Those with Fitzpatrick skin types 2 and 3 (lighter skin tone, n = 2) showed a bit of visible erythema over the bony cheek area. No marked erythema or pressure was visible on any of the other participants (n = 6). No erythema or pressure marks were visible on any staff member on the sides of his/her face where the top applied elastic band of the N95 mask is placed.

Figure 4. All faces after 1 hour of mask wear with facial protection
Phase 4
One staff member with Fitzpatrick type 2 skin was willing to test the mask without facial protection for 2 hours on a different day, before the leak tests were conducted. Researchers believed that this skin type would show visible injury most quickly. The next day, this participant wore the mask for 3 hours with facial protection applied. The results of this trial are depicted in Figure 5.
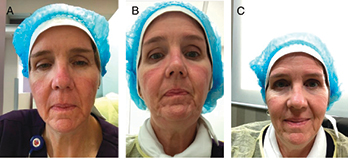
Figure 5. A, Two hours of mask wear without interfacing. B, Three hours of mask wear with interfacing. C, One hour after removal of interfacing and mask (3 hours’ wear)
Mask wear without skin protection resulted in friction and chafing with erythema visible over and along the bony prominences of the cheekbones. A blanchable area was visible on the bridge of the nose after the 2-hour test. This finding is consistent with extant literature reporting that pressure injury can occur in as little as 2 hours.8,11
After testing with facial protection, slight erythema was again present over the bony prominences of the check bones with only a little redness on the left lateral side of the nose. However, these changes were much less noticeable than before, without additional friction or chafing areas present, signifying good mask fit with minimal movement during the 3-hour period. All erythema visibly diminished after 1 hour.
Phase 5
This experimental test took place over 2 consecutive days with five volunteer staff members (one male and four female) with skin types from fair to dark brown on the Fitzpatrick scale. Researchers theorized that skin damage or injury would be easier to observe in females, who have thinner skin than males.18 If female skin was protected by the selected method, it could reasonably be assumed that males would be protected as well. Female nurses also outnumber male nurses in this setting and are therefore more likely to participate in direct care and require protection.
On the first day of this phase, the N95 mask was worn for 4 hours (no eating, drinking, or bathroom breaks allowed) with protection prepared and applied by each participant. Comfort was self-assessed by participants. At the end of the 4 hours, three participants felt that they could have continued for an hour or two more. Slight sweating was present, with indentations visible on all of the participants’ faces. Only one (Fitzpatrick type 2) presented with slight erythema; the least damage was visible on the darkest skin.
Pulse oximetry saturation levels of each participant were also taken before and after the test. All participants lost between 1% and 3% Spo2 in this test, with a mean loss of 2% metabolic Spo2 (Table 1). This is in line with extant studies on N95 mask use that confirms overall oxygen intake is diminished during wear, even with a perfectly fitting mask.19,20
Table 1. Four-hour wear time test with facial protection
On the next day, the N95 mask was worn without any protection (Table 2). Each participant positioned his/her own mask, and it was again worn for 4 hours without any eating, drinking, or bathroom breaks. All four female participants battled with discomfort; pruritus on the mask edges was noted after the first hour. All participants reported that they were relieved when the mask could be removed; none wished to continue wearing the mask for a longer time.
Table 2. Four-hour wear time test without facial protection
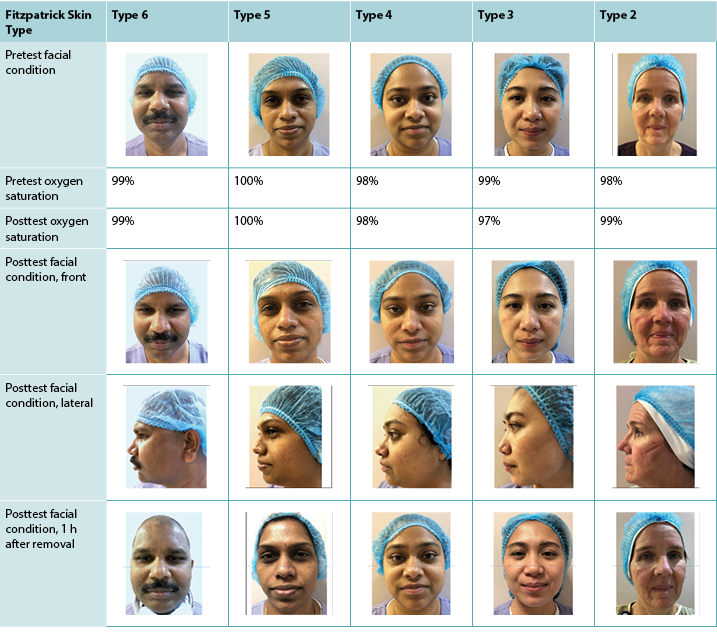
Less moisture build-up was visible compared with the day before, but skin indentations were present on all five faces. The lighter skin tones appeared to have more pressure-related impact than those with darker skin tones. All four female participants had various levels of skin erythema, with the fair skin most damaged of all. The participant with the darkest skin had the least visible damage; one small darkened area was visible that fully recovered in 1 hour. Of the female participants, three continued to have signs of indentation and erythema an hour after the test, with the fair-skinned participant least recovered compared with results from the day before.
With regard to metabolic Spo2 on the second day, three participants retained the exact same starting value, and one gained 1%. The remaining participant had a 2% Spo2 loss. The mean loss was 0.2% metabolic Spo2. Figure 6 depicts Spo2 readings taken from the same participant before and after both 4-hour tests.
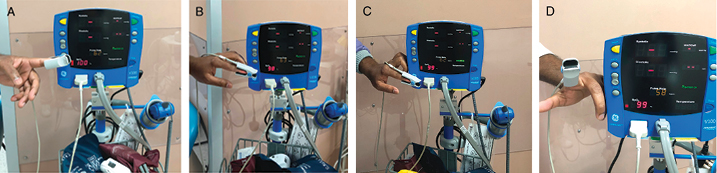
Figure 6. Example of Pulse oximetry saturation readings
A, Before 4-hour wear time test with facial protection (100%). B, After 4-hour wear time test with facial protection (98%). C, Before 4-hour wear time test without facial protection (99%). D, After 4-hour wear time test without facial protection (99%).
Discussion
This article describes a holistic approach to facial skin injury prevention for HCPs to “HELP” staff to embrace a complete self-care approach while working in a high-risk COVID-19 setting. Facial protection was the cornerstone of this safety initiative.
Longer periods of PPE use (with each participant serving as his/her own control) produced a distinct difference between mask wear with and without protection, including improved facial condition and comfort without compromising mask seal. Three possible mechanisms of injury were identified in this experiment. The first was associated with direct high pressure causing skin indentations (ie, from mask edges, nose fitting device, and straps); the second was a diffuse erythema in a linear pattern associated with lower pressure with or without friction (ie, mask edges moving). Both were more pronounced when no facial protection was present. The third was related to sweating: slight localized sweating underneath the mask was more pronounced when skin protection was used, attributable to the better integrity of the acquired seal. Associated moisture build-up from sweat is therefore a risk with this PPE configuration; accordingly, the use of a skin-protective acrylate10 followed by meticulous facial care9 is recommended for off-duty HCPs.
All participants cut up the dressing into segments with ease and could easily apply the dressing to their faces with the use of a mirror. After donning this protective layer, the integrity of the N95 mask was also easily established, with all staff passing both the leak and the fit tests.
The most crucial safety consideration for frontline providers during the pandemic lies in the order of PPE removal; it must be doffed in the exact reverse order it was donned.1 Bathroom and eating breaks cannot be factored into shifts because the proper reverse removal of layers of PPE takes more time than application to prevent contamination and risk to others in the facility.1,7 All body PPE must be removed first, followed by a thorough handwashing,21 after which the N95 masks are removed by touching only the elastic bands,1 and the handwashing procedure is repeated before the facial protective dressings can be removed. Essentially, staff can greatly increase the risk of COVID-19 self-contamination if they touch their faces before all contaminated PPE is safely removed.1
This stringent PPE process requires heightened staff awareness of this vital safety precaution, reinforcing the HELP enabler’s focus on adequate nutrition and hydration in off-duty times and recommendations to limit excessive amounts of fluids immediately before a shift. Given these self-care strategies, a 4-hour fasting period is feasible. The key is to plan and shift nutrition and hydration activities to directly after and/or no less than an hour before a shift. Staff with medical conditions who cannot adhere to a 4-hour fasting or bathroom break-free shift should be deemed at high risk of contagion not only to themselves, but also others using the same facilities.
At least one facility has already trialed this approach with success. For each 4-hour shift of frontline staff in full PPE in Wuhan, China,7 touching masks, eating, drinking, and bathroom breaks were prohibited. This simple process ensured zero staff contracted COVID-19.7 Their experience provided the rationale for the 4-hour wear test conducted in this study.
A different cross-sectional study22 (N = 4,306) from China on facial injuries sustained by HCPs when using PPE also identified this 4-hour cutoff time. Researchers found a statistically significant difference in the number of injuries sustained if HCPs exceeded this time frame in PPE.22 Skin protection under masks is therefore a necessity because shift lengths can be unpredictable based on PPE supplies23 and facial injuries have been noted in shorter shift periods22 (within 2 hours in this study).
It is of vital importance that hours of PPE wear (regardless of facial protection applied) be documented3 to prevent prolonged exposure, excessive moisture build-up, and skin breakdown. Based on the experience of aggressive frontline COVID-19 care in Wuhan,7,22 it is recommended that each 8-hour shift be divided between two teams where one team does the work requiring N95 mask wear (in the dirty/infected area), while the rest works in the clean area. After 4 hours inside without eating, drinking, or a bathroom break in full PPE, the two teams switch. This prevents exhaustion and mask hypoxia19 and protects the skin of HCPs7,22 with minimal impact on staffing.
The most interesting finding of this study was the drop in participant Spo2 values by 2% on average when using the protective dressing underneath the N95 mask. This corresponds with tight-fitting mask wear studies conducted during flu outbreaks.19,20 It is possible that the protective dressing increases the mask’s seal stability while mitigating pressure-related skin damage. Critically, extended periods of N95 mask wear may be related to mask-induced hypoxia in HCPs;19,20 hypoxia is an established major risk factor for pressure-related skin breakdown.3 Mitigation of this concern can be achieved by the split-shift approach previously described.7,22
The reduced Spo2 finding was not the case with N95 mask use alone. This may indicate that, despite passing the fit and leak tests, the discomfort from mask wear results in participants occasionally moving their faces to relieve pressure and facial irritation, which could result in small leaks. The participant with type 2 skin most likely had a leak present during the test where the protective layer was not applied that was sustained during the test by mouth, chin, and facial movements. This participant had a 1% increase in Spo2 and the most pronounced skin damage present after the test.
Mask discomfort may therefore add to the iatrogenic risk of contracting COVID-19 infection. The same risk applies to staff with any facial injury resulting in a skin breach, because pain may compromise proper N95 mask seal. Adding repeated pressure to an existing facial injury has the potential to exacerbate minor injuries and lead to deeper dermal injuries; this is why patients are carefully positioned to displace pressure to other body parts once a stage 1 pressure injury is present.3
Limitations
This small sample was recruited to serve in a pilot project to determine if the application of a facial protective layer could mitigate facial injury risk among N95 mask wearers. More research using different border dressings would be beneficial to expand the evidence base on this topic and give providers more options.
The staff at KHUH is also mainly of West and East Asian descent, hence the lack of a nurse with a Fitzpatrick skin type 1. This is a major limitation because this skin type is usually the most sensitive to injury and skin insults. Further, although the Fitzpatrick scale is the criterion standard for sun-related skin damage, it may not fully predict pressure and shear damage on skin because deeper injuries may not be immediately visible. Further testing in institutions that have HCPs with Fitzpatrick type 1 skin is warranted.
Further work is also needed on N95 mask wear and the impact of reduced Spo2 on fatigue, headache, and concentration to determine the optimal safety balance between skin risk, metabolic stress, and personal protection.
Conclusions
Early on in the COVID-19 health crisis, the need to protect the skin of HCPs was prioritized at the KHUH. At that time, there were no educational resources available to guide practice. (Some enablers have since been released, beginning in April 2020.24,25) The creative stepwise process of skin protection described in this article was developed with readily available products and participants who volunteered to help develop a safe solution for skin injury prevention.
At roughly the same cost as a daily take-away coffee, a repurposed atraumatic silicone border dressing can support skin health underneath a tight-fitting mask. By cutting it into segments and carefully applying it without creases over the nose, cheekbones, and sides of the face, HCPs can achieve pressure redistribution and facial skin protection. This method does not appear to interfere with N95 mask integrity and in fact may provide additional leak protection by securing the mask more firmly in position, ultimately protecting against accidental viral transfer to the face.1 Accordingly, these authors recommend that HCPs add an atraumatic silicone border dressing as a safe and beneficial option to protect facial skin under PPE.
However, no dressing by itself (regardless of testing) can provide complete care of facial skin underneath N95 masks. It is critical that HCPs implement a comprehensive skin care approach. Frontline staff who “HELP” themselves by taking responsibility for their own skin care and who are well prepared, well rested, fed, and hydrated can more safely take care of others.
It is the authors’ hope that this creative evidence-based clinical facial protection solution and HELP enabler will be of assistance to their global colleagues in the fight against COVID-19.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
遵从COVID-19个人防护装备要求的医疗保健提供者预防面部压力性损伤的研究
Hiske Smart, Francis Byron Opinion, Issam Darwich, Manal Aly Elnawasany and Chaitanya Kodange
DOI: https://doi.org/10.33235/wcet.40.3.9-18
摘要
目的 确定在N95口罩下使用重新裁剪的硅酮敷料是否是一种安全、有益的选择,可以在不影响口罩气密性的情况下预防面部皮肤损伤。
方法 自2020年2月21日起,哈马德国王大学医院急诊科(ED)和重症监护病房(ICU)等高危区域的医护人员在从事产生气溶胶的操作时一直佩戴N95口罩,以预防2019新型冠状病毒。当时,在没有可以直接转化为实践操作的教育使能器或资源的情况下,医院的预防压力性损伤委员会探索并创建了一个保护口罩下皮肤的分步程序。该程序根据时间经验开发并经过了测试,确保其不会影响N95口罩密封的有效性。
结果 通过将现成的硅酮有边型敷料切成条状进行重新裁剪,实现了皮肤保护。在成为本证据产生项目一部分的10名不同皮肤类型和性别的志愿医护人员中进行了测试。在4小时佩戴测试前后测得的血氧饱和度值证实,密合的面部保护装备不会影响口罩的气密性,反而会改善口罩的气密性。另一项优势是,据医护人员自述,摩擦力较小,舒适度增加。预防因佩戴N95口罩导致的医疗器械相关压力性损伤的教育使能器是医护人员的重要补充资源。
结论 制定安全的皮肤保护方法,让医护人员可借此在N95口罩下使用重新裁剪的硅酮有边型敷料的这一创造性和新颖的分步程序在很大程度上是有效的,并得益于使能器的创建。
引言
2019新型冠状病毒(COVID-19)的全球性影响力对一线医疗保健提供者(HCP)产生了重大影响。保证HCP的安全需要其始终充分地使用个人防护装备(PPE)。特别是,使用面部防护装备来防止COVID-19飞沫的气溶胶传播是全球范围内的一项重要建议1。这需要使用过滤式防护口罩(如N95口罩)、眼部防护装备(如护目镜)、适合的护面罩和/或专门设计的防护服。各医疗机构已经注意到,在佩戴面部PPE保护的一线HCP中,医疗器械相关压力性损伤的发生率也随之增加,需要降低风险。世界各地正在迅速制定指南,以确保能够实施适合每个环境的最佳解决方案。
哈马德国王大学医院(KHUH)的医护人员包括许多种族和各种皮肤类型的医护人员。与许多其他医疗机构一样,自2020年2月以来,这些HCP一直在高危区域穿戴包含N95口罩的PPE,以防止感染COVID-19(第一例确诊病例出现于2020年2月21日)2。从早期开始,KHUH的预防压力性损伤委员会和护理质量委员会就一致认为,所有医护人员的PPE相关压力性损伤和皮肤损伤保护属于其职责范围。组合式压力性损伤预防干预措施3,如完整皮肤(INTACT SKIN)组合,得到了患者压力性损伤预防的最佳证据支持;在高危环境中使用这些组合的情况拥有完备记录。因此,护理质量委员会建议预防压力性损伤委员会遵循这一方法,为提供COVID-19急性护理的HCP开发和测试专门适用于KHUH工作环境的皮肤护理组合。
采用了一种基于助记符的方法4来增强对知识的记忆,并以一个词提醒自我照护的重要性:HELP。该助记符旨在帮助HCP记住在极短时间内实施的新规则和程序。为此创建了HELP使能器,该使能器强调了10个用于改善HCP对口罩相关面部损伤的预防的循证要点(图1)。关键信息是先自助,后助他。足以支持4小时轮班的充分补水5和营养6、穿戴PPE前排空膀胱7、注意穿戴PPE的时间1,3,8、良好的皮肤卫生9和口罩泄漏测试的重要性1等要素构成了本护理组合的基础。其他建议包括在PPE下使用丙烯酸乳液10或保护性敷料11进行面部保护。
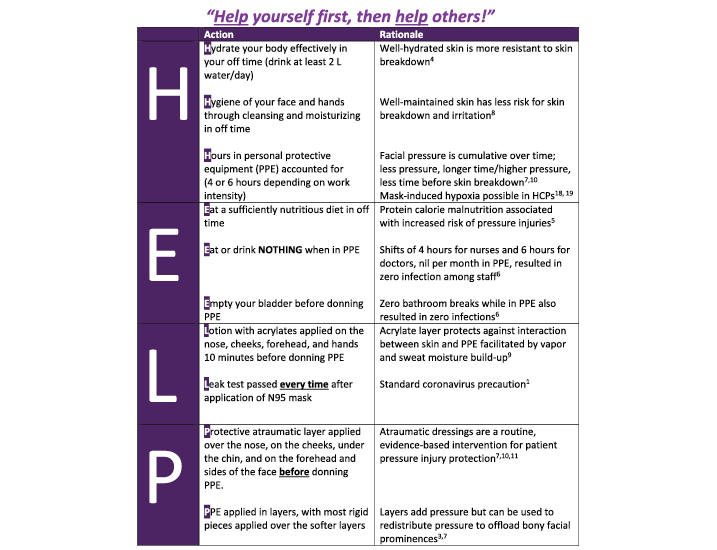
图1. Help enabler © Smart 2020.
因为粘胶增加了脱皮和随后的皮肤撕裂损伤的风险12,还建议在面部使用无损伤硅酮敷料。在缺乏现有证据的情况下,预防压力性损伤委员会将一种现成的敷料重新裁剪,用于面部压力性损伤预防。然而,该小组必须确定此类使用不会影响N95密封的有效性,且在敷料下的面部皮肤将保持完整。此外,由于本研究必须解决所有医护人员的皮肤安全性问题,因此必须考虑皮肤类型的差异;为此,研究人员采用了Fitzpatrick皮肤分型。
Fitzpatrick皮肤分型13于20世纪80年代开发,用于测量晒伤对不同皮肤类型的影响,被视为皮肤分型的判据标准。该分型包括六种皮肤类型,从白色皮肤(1型,容易晒伤但不会晒黑,2型,经常晒伤且有时晒黑)到橄榄色/中棕色皮肤(3型,有时晒伤且有时晒黑,4型,经常晒黑),最后到深棕色和黑色皮肤(5型和6型)13。在本研究中,由于KHUH没有1型(非常白的高加索人皮肤)的护理人员,因此无法纳入这种皮肤类型的HCP。
方法
这项前瞻性观察性队列研究分为五个步骤,以确定每个阶段的适宜性、有效性和安全性。它包括佩戴时间测试,最终为4小时的最终交叉实验。制定方案并召集关键部门(护理、感染控制、质量保证代表、COVID-19医院委员会)讨论和批准拟议的皮肤保护方案需要时间;这一实践创新于2020年3月开始,并在2020年4月的前2周进行了测试。
由于该研究涉及人类受试者,因此获得了机构审查委员会的批准(参考文件编号:20-334)。由于N95口罩的佩戴对于保证COVID-19一线护理提供者的安全是必需的,因此,任何因此而受到的面部损伤均不被视为本实验的伦理异议。实质上,面部损伤是本研究试图减轻的现实生活中存在的风险。受试者签署了一份知情同意书,同意参加研究及将其所有照片在随后的发表中使用,且面部没有任何部分被遮挡。
阶段1。确定如何重新裁剪无损伤硅酮有边型敷料(骶尾部有边型敷料;Mölnlycke,佐治亚州诺克罗斯市),以覆盖面部骨突,同时不影响N95防颗粒物口罩和外科口罩的密合性(3M 1860型,明尼苏达州明尼阿波利斯),每日一次轮班期间仅使用一小块敷料(这实现了对感染控制实践的最严格解释)。
阶段2。为自愿参加本项目的八名不同皮肤类型的受试医护人员敷用保护性敷料层。由感染控制人员根据国际最佳实践进行N95密合性测试。
阶段3。密合性测试后,继续使用面部保护1小时,随后检查面部皮肤状况。
阶段4。3小时后,确定在密合的N95口罩下敷料的有效性和稳定性,随后检查面部质量状况。(此阶段只纳入一名受试者。)
阶段5。比较五名受试者在正常工作日4小时轮班期内,在使用和不使用面部保护的情况下,通过指尖用脉搏血氧计测定的面部皮肤质量和代谢氧饱和度值(Spo2)的差异。该测试在不频繁忙于护理COVID-19阳性患者的工作环境中进行了2天。重复进行摘除口罩前后的面部皮肤评价和Spo2值测定。
结果
阶段1
在研究开发期间(2020年3月),关于该主题的相关指南极少。因此,我们遵循一个创造性的问题解决程序,以确定如何以最有效和最具成本效益的方式解决作者环境中HCP的面部皮肤损伤。由于医护人员必须在每个轮班结束时移除保护性敷料,因此很明显,任何具有极大粘附力的产品都将很快使皮肤外层脱皮12,而且N95口罩对皮肤屏障施加的额外压力将增强粘附力。随着时间的推移,可能会出现移除时的疼痛和皮肤损伤12。因此,需要使用无损伤敷料。
在KHUH,无损伤骶尾部硅酮敷料常规用于高危住院患者的压力性损伤预防11,作为标准压力性损伤预防皮肤护理组合的一部分3。这是作者研究环境中唯一可用的无损伤硅酮敷料类型;每片敷料的成本与外卖咖啡的成本类似。目的是重新裁剪单片10×10敷料,在每个轮班中为一线HCP提供面部保护并为医疗机构限制成本。
图2说明了敷料如何进行重新裁剪。敷料的敷贴技巧包括鼻梁,敷料的开口边缘朝向鼻尖和鼻翼两侧。另一片放在下颌下方,开口端朝前放在下巴边缘,其他敷料片放在颧骨上方。补充表提供了敷料敷贴的分步概述(http://links. lww.com/NSW/A##)。
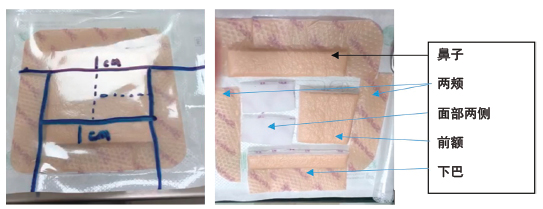
图2.敷料的重新裁剪
早期的测试显示,敷料边缘可以吸附在N95口罩的海绵上,并形成一个互锁机制,使两个卸荷区域彼此邻近,而不是位于彼此顶部。这增强了压力在更大面积上的分布,并通过堆叠多层来防止任何特定区域承受额外压力。其原理是,如果压力在鼻子上平均分布,敷料边缘上的N95口罩海绵互锁密合,颧骨只需要摩擦力控制(保持口罩完整性而不增加体积)。此外,即使在男性医护人员的脸颊和下巴上存在一些小的面部毛发胡茬,这种放置方式也是成功的;尽管敷料贴附在下巴毛发上,但敷料贴合紧密,且移除时无痛。
留有一个方形片用于前额,可用作前额上眼保护罩或护目镜下的减压装备。另外留有两个小片,用于抵消N95口罩松紧带接触面部靠近耳朵的两侧产生的压力(图3)。
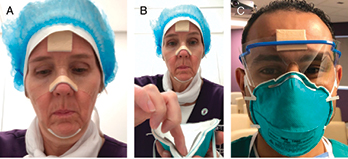
图3.敷料敷贴和个人防护装备密合性
阶段2
为了确保每个人都使用正确的N95口罩尺寸,需要根据国际指南进行标准化初始密合性测试。KHUH感染控制小组在1月底和2月初使用面罩法进行了泄漏测试14,15。该方法包括将一个带有敷抹器窗口的透明聚合物罩放在面部前方,并在HCP的颈部使用密合的密封。为了确定受试者的个人敏感性,将一种具有独特气味的气体(苯甲地那铵)连续喷入面罩内,以确定受试者何时(多少次喷雾后)能闻到该气味。然后,取下面罩,指示受试者漱口并等待15分钟。接着,戴上N95口罩,重复上述步骤。如果使用了在敏感性测试中所需的一半的喷雾次数,受试者未闻到气味,则认为口罩密合性有效。感染控制小组记录每次人员通过密合性测试的情况(只有在超过喷雾次数阈值后才闻到气味)。未能通过密合性测试的人员将佩戴不同尺寸的口罩,并重复进行喷雾测试,直到通过为止;但每人只需完成一次14。
每名医护人员均需要完成泄漏测试,其涉及将N95口罩放置在头部,将两根手指分别放在鼻子两侧,从而将口罩贴合在鼻子周围,一边吸气一边将口罩压紧。然后,双手放在口罩中部上方(不调整口罩位置),医护人员急速呼气。如果空气从口罩两侧逸出,应调整口罩,并重复所有步骤,直到呼出的空气只从口罩中部排出,吸气和呼气时均不发生泄漏。该程序在每次使用N95口罩时重复两次16。如果进行有限的N95口罩重复使用,则按照管理口罩功能/交叉污染预防的KHUH感染控制方案进行口罩重复使用,每人使用口罩不超过五次17。
本阶段纳入了8名不同Fitzpatrick皮肤分型的志愿医护人员(4名男性和4名女性)。两人在ED工作,两人在ICU工作,一人在男性外科病房工作,三人在伤口护理科工作。所有受试者之前均已通过正式的N95密合性测试。所有医护人员之前均在无皮肤保护的情况下佩戴过N95口罩。在初始演示后,受试者在自己的面部敷贴了重新裁剪、分离的无损伤敷料小片。包括剪开敷料所需的时间在内,贴上敷料所花的时间不到5分钟。然后,他们戴上N95口罩,手动进行泄漏测试16。所有八名受试者在口罩下方敷贴敷料后均将口罩调整至与未使用敷料时相同的口罩位置。
然后,感染控制小组又进行了一次密合性测试。医护人员均报告在四次喷雾后仅有轻微的气味,且这种气味在多达六次喷雾后是一致的。因此,使用这种口罩配置可实现95%的阻断。感染控制小组证明该结果符合国际标准,即所有八名受试者在使用无损伤敷料时均通过了密合性测试。
阶段3:佩戴舒适度
医护人员被指示在随后的一小时内保持该PPE配置,不得重新调整位置或移除PPE。一个小时结束后,他们需自己摘除口罩和移除面部敷料,拍摄一张面部照片,并提交给研究小组。所有照片均带有时间戳,以确保在佩戴期结束前未摘除口罩。
医护人员还必须将这一体验与他们之前的体验/最初的密合性测试比较,进行报告。尽管有些男性医护人员的敷料敷贴在其毛发上,但没有来自医护人员的负面评论。事实上,一些医护人员注意到,鼻子上的敷料避免了他们之前在向上或向下看时所经历过的口罩移位。这种互锁机制还有助于最大限度地减少N95口罩对鼻嵴施加的垂直压力;所有的受试者均表示鼻子舒适度有所提高,以及没有由于口罩纤维直接接触面颊而引起的面部刺激。也注意到下巴下方的舒适度;在这种配置中似乎没有瘙痒和湿气积聚。当被问及是否值得花费所需的敷贴时间使用敷料时,答案是一致的赞同使用。
所有使用防护性敷料的医护人员的即时面部状况如图4所示。Fitzpatrick皮肤分型2型和3型的医护人员(肤色较白,n=2)在面颊骨骼区域出现少量可见红斑。其他受试者(n=6)均未有明显的红斑或压痕可见。在医护人员放置N95口罩贴在面部上方的松紧带的面部两侧,未发现红斑或压痕。

图4.带面部保护装备佩戴口罩1小时后的所有面部
阶段4
一名Fitzpatrick 2型皮肤的医护人员愿意在另一天,在进行泄漏测试之前在没有面部保护的情况下进行2小时的口罩测试。研究人员认为,拥有这种皮肤类型的医护人员会最快出现可见的损伤。第二天,这名受试者在使用面部保护的情况下佩戴口罩3小时。该试验的结果如图5所示。
在没有皮肤保护的情况下,佩戴口罩导致摩擦和皮肤发炎,在颧骨的骨突上方和沿线有可见的红斑。2小时测试后,鼻梁上出现可见的皮肤发白区域。这一发现与现有的文献报告一致,即压力性损伤可在短短2小时内发生8,11。
在使用面部保护的情况下进行测试后,颧骨的骨突上方再次出现轻微红斑,仅在鼻子左侧出现少许发红。然而,在没有额外的摩擦或皮肤发炎区域存在的情况下,这些变化远不如之前明显,这表明在3小时内口罩的密合性良好,口罩移位极小。1小时后,所有红斑明显减轻。
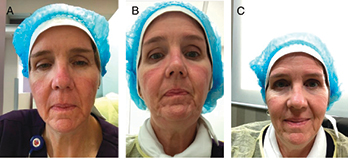
图5.A,无敷料佩戴口罩两小时后。B,有敷料佩戴口罩三小时后。C,移除敷料和摘除口罩后一小时(佩戴3小时)
阶段5
这项实验性测试连续两天进行,有5名志愿医护人员(1名男性和4名女性)参加,他们的皮肤类型在Fitzpatrick量表上属于从白皙到深棕色。研究人员推理,在女性中更易观察到皮损或皮肤损伤,因为女性的皮肤比男性薄18。如果使用所选方法保护了女性的皮肤,则可以合理地假设男性的皮肤也会得到保护。在本研究作者的环境中,女护士的人数也超过男护士,因此更有可能参与直接护理并需要保护。
在该阶段的第一天,每名受试者均佩戴了4个小时的N95口罩(不允许进食、饮水或上洗手间),且准备并使用了保护装备。舒适度由受试者自己进行评估。4小时结束时,有3名受试者认为可以再继续佩戴口罩一至两个小时。所有受试者的面部均轻微出汗并可观察到压痕。仅有一名受试者(Fitzpatrick 2型)出现轻微红斑;在最深色的皮肤上可观察到的损伤极小。
测试前后还采集了每名受试者的脉搏血氧饱和度水平。所有受试者在本次测试中损失1%~3%的Spo2,平均损失2%的代谢Spo2(表1)。这与关于N95口罩使用的现有研究相一致,该研究证实,即使佩戴完美密合的口罩,佩戴期间的总体摄氧量也会减少19,20。
表1.使用面部保护的4小时佩戴时间测试
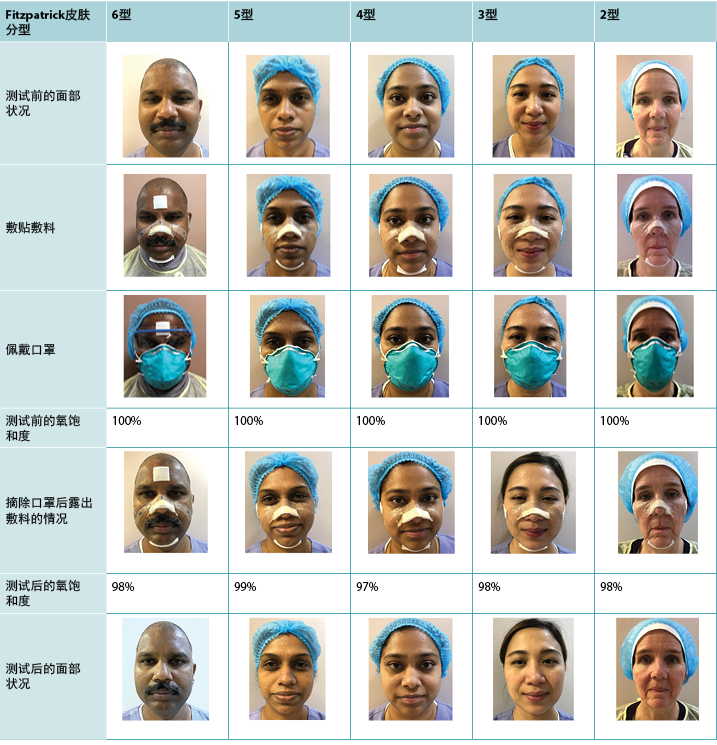
次日,受试者佩戴N95口罩,没有任何保护装备(表2)。每名受试者放置好口罩,并再次佩戴4小时,期间没有进食、饮水或上洗手间。所有四名女性受试者均感到不适;在第一小时后观察到口罩边缘出现皮肤瘙痒。所有受试者均报告称,当可以摘除口罩时,他们松了一口气;没有受试者希望继续再佩戴口罩一段时间。
表2.未使用面部保护的4小时佩戴时间测试
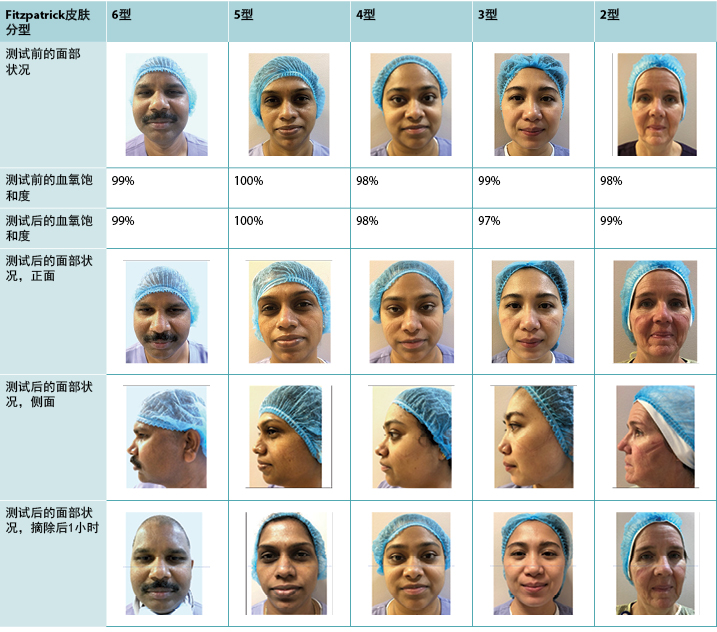
与前一天相比,可观察到较少的湿气积聚,但所有五名受试者的面部均有皮肤压痕。肤色较白的受试者似乎比肤色较深的受试者受到更多的压力相关影响。所有四名女性受试者均出现不同程度的皮肤红斑,其中白皙皮肤受损最为严重。肤色最深的受试者出现的可见损伤最少;可见一小块肤色变暗的区域,但在1小时内完全恢复。在女性受试者中,三名受试者在测试后1小时仍有压痕和红斑的体征,与前一天的结果相比,皮肤白皙的受试者的皮肤恢复最少。
关于第二天的代谢Spo2,三名受试者保留了完全相同的起始值,一名受试者增加了1%。其余受试者出现2%的Spo2损失。代谢性Spo2平均损失为0.2%。图6显示了两次4小时测试前后同一名受试者的Spo2读数。
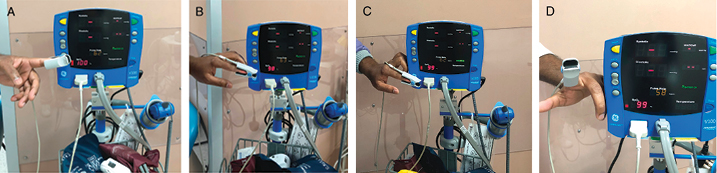
图6.脉搏血氧饱和度读数示例
A,4小时佩戴时间测试前,有面部保护(100%)。B,4小时佩戴时间测试后,有面部保护(98%)。C,4小时佩戴时间测试前,无面部保护
(99%)。D,4小时佩戴时间测试后,无面部保护(99%)。.
讨论
本文介绍了一种HCP预防面部皮肤损伤的整体方法,以“帮助”医护人员在高危的COVID-19环境中工作时拥有全面的自我照护方法。面部保护是这一安全举措的基石。
较长时间使用PPE时(每名受试者作为其自己的对照),在有保护和没有保护的情况下佩戴口罩产生了明显的差异,包括在不影响口罩气密性的情况下改善面部状况和舒适度。本实验发现了三种可能的损伤机制。第一种与导致皮肤压痕的直接高压有关(即,来自口罩边缘、鼻部密合装置和带子);第二种是与有或无摩擦力情况下的较低压力相关的直线型弥漫性红斑(即,口罩边缘移位)。在没有面部保护的情况下,两者均更为明显。第三种是与出汗有关:当使用皮肤保护装备时,口罩下的轻微局部出汗更为明显,这是因为获得的气密完整性更好。因此,这种PPE配置存在因汗水而产生相关湿气积聚的风险;因此,建议下班后的HCP使用丙烯酸护肤剂10,然后进行细致的面部护理9。
所有受试者均能轻松地将敷料剪成小块,并能借助镜子轻松地将敷料敷贴在面部。戴上这一保护层后,也可轻松建立起N95口罩的完整性,所有医护人员均通过了泄漏和密合性测试。
在疫情期间,一线医护人员最关键的安全考虑因素在于PPE的移除顺序;必须按照与其穿戴时完全相反的顺序脱下PPE1。上洗手间和进食不能计入轮班的时间,因为正确的以相反的顺序移除各层PPE比使用PPE需要更多时间,以防止造成污染和对医疗机构中的他人带来风险1,7。必须首先移除所有身体上穿戴的PPE,然后彻底洗手21,之后仅通过接触松紧带摘除N95口罩1,并且在移除面部保护性敷料之前重复洗手程序。实质上,如果医护人员在安全移除所有被污染的PPE之前就触摸自己的面部,会大大增加COVID-19自我污染的风险1。
这一严格的PPE程序要求医护人员深刻地意识到这一重要的安全防范措施,增强HELP使能器对下班时间补充充足营养和水分,以及在轮班前即刻限制过量液体摄入建议的关注。考虑到这些自我照护策略,4小时的禁食时间是可行的。关键是计划并将补充营养和补充水分活动调整为轮班后和/或轮班前不少于一小时前进行。患有疾病而不能坚持4小时禁食或不上洗手间的轮班的医护人员应被视为高危传染人群,不仅会为自己带来风险,也会为使用同一设施的其他人带来风险。
至少有一个医疗机构已经试行了这种方法,并取得了成功。在中国武汉7,一线医护人员在每4小时的轮班中均穿戴完整的PPE,禁止触摸口罩、进食、饮水和上洗手间。这一简单程序确保了没有医护人员感染COVID-197。他们的经验为本研究中进行的4小时佩戴测试提供了依据。
中国的一项关于HCP使用PPE时受到的面部损伤的不同横断面研究22(N=4,306),也发现这一4小时的临界时间。研究人员发现,如果HCP佩戴PPE的时间超过了这一时间范围,则受到损伤的医护人员人数会发生具有统计学意义的差异22。因此,口罩下的皮肤保护是必要的,因为基于PPE用品的轮班时间长度是不可预测的23,且在更短的轮班期中(本研究中为2小时内)已观察到面部损伤22。
至关重要的是,应记录PPE佩戴时间(无论是否使用面部保护)3,以防止长时间接触、过度的湿气积聚和皮肤皲裂。根据武汉市大力开展COVID-19一线护理的经验7,22,建议将每8小时的轮班分为两个小组,其中一个小组进行需要佩戴N95口罩的工作(在脏乱/感染区域),而其余的医护人员在洁净区域工作。在一组医护人员穿戴完整的PPE,且在无进食、饮水或上洗手间的情况下工作四小时后,两个小组进行交换。这可以防止疲惫和口罩导致的缺氧19,并保护HCP的皮肤7,22,对人员配置的影响极小。
本研究最有趣的发现是,当在N95口罩下使用保护性敷料时,受试者的Spo2值平均下降了2%。这与流感爆发期间进行的密合口罩佩戴研究的结果相一致19,20。这可能是保护性敷料增加了口罩的密封稳定性,同时减轻了压力相关性皮损。关键是,长时间佩戴N95口罩可能与HCP中口罩引起的缺氧有关19,20;缺氧是压力相关性皮肤皲裂的一个已确定的主要风险因素3。可通过前述的两班倒方法缓解这种担忧7,22。
单独使用N95口罩时,Spo2的降低结果并非如此。这可能表明,尽管通过了密合性和泄漏测试,但口罩佩戴带来的不适感仍导致受试者偶尔移动面部以缓解压力和面部刺激,这可能导致轻微泄漏。2型皮肤的受试者很有可能在测试过程中,在没有使用保护层的地方出现泄漏,该泄漏在测试过程中因嘴部、下巴和面部移动而持续存在。该受试者的Spo2增加了1%,测试后出现的皮损最为明显。
因此,口罩带来的不适感可能会增加感染COVID-19的医源性风险。同样的风险也适用于任何因面部损伤导致皮肤损伤的医护人员,因为疼痛可能会影响N95口罩的适当气密性。在现有的面部损伤处反复施加压力,有可能加重轻微损伤,导致更深部的真皮损伤;因此一旦出现1期压力性损伤时,就要小心地将患者的受压部位调整到身体的其他部位。3
局限性
本研究招募小样本量参与实验性项目,以确定使用面部保护层能否减轻N95口罩佩戴者的面部损伤风险。使用不同有边型敷料进行更多的研究将有利于扩展关于此主题的证据基础,并为医护人员提供更多的选择。
KHUH的医护人员也主要是西亚和东亚裔,因此缺少Fitzpatrick皮肤分型1型的护士作为受试者。这是一个主要局限性,因为这种皮肤类型通常对损伤和皮肤侵害最为敏感。此外,虽然Fitzpatrick量表是日光相关皮损的判据标准,但它可能无法完全预测皮肤上的压力和剪切力损伤,因为更深部的损伤可能不会立即显现。有必要在存在Fitzpatrick 1型皮肤HCP的医疗机构中进行进一步的测试。
还需要进一步研究N95口罩的佩戴以及Spo2降低对疲劳、头痛和注意力的影响,以确定皮肤风险、代谢压力和个人保护之间的最佳安全平衡。
结论
在COVID-19卫生危机的早期开始,KHUH就将保护HCP皮肤的需求列为优先事项。当时,没有可用的教育资源来指导实践。(此后,从2020年4月开始,发布了一些使能器24,25)本文中描述的创造性分步皮肤保护程序是使用现成产品和自愿帮助开发预防皮肤损伤安全解决方案的受试者开发的。
大约与每日外卖咖啡的成本相同,一块重新裁剪的无损伤硅酮有边型敷料可在密合的口罩下保护皮肤健康。通过将其切为小片,并小心、无皱褶地贴在鼻子、颧骨和面部两侧,HCP可以获得压力再分布和面部皮肤保护。这种方法似乎不会影响N95口罩的完整性,事实上,通过更牢固地固定口罩的位置,可以提供额外的泄漏保护,最终防止病毒意外转移到面部1。因此,作者们建议HCP使用无损伤硅酮有边型敷料,作为在PPE下保护面部皮肤的安全且有益的选择。
然而,任何敷料本身(无论测试如何)都不能为N95口罩下的面部皮肤提供完全的护理。HCP实施全面的皮肤护理方法至关重要。一线医护人员如果能通过有责任心地进行自己的皮肤护理来“帮助”自己,以及做好充分准备、充分休息、进食和补充水分,可以更安全地照护他人。
作者希望,这一创造性的循证面部保护临床解决方案和HELP使能器能对全球同仁对抗COVID-19的工作有所帮助。
利益冲突
作者声明没有利益冲突。
资助
作者在本研究中未收到任何资助。
Author(s)
Hiske Smart*, RN, MA (Nur), PG Dip WHTR, IIWCC
Manager, Wound Care and Hyperbaric Unit, King Hamad University Hospital, Kingdom of Bahrain
Email hiskesmart@gmail.com
Francis Byron Opinion, RN, MAN (UP), ADON
Assistant Director of Nursing, Quality, Research and Informatics Division, King Hamad University Hospital, Kingdom of Bahrain
Issam Darwich, RN, BSc
Manager, Emergency Department, King Hamad University Hospital, Kingdom of Bahrain
Manal Aly Elnawasany, RN, BSc
Infection Control Nurse, Infection Prevention and Control Team, King Hamad University Hospital, Kingdom of Bahrain
Chaitanya Kodange, MBBS, MD(Psy), DMM, DHA, IIWCC
Consultant, Wound Care and Hyperbaric Unit, King Hamad University Hospital, Kingdom of Bahrain
* Corresponding author
References
- World Health Organization. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19). Interim guidance. March 19, 2020. https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf. Last accessed May 26, 2020.
- Kingdom of Bahrain. Public Awareness Campaign to Combat Coronavirus. Coronavirus (COVID 19) latest updates. 2020. www.moh.gov.bh/?lang=en. Last accessed May 27, 2020.
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Advisory Panel. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. Emily Haessler, ed. 3rd ed. EPUAP/NPIAP/PPPIA; 2019.
- Radovic T, Manzey D. The impact of a mnemonic acronym on learning and performing a procedural task and its resilience toward interruptions. Front Psychol 2019;10:2522.
- Voegeli R, Gierschendorf J, Summers B, Rawlings AV. Facial skin mapping: from single point bio-instrumental evaluation to continuous visualization of skin hydration, barrier function, skin surface pH, and sebum in different ethnic skin types. Int J Cosmet Sci 2019;41(5):411-24.
- Little MO. Nutrition and skin ulcers. Curr Opin Clin Nutr Metab Care 2013;16(1):39-49.
- Chen W. Protection of medical team in Wuhan. March 26, 2020. www.academia.edu/42406953/Protection_of_Medical_Team_in_Wuhan. Last accessed May 26, 2020.
- Woo K. Using multi-layer foam dressing to prevent pressure injury in a long-term care setting. Surg Technol Int 2018;32:75-7.
- Vollmer DL, West VA, Lephart ED. Enhancing skin health: by oral administration of natural compounds and minerals with implications to the dermal microbiome. Int J Mol Sci 2018;19(10):3059.
- Ogawa-Fuse C, Morisaki N, Shima K, et al. Impact of water exposure on skin barrier permeability and ultrastructure. Contact Dermatitis 2019;80(4):228-33.
- Santamaria N, Gerdtz M, Kapp S, Wilson L, Gefen A. A randomized controlled trial of the clinical effectiveness of multi-layer silicone foam dressings for the prevention of pressure injuries in high-risk aged care residents: the Border III Trial. Int Wound J 2018;15(3):482-90.
- Serra R, Ielapi N, Barbetta A, de Franciscis S. Skin tears and risk factors assessment: a systematic review on evidence-based medicine. Int Wound J 2018;15(1):38-42.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol 1988;124(6):869-71.
- Lee SA, Hwang DC, Li HY, Tsai CF, Chen CW, Chen JK. Particle size-selective assessment of protection of European standard FFP respirators and surgical masks against particles-tested with human subjects. J Healthc Eng 2016;2016:8572493.
- Kansas Department of Health and Environment. Fit testing procedures for N95 respirators (using 3M FT-30, Bitter Fit Test Equipment). 2020. www.kdheks.gov/cphp/download/Fit_Test_Pro_for_N95_R.pdf. Last accessed May 27, 2020.
- Singapore General Hospital. N95 3M mask fit: how to wear and remove. YouTube. September 16, 2015. https://youtu.be/zoxpvDVo_NI. Last accessed June 9, 2020.
- UNMC Heroes, N95 respirator limited reuse - Health Care Professionals Providing Clinical Care. YouTube. 2020. https://youtu.be/Cfw2tvjiCxM. Last accessed June 9, 2020.
- Rahrovan S, Fanian F, Mehryan P, Humbert P, Firooz A. Male versus female skin: what dermatologists and cosmeticians should know. Int J Womens Dermatol 2018;4(3):122–30.
- Beder A, Büyükkoçak U, Sabuncuoğlu H, Keskil ZA, Keskil S. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia (Astur) 2008;19(2):121-6.
- Tong PS, Kale AS, Ng K, et al. Respiratory consequences of N95-type mask usage in pregnant healthcare workers—a controlled clinical study. Antimicrob Resist Infect Control 2015;4:48.
- Dietz L, Horve PF, Coil DA, Fretz M, Eisen JA, van den Wymelenberg K. 2019 Novel coronavirus (COVID-19) pandemic: built environment considerations to reduce transmission. mSystems 2020;5(2):e00245-20.
- Jiang, Q, Song S, Zhou J, et al. The prevalence, characteristics, and prevention status of skin injury caused by personal protective equipment among medical staff in fighting COVID-19: a multicenter, cross-sectional study. Adv Wound Care 2020;9(7).
- World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortage. Interim guidance. April 6, 2020. https://apps.who.int/iris/bitstream/handle/10665/331695/WHO-2019-nCov-IPC_PPE_use-2020.3-eng.pdf. Last accessed May 27, 2020.
- LeBlanc K, Heerscap C, Butt B, Bresnai-Harris J. Prevention and management of skin damage related to personal protective equipment (PPE). April, 7 2020, Webinar for Continuing Education. Meeting Id 8991745363. Canadian seminar.
- National Pressure Injury Advisory Panel. NPIAP Position statements on preventing injury with N95 masks. April 15, 2020. https://cdn.ymaws.com/npiap.com/resource/resmgr/position_statements/Mask_Position_Paper_FINAL_fo.pdf. Last accessed May 20, 2020.


