Volume 43 Number 4
Prevention of kinking in percutaneous tubes
Sivagame Maniya, Ma V Gonzalves, Nurashiqin B Saadan
Keywords tube care, catheter care, tube protector, percutaneous
For referencing Maniya S, Gonzalves MV & Saadan NB. Prevention of kinking in percutaneous tubes. WCET® Journal 2023; 43(4):27-31.
DOI
10.33235/wcet.43.4.27-31
Submitted 19 January 2023
Accepted 27 November 2023
Abstract
Introduction Percutaneous tubes (PTs) allow permanent or temporary drainage or relieve obstruction caused by blockages or abnormal narrowing of openings or ducts. There is risk of PT kinking due to rotation and bending of the soft tube at the distal end during movement. Despite anchoring and dressing, indentation of the tubing occurrence results in impeded flow of fluid that may lead to infection risk. Aside to discomfort and pain, patients will likely require medical intervention and longer hospital admission. An average of 9–10 cases per month of PT damage were reported in our department.
Aims To explore solutions to minimise the incidence of PT damage and reduce the occurrence of PT kinking.
Methods A quality improvement (QI) team conducted root cause analysis to identify causes for the prevention and management of PT kinking. A modified fishbone framework identified root causes and possible interventions. The number of kinking in PTs was monitored.
Results Lack of training in staff to manage PT, the absence of standardised way of dressing, and the soft material-based tube were three major causes identified. Intensive education with a training video for the nurses and a standardised method of dressing application reference guide over the PT were initiated. A non skin-irritant conformable gadget was applied to protect the PT. The incidence of PT kinking dropped within the first month of implementation of the solution.
Conclusion Patients with long-term PTs/catheters can benefit from the use of an inexpensive efficacious protector to prevent damage to their PTs.
Introduction
Percutaneous tube (PT) insertion is a minimally invasive well-established procedure in which a catheter is inserted through a skin puncture into an organ such as the kidney or liver for diagnostic and therapeutic purposes1 to allow permanent or temporary drainage of urine, bile or abscess. PT insertion also relieves obstruction caused by blockage or abnormal narrowing of the ureter or bile duct and is used to drain abscesses2. This procedure reportedly reduces morbidity and mortality compared to open surgical drainage procedures, especially in critical ill or high surgical risk patients3. Although procedural complications are uncommon, the management of PT drainage-related complications can have adverse consequences that lead to increased length of stay and associated raised healthcare costs3.
Lorenz and Thomas4 have discussed procedure-related complications and strategies to prevent or reduce these occurrences. Aside from procedural-related complications, blockage and slippage of PTs are commonly reported PT complications5,6. Further, while the soft material of the PT facilitates patient comfort, there is the risk of kinking. Rotation and bending of the PT at the distal end are most common observations on drainage PTs. Sdrales and Benumof7 defined kinking of a PT as the touching of diametrically opposite sides of the plastic catheter alone at a point of sharp curvature, observed visually. This twisting and bending of the PT may cause temporary kinking and/or permanent indentation of the tubing, resulting in the flow of fluid in the PT being impeded. PT kinking can lead to increased risk of infection and septicaemia that may require high dependency or intensive care admission. With total catheter failure, patients will require reinsertion of a new PT and treatment of potential or actual infection. Aside from experiencing additional discomfort and pain, those patients who require further medical intervention will endure a longer hospital admission.
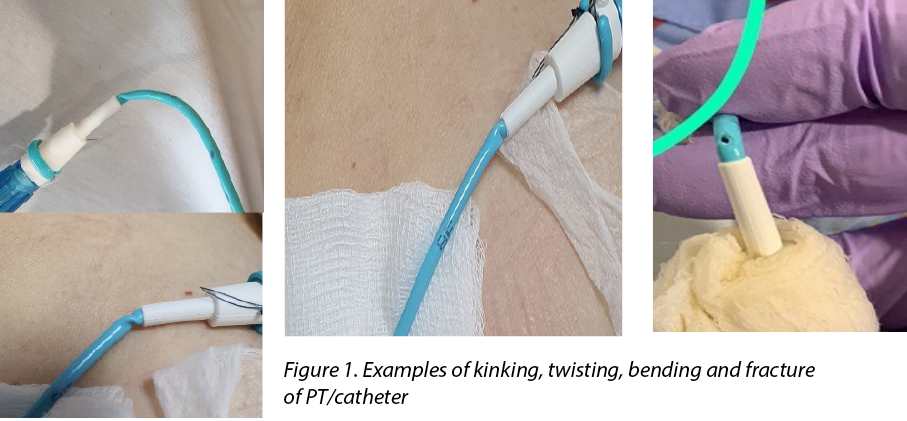
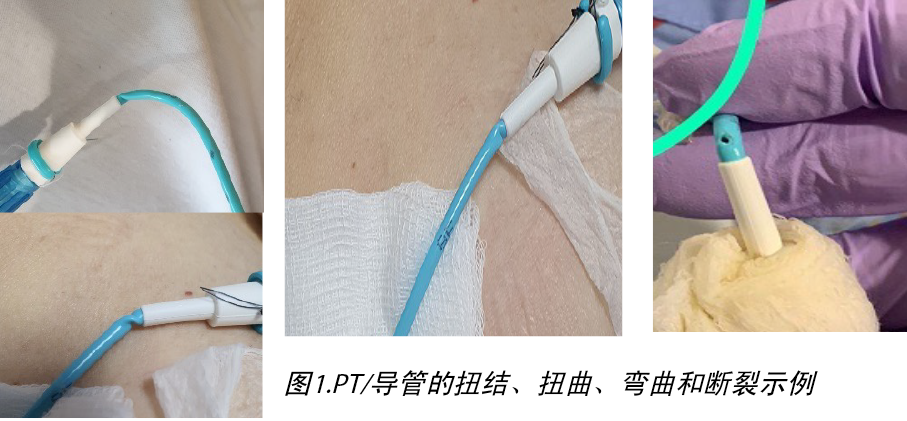
The patency of nephrostomy PTs should be always maintained to ensure adequate flow and drainage of urine. Although care of nephrostomy PTs often focuses on proper anchoring and dressing, the PT may still twist and bend during patient movement and positioning. Complications such as kinking and prevention of PT fractures are rarely discussed or reported as being observed. Turo et al.8 reported the incidence of nephrostomy PT-related complications such as fracturing, kinking and blockage was 6.1% in 66 patients in their study. Figure 1 shows the types of kinking which are most likely to occur at the distal end of the catheter. Kinking results in twisting and bending of the PT, which will eventually fracture, tear and leak and become a portal for infection.
The care of the PT is a fundamental aspect of surgical nursing. Martin and Baker9 emphasised, in addition to suturing the PT in position on the skin, the importance of dressings over the exit site of nephrostomy PTs in consideration of patient comfort and prevention of infection. As the exit site for drainage can be inserted at a challenged anatomical site, body movements or positions may cause discomfort and dislodgement. Commercialised drain-specific dressings or simple gauze-tape methods can support the PT to prevent unintentional tugging and secures it over the patient’s skin9,10.
The SKATER™ drainage catheters are designed for easy insertion and patient comfort, while ensuring effective drainage flow. Within our hospital, these PTs inserted by an interventional radiologist (IR) for drainage procedures are small in diameter and flexible. Post-insertion, the ward nursing staff would keep and monitor the IR-placed dressing. Dressings over the exit sites were changed every 3 days or as per required when soaked or stained.
Although the manufacturing company claims a kink-resistance quality to the SKATER™ drainage tube, the nature of the PT’s soft material may be another contributing factor to potential twisting. An observation of PT kinking/twisting incidence over the distal end of the PT and the hub connection resulting in PT fracture, was noted in our department (Figure 2). An average of 9–10 cases per month in nephrostomy PTs, biliary and abscess drains were reported over a 3-month period. However, the authors found limited literature discussing strategies regarding the prevention of kinking in PTs.
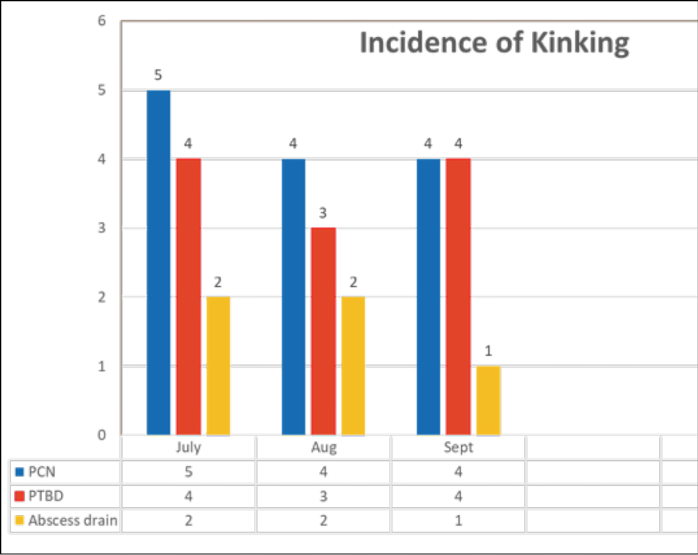
Figure 2. Incidence of kinking in PTs/catheters
A quality improvement (QI) project was embarked upon, aiming to explore solutions to minimise the incidence of PT damage and to reduce the occurrence of PT kinking in our patient population in general surgical wards of our hospital within a 6-month period.
Methods
The nursing team was formed to brainstorm possible causes and solutions. The team brainstormed the problem using a fishbone concept to identify the root causes of PT kinking. The fishbone concept or Ishikawa diagram11 is an effective authenticated framework to brainstorm potential causes of problems, narrow the root causes, mind-mapping the quality issues to focus on problem solving. As this was a QI study with no invasive patient interventions, separate ethical clearance from our hospital ethics committee was not required.
In the root cause analysis (Figure 3), the members identified three major causes of PT kinking: the lack of training and knowledge in managing PTs among staff; the absence of a standardised way of applying a protective/anchoring dressing and; the likelihood that the soft material used in PT manufacture will kink with body movement.
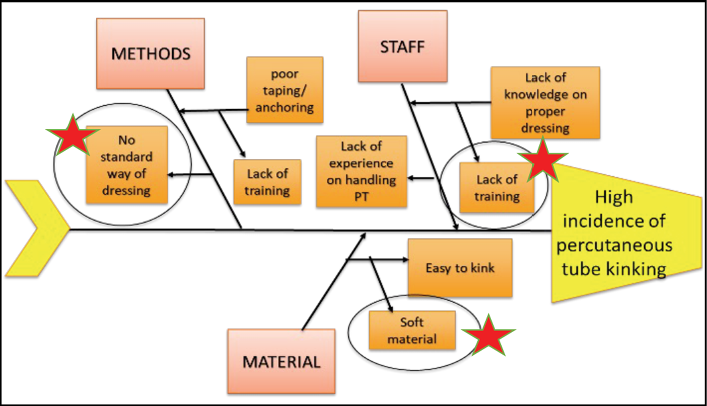
Figure 3. Root cause analysis
The pilot project was implemented in five general surgical wards over a period of 6 months. Each of the three causative problems were addressed using brainstorming strategies.
Staff lack of training in managing PTs
Proposed intervention: A training video on PT dressing steps was disseminated to the ward nurses. Following comprehensive in-service and dissemination of the training video, the nurses were surveyed on their knowledge of managing PTs (Figure 4). Responses from survey were analysed: 83.3% (n=60) answered they were still not confident in managing PTs, particularly dressing and anchoring.
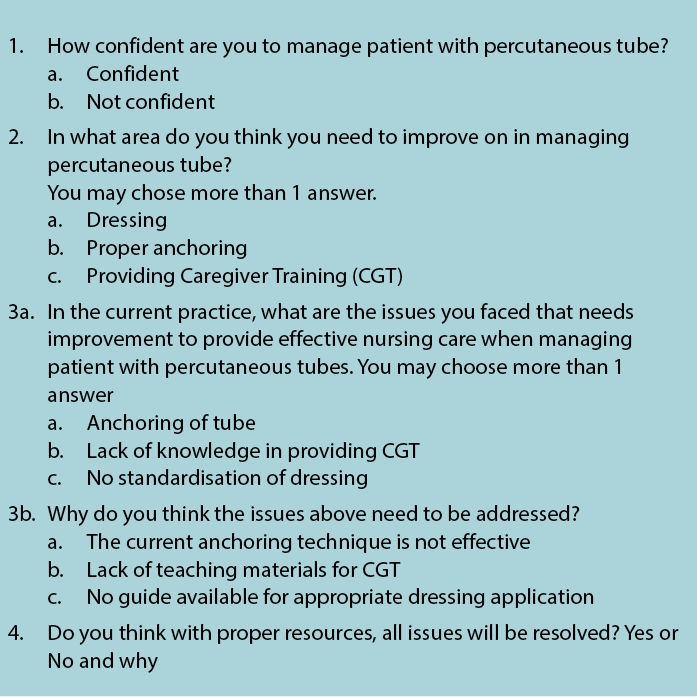
Figure 4. Nurses’ survey
The QI team also developed a quick reference guide (Figure 5) as a resource for the nurses to resolve this. However, kinking of PTs was still observed.
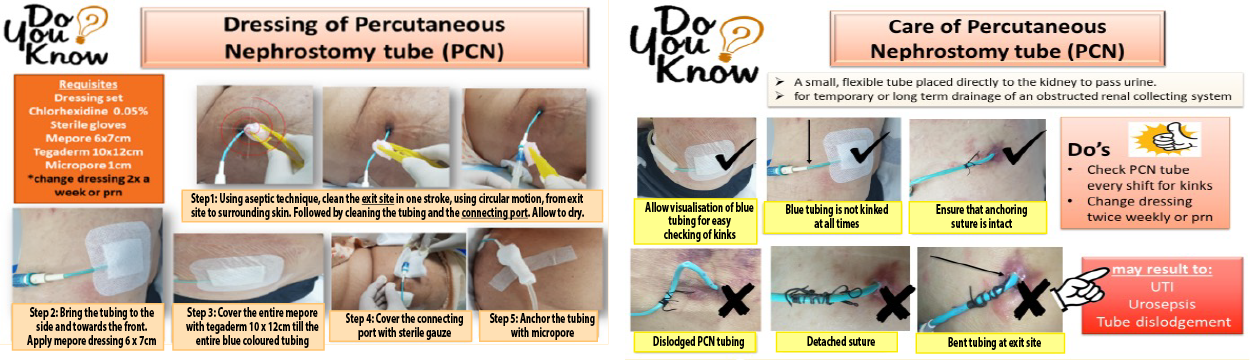
Figure 5. Nurses’ resource guide
Lack of standardised way of dressing application over the PT
Proposed intervention: different methods of dressing and anchoring were explored (Figure 6). A non-adherent island over the exit site and film dressing over the tubing (a) was applied. The second method was a large non-adherent island dressing (b) that covered both the exit site and the tubing; this was considered to stabilise the tubing. The third method was to use the commercial Grip-Lok securement device (c), which is commonly to secure urine catheters. This was applied in addition to the conventional dressing over the exit site in order to stabilise the area prone to kinking.
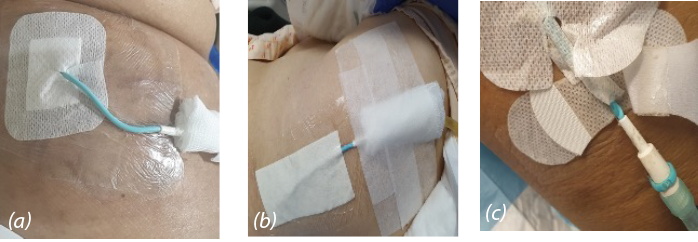
Figure 6. Dressing for anchoring
a) Non-adherent island and film dressing
b) Non-adherent island dressing
c) Grip-Lok securement device
Although the non-adherent island and film dressing were readily available, kinking of the PT persisted at the distal end of the tubing. Likewise, despite the use of the Grip-Lok securement device, twisting of the tubing was still observed. The additional cost of the Grip-Lok securement device at S$3.00 was another disadvantage to consider.
Likelihood of soft material kinking with body movement
Proposed intervention: the team proposed a PT stabiliser, an idea inspired from cable protectors that could protect the soft material tubing from kinking and twisting. The PT-protector (PTP) (Figure 7) was made with non skin-irritant thermoplastic polyurethane material; it was flexible yet durable. The conformable PTP could be removed for cleaning and reapplied. The cost of the protector is minimal at 16 cents. The infection control department was consulted to discuss options of disinfection vs sterilisation. Aligned with the Spaulding classification12, alcohol 70% can be used to disinfect the PTP before application and during each dressing change, or as deemed necessary.

Figure 7. Tube protector
Utilising the three interventions of staff training, improved standardised dressing application and PTP in conjunction with one another further education and training was conducted demonstrating the improved dressing method of management and the PTP application. The quick reference guide was revised and uploaded to the hospital education website for nurses to easily access. The effectiveness of PTP with a standardised dressing (Figure 8) in preventing kinking of PT was monitored.
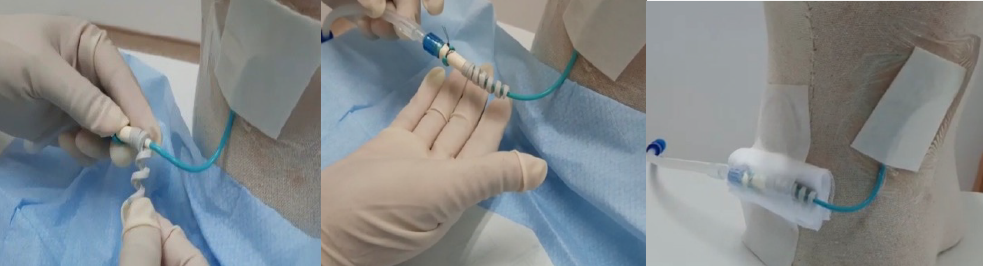
Figure 8. PTP application with standardised gauze dressing
Results
The interventions were implemented on 100 patients with PTs or drains in five surgical wards. The incidence of PT kinking in nephrostomy PTs, biliary and abscess drains significantly dropped within the first month of implementation (Figure 9). One incident of PT bending was reported on the 3rd month post-implementation which was attributed to an improper anchoring technique. Subsequently, nil numbers of kinking/ bending/twisting were observed in the next 3-month period of monitoring. The PTP device was effective in stabilising PT to prevent kinking. This initiative of PTP, together with proper anchoring and regular staff compliance audits, resulted in zero incidence of PT kinking from the month of implementation to date. At the 3-month follow-up, no primary PT infection was reported nor was any secondary infection as a result of the use of the PTP.
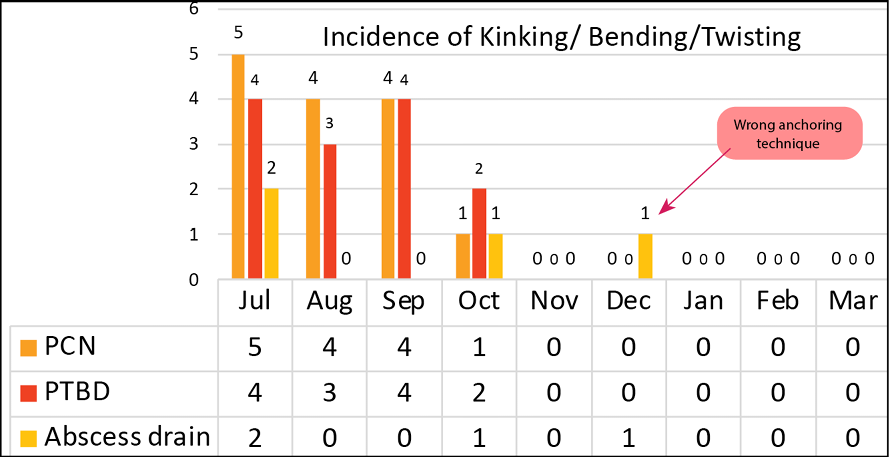
Figure 9. Effectiveness of PTP
Discussion and implications for practice
Although most of the literature2–6,8 combined major and minor complications from PT placement or procedures related such as injury to adjacent structures, severe bleeding or severe infection, we found limited publications discussing the incidence or complications arising from PT kinking as result of care of PTs. However, PT kinking can impede drainage or result in fractures or tears, leading to leakage of contents13. As these PTs are placed for a period of duration and managed in the home care environment, correct care of the PT is imperative. Furthermore, while a soft material-based tubing is ideal for patient comfort, the pliability may have a disadvantageous potential for kinking with patient movement or positioning.
Our team believe that this is a great milestone for maintaining the target of zero-harm for patients with PT. It is recommended that staff should perform regular checks for kinking over the PT site once every shift. Nurses need to be knowledgeable on what to look out for and monitor when handling patients with PTs. Nurses play a vital role in ensuring that all patients with a PT in our facility have had a PTP device and the standardised dressing applied to prevent the incidence of PT kinking. We also recommended judicious change of the PTP weekly and cleansing of the device with alcohol 70% routinely as per the Spaulding classification process.
A reference guide for nurses was also useful to elaborate the steps of applying the PTP, with the aim of reinforcing the practice. This simple guide with illustrations was used to educate and train nurses for better understanding and compliance. A copy of the reference guide was available to the nurses on the institution’s intranet. Compliance with the use of the PTP device and the standardised dressing application was also reviewed through adhoc audits and reinforcement training.
It is proposed that the incidence of PTP-related PT exit site infection can be monitored as a follow-up study to evaluate the safety and efficacy of PTP. The following potential outcomes for patients that could be measured are decreased length of stay, the need for antibiotics use, re-insertion of PTs, and avoidance of readmissions of patients discharged with PTs.
The success of this project was shared with the surgeons at the hospital’s department meeting platform. The PTP concept was subsequently considered for other types of soft material-based drainage PTs or catheters. Project outcomes were also shared at the local healthcare QI conference platform with other hospitals. The project team are also considering developing an educational video on the care of drainage catheters.
Conclusion
Subsequent follow-up monitoring of data post-implementation of the PTP device and standardisation of dressings to secure the PT reported no incidence of PT kinking or damage. This QI project benefited patients with long-term drainage PTs/catheters; the use of this inexpensive and efficacious method prevents damage to PTs or catheters that potentially leads to complications and increased duration of hospitalisation. Further, it can be assumed that there were facility and cost efficiencies from fewer infections, dressing procedures and replacements of PTs from kinking.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
防止经皮导管扭结
Sivagame Maniya, Ma V Gonzalves, Nurashiqin B Saadan
DOI: 10.33235/wcet.43.4.27-31
摘要
引言 经皮导管(PT)可实现永久性或暂时性引流,或可缓解开口或导管堵塞或异常狭窄引起的阻塞。由于移动过程中远端软管的旋转和弯曲,存在PT扭结风险。虽然进行了固定并使用了辅料,但管路凹痕仍会导致液体流动受阻,从而引发感染风险。除不适和疼痛外,患者可能需要接受医疗干预和延长住院时间。我所在的科室平均每月报告9-10例PT损伤病例。
目的 探索尽可能降低PT损伤发生率和减少PT扭结发生的解决方案。
方法 由质量改进(QI)团队进行根本原因分析,以确定预防和管理PT扭结的原因。通过改良的鱼骨框架确定了根本原因和可能的干预措施。对PT中的扭结数量进行了监测。
结果 确定的三大原因分别为工作人员缺乏PT管理相关培训、缺乏标准化辅料应用方法以及柔性材料导管。通过为护士播放培训视频和针对PT使用标准化辅料应用方法参考指南,开始进行强化教育。使用非皮肤刺激性适形性工具保护PT。在实施该解决方法的第一个月内,PT扭结发生率有所下降。
结论 置入了长期PT/导管的患者可使用廉价有效的保护套预防其PT损伤,进而从中获益。
引言
经皮导管(PT)插入术是一种成熟的侵入性手术,通过皮肤穿刺将导管插入肾脏或肝脏等器官,用于进行诊断和治疗1,以实现永久性或暂时性尿液、胆汁或脓肿引流。PT插入术还可缓解输尿管或胆管堵塞或异常狭窄引起的阻塞,并可用于脓肿引流2。据报告,与开放性外科引流术相比,经皮导管插入术可降低发病率和死亡率,尤其是在重症或高手术风险患者中3。虽然手术并发症并不常见,但PT引流相关并发症的管理可能产生不良后果,导致住院时间延长和相关医疗费用増加3。
Lorenz和Thomas4讨论了手术相关并发症以及预防或减少发生此类事件的策略。除手术相关并发症外,PT堵塞和滑脱是常报告的PT并发症5,6。此外,虽然PT使用的柔性材料提高了患者舒适度,但仍存在扭结风险。PT远端旋转和弯曲是引流PT最常见的观察结果。Sdrales和Benumof7将PT扭结定义为目视观察到塑料导管截然相反的对侧仅在小曲率点接触。此类PT扭曲和弯曲可能造成暂时性管路扭结和/或永久性凹痕,导致PT中的液体流动受阻。PT扭结可増加感染和败血症风险,可能使患者具有高依赖性或入住重症监护病房。导管完全失效后,患者将需要重新插入新的PT并接受潜在或实际感染治疗。除了经历额外的不适和疼痛外,那些需要进一步医疗干预的患者的住院时间将延长。
应始终保持肾造瘘PT通畅,以确保充分的尿液流动和引流。虽然肾造瘘PT的护理通常侧重于适当的固定和敷料应用,但在患者移动和定位过程中,仍可能发生PT扭曲和弯曲。与观察到的并发症(如扭结和预防PT断裂)相关的讨论或报告较少。Turo等人8报告了其所研究的66例患者中肾造瘘PT相关并发症(如断裂、扭结和堵塞)的发生率为6.1%。导管远端最可能发生的扭结类型见图1。扭结导致PT扭曲和弯曲,最终导致导管断裂、撕裂和泄漏,成为感染源。
PT护理是手术护理的基本方面。Martin和Baker9强调,除了在皮肤上原位缝合PT外,考虑到患者舒适度和感染预防,在肾造瘘PT出口部位应用敷料十分重要。由于可以在具有挑战性的解剖部位插入引流出口,身体运动或定位可能造成不适和导管移位。市售的特定引流敷料或简单的纱布胶带方法可以用于支持PT,防止意外牵拉并将其固定在患者的皮肤上9,10。
SKATER˛引流导管的设计便于插入,且患者舒适度较高,同时还可确保有效的引流流量。在我们医院内,由介入放射科医生(IR)插入用于引流手术的这类PT直径较小且具有柔韧性。插入后,病房护理人员将保留并监测IR放置的敷料。出口部位的敷料每3天更换一次,或在浸湿或染色时按要求更换。
虽然制造公司声称SKATER˛引流管具有抗扭结性,但PT所用的柔性材料的性质可能是潜在扭曲的另一个促成因素。在我所在科室观察到了PT远端和连接器连接部分发生PT扭结/扭曲的事件,导致PT断裂(图2)。在3个月期间,每月平均报告9-10例肾造瘘PT、胆道和脓肿引流病例。但是,作者发现讨论PT扭结预防策略的文献较少。
启动了质量改进(QI)项目,旨在探索6个月内尽可能减少我院普通外科病房患者人群PT损伤发生率和降低PT扭结发生率的解决方案。
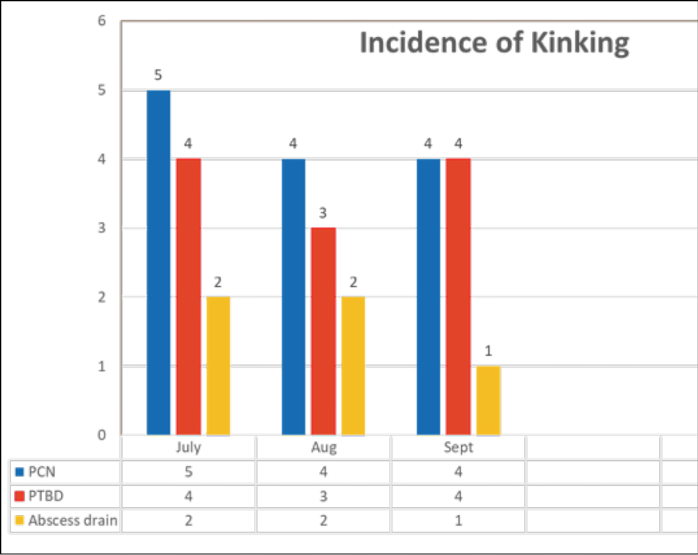
图2.PT/导管扭结的发生率
方法
成立了护理团队,他们进行头脑风暴以确定可能的原因和解决方案。该团队使用鱼骨图进行头脑风暴来解决该问题,以确定PT扭结的根本原因。鱼骨图或石川图11是一个经认证的有效框架,可用于进行头脑风暴以确定问题的潜在原因,缩小根本原因范围,通过思维导图确定质量问题,进而专注于解决问题。由于这是一项QI研究,无侵入性患者干预,因此无需获得我院伦理委员会的单独伦理许可。
在根本原因分析中(图3),成员确定了PT扭结的三个主要原因,具体如下:工作人员缺乏PT管理相关培训和知识;缺乏标准化保护/固定敷料应用方法;PT生产中使用的柔性材料可能会随身体运动而出现扭结。
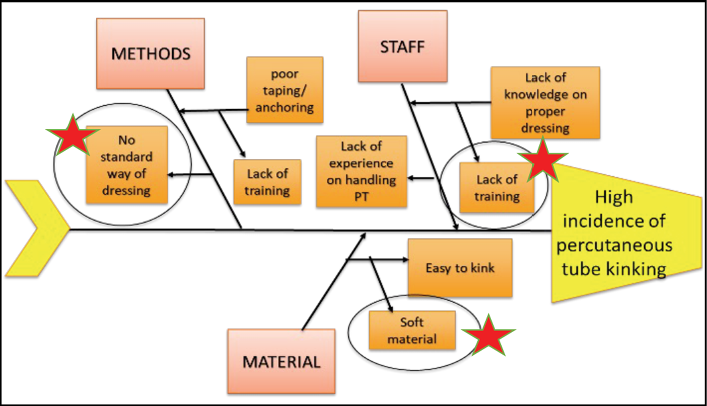
图3.根本原因分析
在5个普通外科病房执行了试点项目,为期6个月。使用头脑风暴策略解决三个致病问题中的任何一个问题。
工作人员缺乏PT管理培训
拟定干预:向病房护士发送了关于PT敷料应用步骤的培训视频。在经过全面在职培训并发送培训视频后,调查护士对PT管理知识的掌握情况(图4)。对调查的回复进行了分析:83.3%(n=60)的受访者表示他们在管理PT方面仍然缺乏信息,尤其是敷料应用和固定。
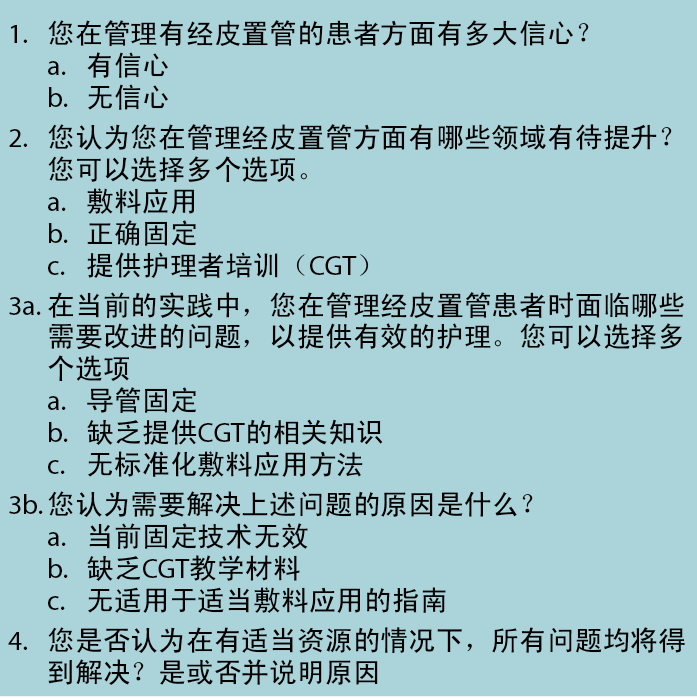
图4.护士调查
QI团队还开发了快速参考指南(图5),用作护士解决该问题的资源。但是,仍观察到PT扭结。
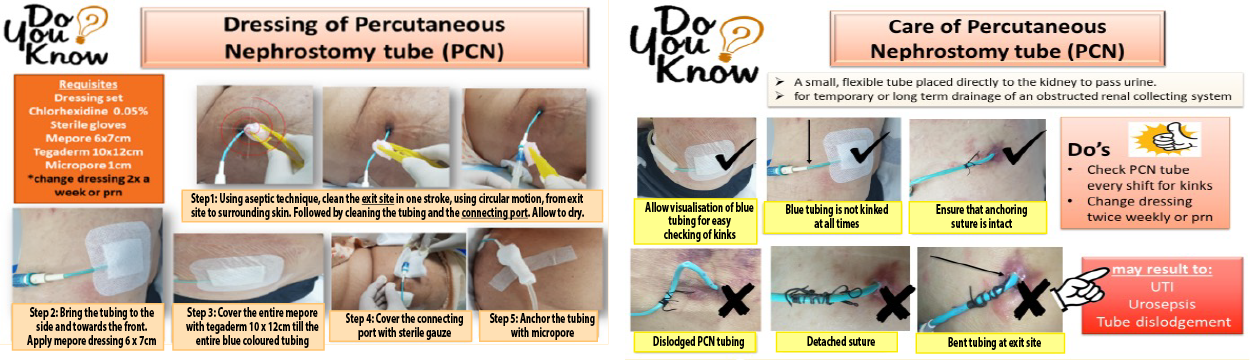
图5.护士资源指南
缺乏标准化PT敷料应用方法
拟定干预:探索了不同的敷料应用方法和固定方法(图6)。在出口部位应用非粘性岛状敷料,并在管路上应用薄膜敷料(a)。第二种方法是在出口部位和管路上覆盖较大非粘性岛状敷料(b);认为这种方法可稳定管路。第三种方法是使用市售Grip-Lok固定装置(c),通常用于固定导尿管。除了在出口部位使用常规敷料外,还使用了上述方法,以稳定易发生扭结的区域。
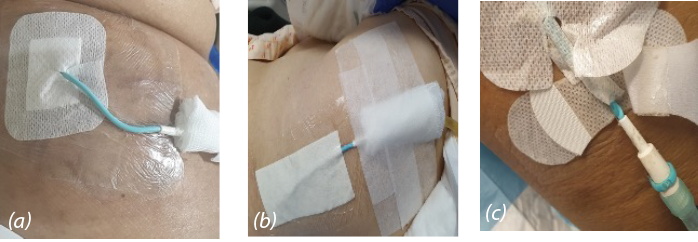
图6.固定用敷料
a)非粘性岛状敷料和薄膜敷料
b)非粘性岛状敷料
c)Grip-Lok固定装置
虽然非粘性岛状敷料和薄膜敷料随时可用,但管路远端仍持续出现PT扭结。同样,虽然使用了Grip-Lok固定装置,但仍观察到管路扭曲。Grip-Lok固定装置的额外成本为3.00新加坡元,这是需要考虑的另一个缺点。
身体运动时柔性材料扭结的可能性
拟定干预:团队建议使用PT稳定器,这一想法的灵感来源于电缆保护套,其可以保护柔性材料管路不发生扭结和扭曲。PT保护套(PTP)(图7)由非皮肤刺激性热塑性聚氨酯材料制成;具有柔韧性和耐久性。可取出适形性PTP进行清洁并重新应用。保护套的成本最低为16美分。咨询了感染控制科,讨论是选择消毒还是灭菌。与Spaulding分类一致12,在应用前和每次更换敷料期间或必要时,可使用70%乙醇对PTP进行消毒。

图7.导管保护套
通过工作人员培训、改进的标准化敷料应用方法和PTP这三项干预措施的相互配合,开展了进一步的教育和培训,展示了改进后的敷料管理方法和PTP应用。对快速参考指南进行了修订,并上传至医院教育网站,方便护士查阅。对采用标准化敷料(图8)的PTP预防PT扭结的有效性进行了监测。
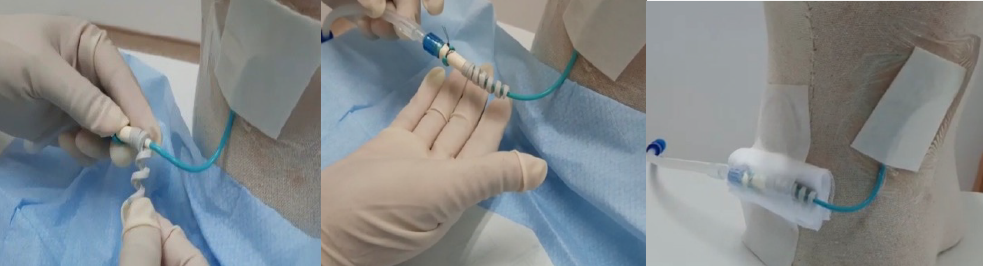
图8.使用标准化纱布敷料应用PTP
结果
在五个外科病房对100例使用PT的患者或引流患者实施干预。在实施干预的第一个月内,肾造瘘PT、胆道和脓肿引流的PT扭结发生率显著下降(图9)。在实施后第3个月报告了1例PT弯曲事件,归因于固定技术不当。随后,在接下来的3个月监测期内未观察到扭结/弯曲/扭曲。PTP装置可有效稳定PT,防止扭结。采用PTP的这一措施,加上适当的固定和定期工作人员合规性稽查,使得迄今为止PT扭结的发生率为零。在3个月随访时,未报告原发性PT感染,也未报告使用PTP导致的任何继发性感染。
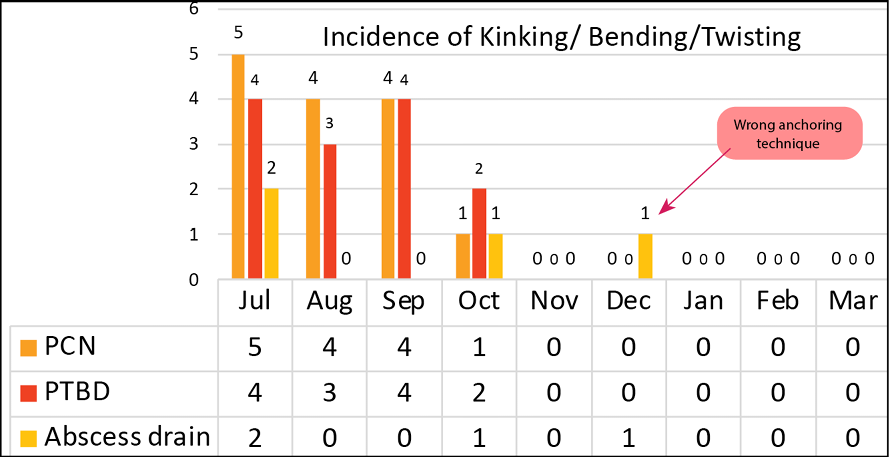
图9.PTP的有效性
讨论和实践启示
虽然大多数文献2-6,8均综合阐述了PT置入或手术相关的重大和轻微并发症,如邻近结构损伤、严重出血或严重感染,但我们发现讨论PT护理导致PT扭结的发生率或并发症的出版物较少。然而,PT扭结可阻碍引流或导致导管断裂或撕裂,进而造成内容物泄漏13。由于这些PT放置了一段时间并在家庭护理环境中进行管理,因此必须对PT进行正确护理。此外,虽然使用基于柔性材料的管路是确保患者舒适度的理想选择,但是柔韧性可能导致患者移动或定位过程中易出现扭结。
我们的团队相信,这对于保持使用PT患者的零伤害目标是一个重要的里程碑。建议工作人员每班一次定期检查PT部位的扭结情况。护士需要了解在处理使用PT的患者时应注意和监测的事项。通过确保本机构中所有使用PT的患者均使用了PTP装置和标准化敷料,可以预防发生PT扭结,而护士在这方面发挥着重要作用。我们还建议每周合理更换PTP,并根据Spaulding分类过程定期使用70%乙醇清洁该装置。
护士参考指南也很十分有用,其详细说明了应用PTP的步骤,旨在加强实践。这份带有插图的简明指南用于教育和培训护士,使其更好地理解并遵守规定。该机构的内联网还向护士提供了一份参考指南。还通过临时稽查和强化培训审查了PTP装置和标准化敷料应用的合规性。
建议可开展随访研究,监测PTP相关PT出口部位感染的发生率,以评价PTP的安全性和有效性。可衡量的患者潜在结局如下,包括住院时间缩短、需要使用抗生素、重新插入PT和避免出院时使用了PT的患者再次入院。
在医院的科室会议平台上,与外科医生分享了这一项目的成功经验。随后,针对其他类型的基于柔性材料的引流PT或导管考虑了PTP概念。同时,还在当地医疗保健QI会议平台上与其他医院分享了项目成果。项目团队还在考虑制作一部关于引流导管护理的教育视频。
结论
使用PTP装置和标准化敷料固定PT后,对数据进行的后续随访监测未报告PT扭结或损坏。该QI项目为使用长期引流PT/导管的患者带来获益;使用这种廉价有效的方法可防止PT或导管损坏,以免出现并发症和延长住院时间。此外,可以假设,感染、敷料应用程序和因扭结而更换PT情况的减少具有设施和成本效益。
利益冲突声明
作者声明无利益冲突。
资助
作者未因该项研究收到任何资助。
Author(s)
Sivagame Maniya*
RN MN IIWCC WOCN DNP
Advanced Practice Nurse
SengKang General Hospital, Singapore
Email sivagame.maniya@skh.com.sg
Ma V Gonzalves
RN
Nurse Clinician
SengKang General Hospital, Singapore
Nurashiqin B Saadan
RN
Senior Staff Nurse
SengKang General Hospital, Singapore
* Corresponding author
References
- Wallace MJ, Chin KW, Fletcher TB, Bakal CW, Cardella JF, et al. Quality improvement guidelines for percutaneous drainage/aspiration of abscess and fluid collections. J Vasc Intervent Radiol 2010;21:431–435.
- Dagli M, Ramchandani P. Percutaneous nephrostomy: technical aspects and indications. Semin Intervent Radiol 2011;28(4):424–437. doi:10.1055/s-0031-1296085.
- Huang SY, Engstrom BI, Lungren MP, Kim CY. Management of dysfunctional catheters and tubes inserted by interventional radiology. Semin Intervent Radiol 2015;32(2):67–77. doi:10.1055/s-0035-1549371.
- Lorenz J, Thomas JL. Complications of percutaneous drainage. Semin Intervent Radiol 2006;23(2):194–204. doi:10.1055/s-2006-941450.
- Elamin EWM, Taha SM, Ahmed MEIM, Mansour MO, Mustafa G, Gismalla MDA, Elhassan MMA. Outcome and complications of percutaneous nephrostomy: single center experience. Sudan Med J 2017;53(2):69–75.
- Robert B, Yzet T, Regimbeau JM. Radiologic drainage of post-operative collections and abscesses. J Visc Surg 2013;S11–S18. doi:10.1016/j.jviscsurg.2013.05.005
- Sdrales L, Benumof JL. Prevention of kinking of a percutaneous transtracheal intravenous catheter. Anesthesiol 1995;82:288–291.
- Turo R, Horsu S, Broome J, Das S, Gulur DM. Complications of percutaneous nephrostomy in a district general hospital. Turk J Urol 2018;44(6):478–483.
- Martin R, Baker H. Nursing care and management of patients with a nephrostomy. Nurs Times 2019;115(11):40–43.
- Urology Nursing Working Group. Management of patients with nephrostomy tubes: clinical guideline and patient information templates. Chatswood, Australia: Agency for Clinical Innovation; 2013 [cited 2022 Dec 16]. Available from: http://www.aci.health.nsw.gov.au/_data/assets/pdf_file/0005/191066/ACI_Nephrostomy_Jan13.pdf
- Skrabec Jr QR. Using the Ishikawa process classification diagram for improved process control. Qual Eng 2007;3(4):517–528. doi:10.1080/08982119108918880
- Rowan NJ, Kremer T, McDonnell G. A review of Spaulding’s classification system for effective cleaning, disinfection and sterilization of reusable medical devices: viewed through a modern-day lens that will inform and enable future sustainability. Sci Total Environ 2023;878:162976. doi:10.1016/j.scitotenv.2023.162976.
- Molina H, Chan MM, Lewandowski RJ, Gab A, Riaz A. Complications of percutaneous biliary procedures. Semin Intervent Radiol 2021;38(3):364–372. doi:10.1055/s-0041-1731375


