Volume 29 Number 3
Demographic and injury details of chemical burn patients at a burn centre in the southeastern Anatolia region of Turkey
Ebral Yiğit and Ilhan Taş
Keywords mortality, chemical burns, epidemiology, morbidity
For referencing Yiğit E and Taş I. Demographic and injury details of chemical burn patients at a burn centre in the southeastern Anatolia region of Turkey. Wound Practice and Research 2021; 29(3):154-157
DOI
https://doi.org/10.33235/wpr.29.3. 154-157
Submitted 9 June 2021
Accepted 16 July 2021
Abstract
Introduction Chemical burns are the result of exposure to a variety of substances commonly found in the home, workplace and surrounding environment.
Material and method Between January 2016 and December 2019, patients who were followed up for chemical burns in the burn centre of Diyarbakır Gazi Yaşargil Training and Research Hospital were examined. In this study, we collected medical records, demographic information, cause of injury and related factors, hospital treatment and demographic data (e.g. age, sex, location, application date and discharge date).
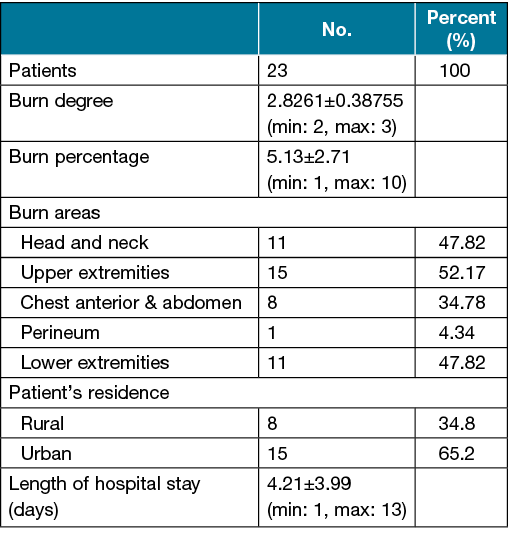
Results The number of patients hospitalised for chemical burns was 23, of which 18 (78.3%) were males and 5 (21.7%) were females. The most frequently affected body areas were the upper extremities, and two patients had conjunctivitis in the eyes after chemical burns. Mean total body surface area 5.13±2.71 (min: 1, max: 10). Chemical burns occurred as work-related accidents in five patients. The remaining 18 chemical injuries were accidental and at home. Acid and base chemical burns were seen in equal numbers. Chemical burns were most common in spring and summer.
Conclusion Chemicals in the household should be stored in safe, well-ventilated areas and should be kept out of the reach of everyone.
Introduction
Chemical substances are commonly used as industrial products. There are over 5 million well-known chemical compounds and 300 of them were reported by the National Fire Protection Association as chemicals with a very high level of health hazard. At the present time more than 65000 different types of chemical substances are present on the market and approximately 6000 new types are added each year1.
Chemical burns are the result of exposure to a variety of substances commonly found in the home, workplace and surrounding environment. Chemical burns constitute approximately 10.7% of all burn injuries and 2–6% of all burn centre admissions2. Although they have a low occurrence rate, chemical burns constitute 30% of all burn-related deaths3. The epidemiological characteristics of chemical burn injuries vary between different countries; they also show internal differences within a particular country according to the geographical location, the level of development in various regions, and even the country’s military situation (e.g. at war or during peace)4. There are some study results on chemical burn injuries in Turkey; however, these studies are very limited1.
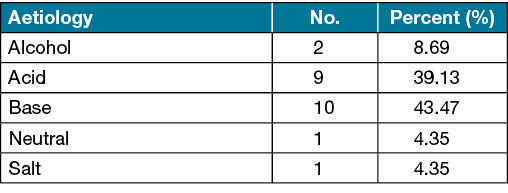
Chemicals can be classified as acid, alkali, organic and inorganic compounds. Acidic chemicals, other than hydrofluoric acid, cause coagulation necrosis, while bases create liquefaction necrosis and therefore often wider and deeper burns5. Organic and inorganic compounds cause tissue damage by directly binding and forming salts6.
Healthcare professionals should know the types and treatment modalities of chemical burns in order to recognise, manage and treat the burns7. In this study, we aimed to show the results of chemical burn treatment in our burn centre.
Materials and methods
Between January 2016 and December 2020, patients who were followed up for chemical burns in the burn centre of Diyarbakır Gazi Yaşargil Training and Research Hospital were examined. All patients included in the study were hospitalised. The burn centre in Diyarbakır is the only one in southeast Turkey. It serves the 10 million citizens of Diyarbakır and the surrounding 300 kilometres. Since we are the only centre with an intensive care unit in southeast Turkey, we serve all patients with major burn trauma and complicated burns.
This study was carried out in accordance with the principles of the 2008 Declaration of Helsinki, and a retrospective review was conducted through the electronic medical record system with permission from the chief physician. From the hospital’s electronic medical record system, we collected medical records, demographic information, cause of injury and related factors, hospital treatment and demographic data (e.g. age, sex, location, application date and discharge date). From the same system, we also collected information on injury-related data (e.g. burn status, cause of burn injuries, total body surface area [TBSA] and degree of burn), major complications and treatment outcomes (e.g. recovery, discontinuation or death).
Statistical analysis
Numerical data obtained in the study were expressed as arithmetic mean ± standard deviation, and categorical data were expressed as frequency (percentage). Statistical analyses were performed using the SPSS 16.0 (Chicago, IL, USA) statistical package program. Compliance of numerical data with a normal distribution was tested with Chi-square tests, independent Student’s t-tests, one-way analysis of variance (one-way ANOVA), and Tukey’s honestly significant difference (HSD) post hoc tests were used for statistical analysis. A p<0.05 value was accepted for statistical significance.
Results
The number of patients hospitalised for chemical burns was 23, of which 18 (78.3%) were males and 5 (21.7%) were females. Our male:female ratio was 3.6. The mean age of the patients was 24.7±20.78 years. The age groups most affected by chemical burns were five (21.73%) patients in the 1–4 year age group, six (26.08%) in the 15–24 year age group and seven (30.43%) in the 45–64 year age group.
Seven patients presented to our centre 1 day after the burn, while the remaining 16 patients presented to our emergency department on the day of the chemical burn. The most frequently affected body areas were the upper extremities, and two patients had conjunctivitis in the eyes after chemical burns (Table 1).
Table 1. Demographic and injury details of chemical burn patients
Chemical burns developed as a result of work-related accidents in five patients. The remaining 18 chemical injuries were accidental and at home (Table 2). The most common cause of chemical burns was sodium hydroxide (NaOH) with 17.39%. Acid and base chemical burns were seen in equal numbers (Table 3).
Table 2. Occurrence mode of chemical accidents
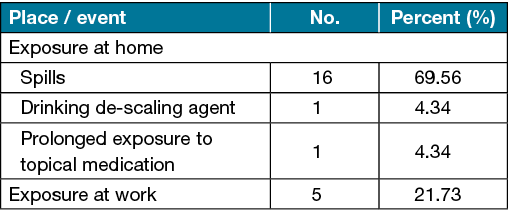
Table 3. Causes of chemical burns
The most common cause of chemical burns in women was creams, lotions (such as garlic or cologne) or medical materials used for traditional complementary medicine (Figure 1). In men, burns were from household cleaning materials (e.g. bleach, sodium hypochlorite [NaClO], lime remover and amidosulfonic acid) and from drain cleaners (NaOH) at work (Figure 2). Chemical burns started to increase in the spring and peaked in the summer. The burns made a second peak in the autumn. There were no cases in January or February (Figure 3).

Figure 1. Chemical burn after long-term use of medical silicone
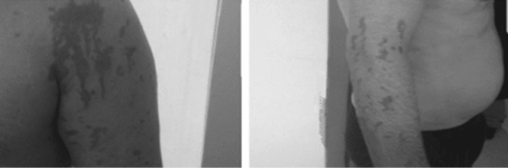
Figure 2. Patient injured due to drain cleaner
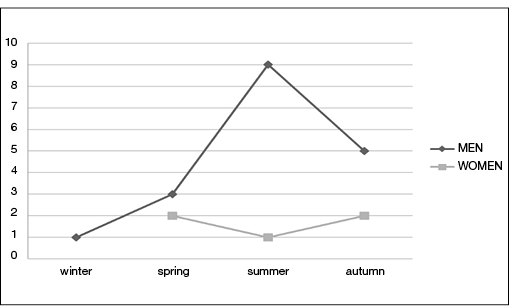
Figure 3. Number of patients presenting with burns to our unit according to season
Escharectomy was performed in 21 (91.30%) patients and these patients recovered with dressings. A fasciocutaneous flap was applied to two (7.70%) patients after the burn excision. The mean hospital stay was 4.21±3.99 days. None of our patients had an amputation or died during treatment.
Discussion
Early intervention is important in the treatment of chemical burns8. In our study, seven (30.43%) patients could not receive emergency first aid treatment because they were admitted to the hospital with a delay of at least 1 day. The other 16 (69.56%) patients were able to receive emergency first aid treatment.
Li et al.9 reported a mean TBSA of 30.3±24.7 in chemical burn patients. However, the patients in our study had a much lower mean TBSA of 5.13±2.71. We attribute our low TBSA rate to the fact that most of the chemical burns developed as a result of exposure to household cleaning materials rather than from workplace accidents.
Xie et al.10 reported that males were predominant among patients with chemical burn injuries. Our study is comparable with the literature in this respect. In our region, home renovation work (opening sinks with NaOH) is generally done by men. We attribute these accidental household burns to the fact that, once used, chemical cleaning materials may not have been safely stored by the person who cleaned the house.
According to the study by Gao et al.11, acids are the most common cause of chemical burns; however, in our study, acid and base chemical burns occurred in equal numbers. Gao et al.11 also reported that chemical burns occur mostly in summer and autumn, with the incidence gradually increasing in April and peaking in July, at which point it gradually begins to decrease. Our study results are in parallel with this, as chemical burns peaked in the spring and autumn. Culturally, we attribute this to the spring cleaning made in preparation for the spring season in the region and the autumn cleaning done in the preparation for winter.
In the epidemiological study by Song et al.12, the rate of burns resulting from work accidents in the last 5 years was 33.4%; however, in the last 7 years, there had also been an 11.6% decrease in burns resulting from work accidents. In our study, the rate of chemical burns resulting from an occupational accident was 21.73%. We attribute our low rate to the scarcity of factories producing chemicals since we are an underdeveloped country.
According to Zhang et al.13, chemical burns that develop as a result of work accidents usually occur when carrying chemicals by hand or because the worker did not wear the necessary protective clothing. Similarly, in our study, injuries were mostly seen in the upper extremities since adequate protective equipment was not used while cleaning or renovating the house.
The most common cause of chemical burns in our study was exposure to chemicals used in household cleaning. Houses with large families are often unhealthy/unsafe. Therefore, the consumption of cleaning materials, such as NaClO and NaOH, which are easily available in local markets and supermarkets, is high. The traditional use of such chemicals can easily lead to serious consequences. Our results are consistent with the studies of Saraçoğlu et al1.
The gold standard treatment in chemical burn injuries is to remove the substance that caused the chemical burn and to wash the wound with copious amounts of water8. In this regard, public awareness should be raised in order to prevent complications of possible chemical burn injuries.
Conclusion
In our region, chemical burns mostly occur accidentally at home. Healthcare professionals should be knowledgeable about the types and treatments of accidental chemical burns in homes.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
Not applicable.
Funding
The authors received no funding for this study.
Author(s)
Ebral Yiğit*1 MD
Email ebralyigit@gmail.com
Ilhan Taş1
1Gazi Yaşargil Training and Research Hospital Department of General Surgery, Diyarbakır
Turkey 21090
* Corresponding author
References
- Saraçoğlu A, Yılmaz M, Saraçoğlu KT. Chemical burn injuries. Kocaeli Med J 2018;7(1):54–58.
- Ahmadi H, Durrant CAT, Sarraf KM, et al. Chemical burns: a review. Curr Anaesth Crit Care 2008;19:282–286.
- Maghsoudi H, Gabraely N. Epidemiology and outcome of 121 cases of chemical burn in East Azarbaijan province, Iran. Injury 2008;39(9):1042–6.
- Pitkanen J, Al-Qattan MM. Epidemiology of domestic chemical burns in Saudi Arabia. Burns 2001;27(4):376–8.
- Hettiaratchy S, Dziewulski P. ABC of burns: pathophysiology and types of burns. BMJ 2004 Jun 12;328(7453):1427–9. doi:10.1136/bmj.328.7453.1427. Erratum in: BMJ 2004 Jul 17;329(7458):148. PMID:15191982; PMCID: PMC421790.
- Koltka K. Burn injuries: burn depth, physiopathology and type of burns. J Turkish Soc Intensive Care 2011;9 Special issue:1–6.
- Rochlin DH, Rajasingh CM, Karanas YL, Davis DJ. Full-thickness chemical burn from trifluoroacetic acid: a case report and review of the literature. Ann Plast Surg 2018 Nov;81(5):528–530. doi:10.1097/SAP.0000000000001579. PMID:30059387.
- Palao R, Monge I, Ruiz M, Barret JP. Chemical burns: pathophysiology and treatment. Burns 2010 May;36(3):295–304. doi:10.1016/j.burns.2009.07.009. Epub 2009 Oct 28. PMID:19864073.
- Li W, Wu X, Gao C. Ten-year epidemiological study of chemical burns in Jinshan, Shanghai, PR China. Burns 2013 Nov;39(7):1468–73. doi:10.1016/j.burns.2013.03.012. Epub 2013 Apr 24. PMID:23622871.
- Xie Y, Tan Y, Tang S. Epidemiology of 377 patients with chemical burns in Guangdong province. Burns 2004 Sep;30(6):569–72. doi:10.1016/j.burns.2004.01.028. PMID:15302423.
- Gao H, Li W, Zhao YD. Epidemiological investigation of 615 patients with chemical burns in eastern China. Zhonghua Shao Shang Za Zhi 2012 Dec;28(6):411–4. Chinese. PMID:23327908.
- Song C, Chua A. Epidemiology of burn injuries in Singapore from 1997 to 2003. Burns 2005 Jan;31 Suppl 1:S18–26. doi:10.1016/j.burns.2004.10.005. PMID:15649612.
- Zhang YH, Han CM, Chen GX, Ye CJ, Jiang RM, Liu LP, Ni LF. Factors associated with chemical burns in Zhejiang province, China: an epidemiological study. BMC Public Health 2011 Sep 30;11:746. doi:10.1186/1471-2458-11-746. PMID:21958110; PMCID: PMC3196712.



