Volume 29 Number 3
A survey of nurses’ wound assessment knowledge, attitude and competence in Nigeria
Helen N Obilor, Adeboye B Omolara and Odinaka B Ani
Keywords attitude, clinical competence, knowledge, nurses, wound assessment
For referencing Obilor HN et al. A survey of nurses’ wound assessment knowledge, attitude and competence in Nigeria. Wound Practice and Research 2021; 29(3):140-147.
DOI
https://doi.org/10.33235/wpr.29.3.140-147
Submitted 29 June 2021
Accepted 29 July 2021
Abstract
Background Wound assessment is an integral component of wound management that improves patient wound healing outcomes.
Aim This study aimed to assess nurses’ knowledge, attitude and competence in wound assessment in Nigeria.
Methods This descriptive, cross-sectional study utilised a structured questionnaire based on relevant literature and wound assessment guidelines for data collection.
Results A total of 182 registered nurses participated in the study. Nearly 75% of the participants had diploma nursing education but had not attended any post-nursing training wound care program. More than half of the nurses demonstrated a high level of knowledge (n=96, 52.7%) in wound assessment overall, except in wound aetiology, wound size measurement, undermining and wound bed tissues. Also, 51.1% of the nurses had a positive attitude (n=93) and low competence (n=171, 94%) in wound assessment. Wound assessment was mostly perceived as physicians’ responsibility and not that of nurses. There was no significant association between nurses’ competence and knowledge (χ2=0.24, p=0.81) and their attitude to wound assessment (χ2=0.15, p=0.73).
Conclusion Many of the nurses lacked competence in wound assessment and demonstrated a deficiency in their knowledge and attitude, thus suggesting the need for in-service education of nurses on wound assessment procedures and regular updates of nurses’ knowledge, skill and competence in Nigeria.
Key points
- Wound assessment is a quality improvement standard required to effectively manage patients with wounds. However, nurses who are primarily responsible for routine wound care often do not conduct detailed wound assessments.
- This study evaluated nurses’ knowledge, attitude and competence in wound assessment using a structured questionnaire in order to identify gaps and improve nurses’ wound care practice.
- Overall, the nurses demonstrated a high knowledge and positive attitude to wound assessment but demonstrated low competency in wound assessment tasks, thus suggesting the need to train nurses in clinical settings on wound assessment.
Introduction
Wound care is one of the primary and routine duties of nurses that focuses on restoring structural and functional skin integrity. Required for quality wound care is a comprehensive or detailed wound assessment. A wound assessment is a standard practice involving a serial examination and documentation of all aspects of a wound and its impact on the patient’s wellbeing. It is a valid and reliable method of monitoring healing progress and identifying factors that may delay the wound’s healing1. Wound assessment facilitates the development and implementation of an individualised wound care plan.
The benefits of holistic wound assessment include optimum wound healing, improved patient quality of life, and decreased treatment costs for both patients and the organisation2. Clinicians involved in wound care need to conduct detailed wound assessments for all patients irrespective of the wound type, aetiologies or practice setting because of its significance3. However, this has remained a professional challenge, especially for nurses4. Research evidence shows that nurses often do not conduct detailed wound assessments due to insufficient knowledge and poor attitude5,6. A similar practice gap in nurses’ wound assessment in Nigeria was reported by Oseni and Adejumo7 and, as observed by the authors, has remained unchanged.
Globally, wounds are prevalent health problems that constitute a significant healthcare burden. There is therefore an urgent need to understand nurses’ ability to perform wound assessment because of the increasing cases of chronic wounds8. This rising prevalence of chronic wounds is due to the growth in the aged population and chronic conditions such as diabetes and obesity. In addition, Nigeria has a high rate of road traffic accidents, making traumatic wounds a leading acute wound condition managed in healthcare facilities9,10. Wound assessment facilitates accurate diagnosis, appropriate treatment decisions, and strategies to avoid complications11. In addition, the cost of wound care is extremely high, and wound assessment can help ensure that nursing interventions are cost-effective and evidence-based. Furthermore, the rapid development in wound care science has led to an increased availability of various advanced dressings and technologies, which therefore makes professional decision-making on treatment options very challenging12. The right choice of dressing(s) and treatment modality among the available wound care options is skillfully rooted in detailed assessment findings.
The ability to conduct a comprehensive wound assessment depends on professional competencies, operationalised as the interplay of knowledge, performance, skills, judgement and attitude required for efficient wound assessment practice13. A key determinant in competence development is the extent to which nurses interpret, integrate and apply knowledge in practice14. Wound assessment requires that nurses have a sound knowledge of the physiology of the skin and wound healing process and the ability to identify potential impediments to healing, discriminate between subjective and objective data, and analyse and interpret findings from the assessment15. Primarily, wound assessment is rooted in clinical observations16 and so requires a lot of clinical skill, experience, and a positive disposition.
Nurses’ inability to perform detailed wound assessments can potentially result in treatment failure, exposure to professional litigation, and questions over professionalism15. Also, any negative nurse attitude to wound assessment can affect the delivery of quality wound care6. Furthermore, the inability of nurses to conduct detailed wound assessment could lead to delay in wound healing, patient discomfort, increased risk of infection, inappropriate use of wound dressings, increased wound care cost, and a reduction in patients’ quality of life17–20. In contrast, an accurate wound assessment correlates with positive client health outcomes11.
Nurses’ competence in wound assessment is therefore critical for effective wound management. Nurses’ competence in wound assessment facilitates their ability to establish current wound conditions accurately, evaluate whether the wound is improving or deteriorating, and decide upon the most suitable treatment20. Given the significance of wound assessment in wound care, it is pertinent that nurses take the responsibility to routinely evaluate and improve their competencies19. As part of the effort to improve the quality of nursing wound care in Nigerian, this study aimed to assess nurses’ knowledge, attitude and competence in wound assessment.
Method
This study utilised a descriptive cross-sectional design to investigate nurses’ knowledge, attitude and competence in wound assessment. The participants were registered nurses who rendered wound care to clients in a tertiary healthcare facility in southwest Nigeria. A total of 182 nurses working in the hospital’s medical, surgical and neuroscience units participated in the study. The hospital units were purposefully selected because these units were known to have the highest number of clients with wound care needs. The participants were recruited using a convenience sampling method. The sample size was determined based on two factors: Yamane’s formula n=N/[1+(N(e2)]21, where n is the sample size, N is the total number of nurses working in the selected hospital units (259 nurses) and e is the level of precision (0.05); and consideration of a 15% attrition rate.
The data collection instrument was a 50-item structured questionnaire based on relevant literature on wound assessment procedures11,14,22. The instrument has four sections – socio-demographic characteristics, knowledge, attitude and competence of nurses in wound assessment. The nurses’ competence section incorporated three wound pictures with features specific to tissue type, undermining and edge in order for the study participants to assess and document their findings. The scoring scales used in the competence section for nurses to document their assessment findings were adapted from the Photographic Wound Assessment tool (wound bed tissues)23 and Bates-Jensen Wound Assessment tool (wound edge and undermining)24. Experts in wound care at the study location ascertained the content validity of the instrument. The questionnaire has a test-retest (2-week interval) reliability coefficient of 0.81. The reliability of the instrument was determined using 20 nurses involved in the care of individuals with wounds in a secondary health facility in Southwest Nigeria.
The Ethical Review Board of the University of Ibadan/University College Hospital, Ibadan, approved the study protocol. The hard copies of the study questionnaire were administered in person following the approval of the hospital administrator. Nurses who consented to participate in the study were given the questionnaire to fill in at their convenience; these were retrieved after a week. Data collection lasted for 1 month.
The data were analysed using the Statistical Package for Social Sciences (SPSS) version 25. Both descriptive and inferential statistics were undertaken. A marking guide was developed and used to score the participants’ responses. For the knowledge section, each correct response was scored as ‘1’ while an incorrect response or ‘I don’t know’ was scored as ‘0’ (the expected score range was 0–25). Knowledge score was classified into low and high levels based on the obtained mean value, below and above the mean value, respectively. The items exploring participants’ attitudes were structured in a four-point Likert scale format (strongly agree, agree, disagree and strongly disagree), with the expected score ranging from 10–40. The participants’ attitude to wound assessment was classified into negative attitude (score below the obtained mean value) and positive attitude (score from the obtained mean value and above). Each correct assessment was scored as ‘1’ in the competence section, while incorrect assessments/missing responses were scored as ‘0’ (the expected score range was 0–5). The obtained score was classified as low (0–3) and high competence4,5.
Results
Socio-demographic variables
Table 1 shows the socio-demographic characteristics of the study participants. Most of the participants were female (n=166, 91.2%). The average years of nursing practice was 6.5 (±4.5). Most nurses had a diploma in nursing as the highest level of education (n=140, 76.9%). In addition, 72.3% of the participants had never attended a wound care training workshop or seminar throughout their professional nursing practice.
Table 1. Participants’ socio-demographic characteristics
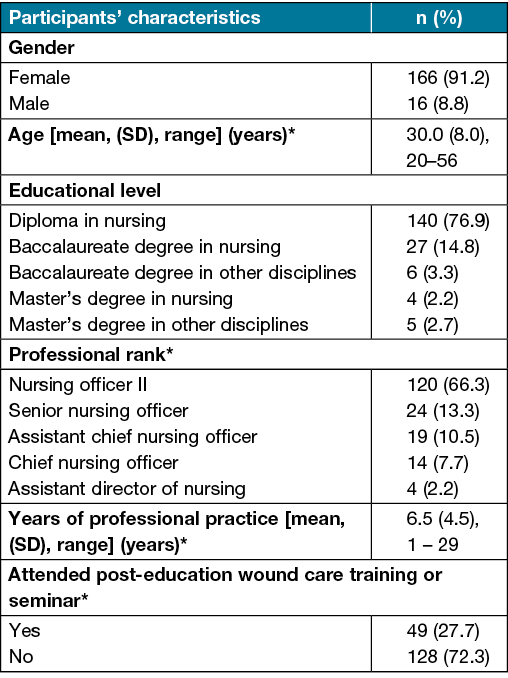
* represents items with missing responses
Knowledge of wound assessment
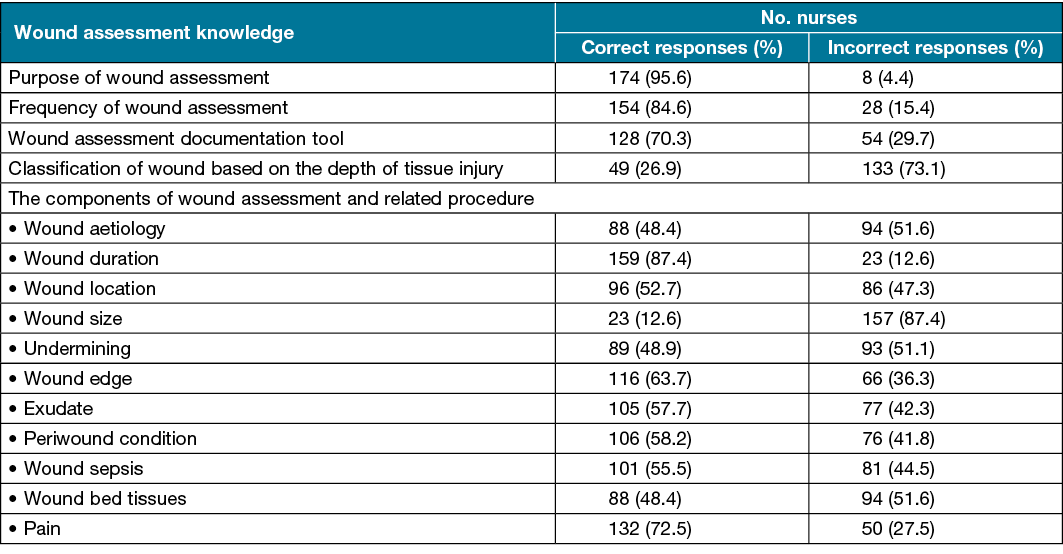
The participants’ wound assessment knowledge score ranged from 1–24, with a mean of 16.6 (±4.7). Most participants demonstrated high knowledge (n=96, 52.7%), while 47.3% (n=86) had low knowledge of wound assessment. More specifically, most of the participants were knowledgeable about the purpose of wound assessment and the frequency of wound assessment. However, less than half of the participants demonstrated knowledge of wound classification based on tissue injury depth (n=49, 26.9%). Regarding wound assessment components, the majority of the participants demonstrated sound knowledge except on the aspect of wound aetiology (n=88, 48.4%), the measurement of wound size (n=23, 12.6%), undermining (n=89, 48.9%), and wound bed tissues (n=88; 48.4) (Table 2).
Table 2. Participants’ wound assessment knowledge
Attitude to wound assessment
The participants’ attitude scores ranged from 10–40, with a mean value of 28.7 (±5.3). Based on the predetermined classification, 48.9% (n=89) had a negative attitude, while 51.1% (n=93) had a positive attitude to wound assessment. More specifically, more than half of the participants (n=98, 53.8%) agreed to the statement that wound assessment is the sole responsibility of the physicians and not that of nurses (Table 3).
Table 3. Participants’ attitude to wound assessment
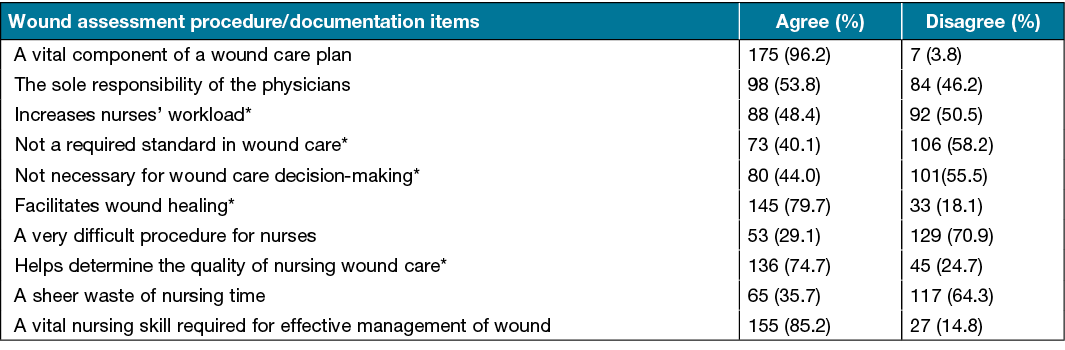
* represents items with missing responses
Wound assessment competence
The participants’ wound assessment competence mean score was 2.0±1.2 (range 0–5). Figure 2 shows that 65–93% of nurses incorrectly assessed the different wound features shown in the digital images on the study questionnaire, namely wound bed tissues, undermining and edge (Figure 1). Based on the predetermined classification, 11 (6%) nurses had high competence while the others had low competence (171, 94%). Finally, the Chi-square analysis revealed that the nurses’ competence in wound assessment was not significantly associated with their knowledge (χ2=0.24, df=2, p=0.81) and attitude (χ2=0.15, df=1, p=0.73).
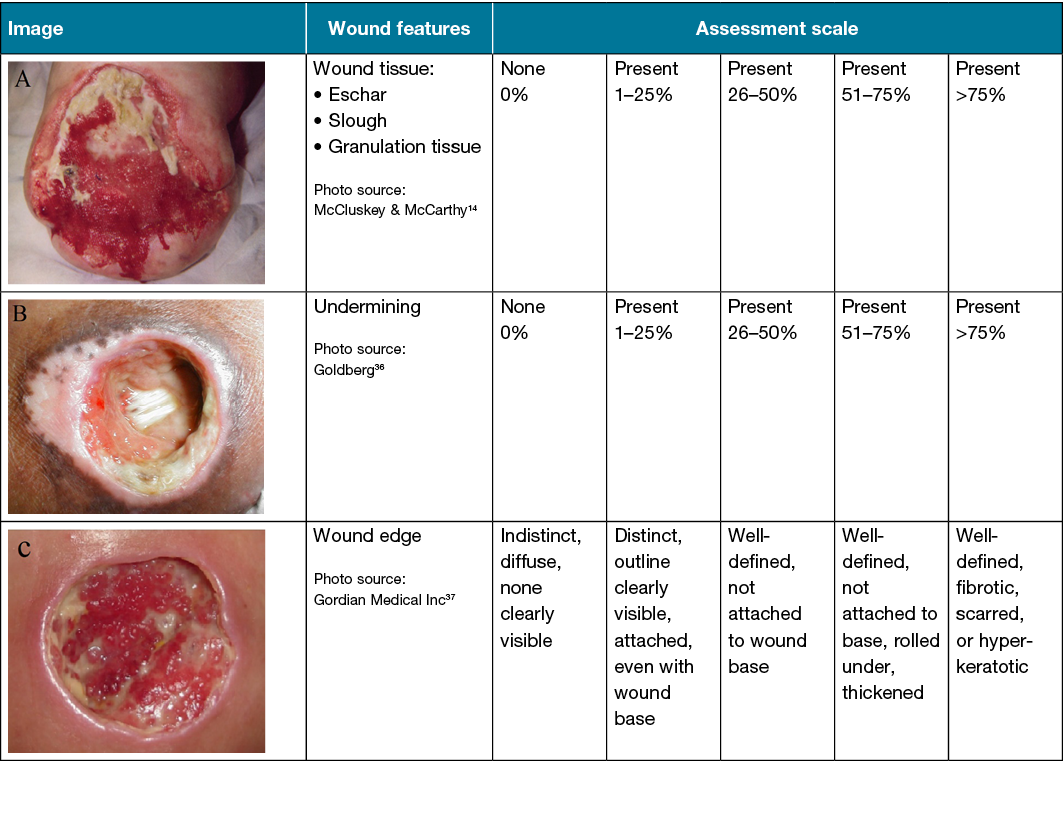 Figure 1. Wound assessment competence section of the study questionnaire
Figure 1. Wound assessment competence section of the study questionnaire
Assessment scale adapted from the Photographic Wound Assessment Tool (A) and Bates-Jensen Wound Assessment tool (B and C).
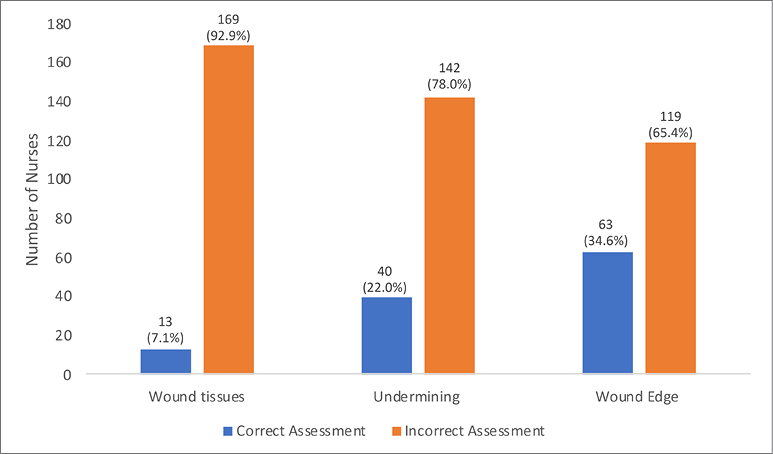
Figure 2. Nurses’ competence in wound assessment
Discussion
Optimum wound management is an essential skill and competence required by nurses to manage patient health effectively. Nurses play a crucial role during routine patient nursing care because they provide the critical observation that informs the decisions for wound treatments. However, wound assessment/management knowledge and competence among nurses in middle and low-income countries are poorly described. Nurses are expected to assess wounds at the beginning of treatment and periodically. The clients’ assessment must be detailed, comprehensive and extend beyond the wound to identify other factors such as biopsychosocial issues that impede wound healing and the clients’ compliance with treatment. This professional wound care skill requirement depends on individual nurses’ knowledge of wound characteristics and the healing process, their competence to carry out wound assessment, and their attitude or belief14. This study described nurses’ wound assessment knowledge, attitude and competence in wound assessment in a tertiary health facility in response to the Nursing and Midwifery Council of Nigeria action call to promote patient-centred care and quality improvement in Nigeria.
Knowledge is valuable for evidence-based practice as it underpins and gives power to nurses’ actions. A lack of knowledge can leave nurses powerless to provide quality patient care. In this study, the nurses demonstrated an overall high level of knowledge in wound assessment. The knowledge level observed among nurses in this study is similar to that reported in McCluskey and McCarthy14, and Ayello, Baranoski and Salati25, where a good knowledge level in wound care, including wound assessment, was found among the study participants. On the contrary, the observed overall knowledge level in this study was in disagreement with findings from the study of Faria et al.26 and Ilesanmi and Olabisi27 with a low level of knowledge in wound assessment and management.
This difference in study results on nurses’ knowledge may be linked to the broad nature of these studies as they did not primarily focus on wound assessment. In this study, even though most nurses had overall high knowledge in wound assessment, the nurses had limited knowledge in wound aetiology, measurement, undermining and wound bed tissues. Wound size determination (area and depth), aetiology, undermining and wound bed tissues are core components of wound assessment that guide treatment decisions. The wound measurement provides information on wound size that further serves as the baseline for ongoing treatment decisions and periodic evaluation of the impact of interventions28. The different wound bed tissues reflect the physiological responses that help provide objective data on the current wound healing status and aid clinicians in identifying appropriate treatment goals and dressing products11. Assessment of the wound’s edge and undermining can provide information on wound aetiology, severity, healing progress, and the effectiveness of the current treatment plan29. Therefore, insufficient nurse knowledge in core wound assessment components could translate to inappropriate treatment decisions, delays in wound healing, poor quality of life, and increased healthcare costs.
Healthcare professional attitude is an important quality that reflects individual belief and helps understand how issues or processes are perceived in clinical care and decision-making on what is appropriate for patients’ health and wellbeing30. Most nurses in this study had an overall positive attitude towards wound assessment. This finding is similar to that reported in Dilie and Mengistu31 where nurses were noted to have a positive attitude towards wound assessment and wound care in general. However, despite the positive attitude, over 50% of the participants in this study stated that wound assessment is the physicians’ sole responsibility and not that of nurses, with about 40% considering it not to be an essential standard in wound care and decision-making.
Nevertheless, this opinion is erroneous and detrimental to patients’ wellbeing. In the study setting, it is routine for nurses to expose patients’ wounds even when a dressing change is not due for physician assessment during medical rounds, which may suggest the basis for the reported nurse attitude. This exposure tends to increase patient suffering, risk of infection, and healthcare costs. Assessment is the first step of the nursing process covered extensively in nursing training and should be practised by nurses irrespective of the procedure or a patient’s condition32. Assessment informs subsequent components of a patient’s nursing care plan – diagnosis, planning, implementation and evaluation – and wound assessment should not be an exception. A positive change in nurses’ perception of wound assessment as their primary responsibility and a vital care standard could help ensure that they conduct detailed wound assessment and documentation both at admission and periodically throughout patient care. This, in turn, could help reduce the routine exposure of wounds during physicians’ rounds for evaluation purposes and increase patients’ health outcomes in Nigeria.
The last outcome assessed in this study was nurses’ competence in wound assessment. The regular evaluation of nurses’ competence in wound assessment could help identify real-life problems, knowledge and skill gaps in clinical performance, thus providing the evidence to prompt action to address the identified gap before patients’ health is negatively affected.
In this study, only 6% of the nurses demonstrated competency in wound bed tissues, undermining and edge assessment. The wound characteristics assessed provided information on aetiology, healing status, anticipated healing time and prognosis that could facilitate treatment decisions to promote optimum wound healing, prevent complications, and improve patients’ quality of life. The proportion of nurses competent in wound assessment observed in this study is lower than that reported in McCluskey and McCarthy14 where 37% of Irish nurses (n=145) correctly assessed the wound healing phase and identified if the wound was infected.
In addition, the high knowledge and positive attitude to wound assessment observed in this study did not correlate to the participants’ competence to assess the featured wound characteristics shown in the pictures. In practice, nurses must apply and adapt their knowledge, skills and innate individual traits that informs their attitude to each clinical situation33. The non-significant association between nurses’ wound assessment competence and their knowledge and attitude could result from the nurses’ limited knowledge in core assessment components discussed above and their perception of wound assessment as not being their responsibility.
The observed competency level in wound assessment in this study could also be attributed to Nigeria’s general nursing educational preparation and poor attendance of post-training programs as shown in the socio-demographic data. The preparatory training course in wound care for student nurses primarily focuses on dressing change procedures with little or no emphasis on objective wound assessment methods. Also, it is expected that nurses in their clinical practice build on their educational training through self-education, reflection and attending further training to improve their knowledge, skill and competence in providing holistic and evidence-based care. Other determinants of nurses’ competence in wound assessment need to be explored.
Overall, the finding of this study on nurses’ wound assessment competence suggests a severe deficiency in practice and a threat to patient safety in Nigeria that needs to be urgently addressed through the development of competency-based wound assessment and management programs.
Finally, the strength and limitations of this study need to be highlighted. The first strength of this study is the combination of variables – knowledge, attitude and competence – explored to identify nurses’ practice gaps and generate results that can improve nurses’ practice in clinical settings. In the literature, most studies focus primarily on knowledge and attitude regarding the practice of wound assessment. Studies that assess the nurses’ wound assessment competency, especially in low-income countries, are scarce. In addition to the in-depth knowledge and attitude of nurses uncovered, this study provides insight into their competence, a critical factor that drives professionalism and safe practice. Secondly, the indirect method (wound images) used to determine nurses’ competence in wound assessment helped prevent undue exposure of patients’ wounds and eliminated their risk of infection and discomfort. Wound photographs are an objective method to evaluate wound size, depth, tissue types, edge and peri-wound and obtain data to ascertain severity, deterioration, or improvement, in wound conditions23.
Despite the strengths mentioned above, this study is limited because it was conducted only among nurses working in some selected units of a tertiary hospital in Nigeria. Thus, it may be difficult to generalise the study findings to nurses working in various healthcare facilities in Nigeria. In addition, photographs are not an ideal method to assess undermining34. The undermining of wound edges is a severe complication that delays the wound healing cascade. The standard step of evaluating undermining involves carefully inserting a cotton-tipped probe under the wound edge parallel to the wound surface until the point of resistance and then measuring the depth in centimetres and documenting the location using the clock method35. The image used in this study, however, provided some insight into nurses’ competence in terms of identifying the location of undermining but not in quantifying the depth of tissue destruction and thus could have affected the participants’ interpretation. Also, the overall knowledge level obtained in this study could have been influenced by the data collection technique that allowed participants to complete the questionnaire within a week without being directly observed by the research team. Hence, there is a need to interpret the result with caution.
Conclusion
Nurses are at the forefront of wound care delivery and make very salient contributions to improving services rendered to patients. Adequate knowledge, attitude and competence towards wound assessment will positively impact nurses’ clinical practice in wound care and improve other healthcare team members’ trust in their judgment and documentation. However, the high knowledge and positive attitude to wound assessment found in this study did not increase nurses’ competence. In addition, most nurses lacked specific knowledge of the core components of wound assessment, perceived it as not their responsibility, and demonstrated low competence. This study finding implies the need for the hospital-based in-service education program to emphasise the importance of wound assessment and regularly update nurses’ knowledge and skill in wound assessment. Efforts, therefore, need to be consolidated at all levels of nursing administration towards ensuring that nurses are trained in wound assessment and resources such as wound assessment documentation tools are made available.
There is also a need to review the general nurses’ preparatory education curriculum and include comprehensive wound assessment. An in-service education program in wound assessment will help nurses in clinical practice be knowledgeable, perceive wound assessment as a nursing responsibility, and become competent. Thus, it could, in turn, lead to an improvement in patient health outcomes. Proficiency in wound assessment could also help nurses carry out evidence-based, patient-centred and cost-effective wound care. Future studies should design wound management education programs and evaluate their impact on both nurses’ practice and patient health outcomes.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
Not applicable.
Funding
The authors received no funding for this study.
Author(s)
Helen N Obilor* MSc (Nursing), RN PhD Candidate
Department of Nursing, Faculty of Clinical Sciences, College of Medicine, University of Ibadan, Ibadan, Nigeria
School of Nursing, Queen’s University, Kingston ON, Canada
Email ngoziobilor@yahoo.com
Adeboye B Omolara BNSc, RN
Northern Lincolnshire and Goole NHS Foundation Trust, UK
Odinaka B Ani MSc (Nursing), RN
Department of Nursing, Faculty of Basic Medical Sciences, Lead City University, Ibadan, Nigeria
* Corresponding author
References
- Nix D. Skin and wound inspection and assessment. In: Bryant RA, Nix DP, editors. Acute and chronic wounds: current management concepts. Missouri, USA: Elsevier; 2016.
- Wounds UK. Best practice statement: Improving holistic assessment of chronic wounds London: Wounds UK; 2018. Available from: https://www.wounds-uk.com/resources/details/best-practice-statement-improving-holistic-assessment-chronic-wounds.
- de Leon J, Bohn GA, DiDomenico L, Fearmonti R, Gottlieb HD, Lincoln K, et al. Wound care centers: critical thinking and treatment strategies for wounds. Wounds 2016;28(10):S1–s23.
- Gottrup F, Apelqvist J, Bjarnsholt T, Cooper R, Moore Z, Peters EJ, et al. EWMA document: Antimicrobials and non-healing wounds. Evidence, controversies and suggestions. J Wound Care 2013;22(5 Suppl):S1–89.
- Barrett S, Cassidy I, Graham MM. National survey of Irish community nurses leg ulcer management practices and knowledge. J Wound Care 2009;18(5):181–2, 4,6 passim.
- Fletcher J. Development of a new wound assessment form. Wounds UK 2010;6(1):92–9.
- Oseni OM, Adejumo PO. Nurses’ reported practice and knowledge of wound assessment, assessment tools and documentation in a selected hospital in Lagos, Nigeria. Afr J Med Med Sci 2014;43(2):149–57.
- Järbrink K, Ni G, Sönnergren H, Schmidtchen A, Pang C, Bajpai R, et al. Prevalence and incidence of chronic wounds and related complications: a protocol for a systematic review. System Rev 2016;5(1):152.
- Obilor HN, Adejumo PO. A review of the road traffic accident cases admitted in the University College Hospital, Ibadan. Af J Nurs Hlth Iss 2013;4 (1):33–8.
- Obilor HN, Adejumo PO, Ilesanmi RE. Assessment of patients’ wound-related pain experiences in University College Hospital, Ibadan, Nigeria. Int Wound J 2016;13(5):697–704.
- Benbow M. Best practice in wound assessment. Nurs Stand 2016;30(27):40–7.
- Shi C, Wang C, Liu H, Li Q, Li R, Zhang Y, et al. Selection of appropriate wound dressing for various wounds. Frontier Bioengineer Biotech 2020;8(182).
- Pijl-Zieber EM, Barton S, Konkin J, Awosoga O, Caine V. Competence and competency-based nursing education: finding our way through the issues. Nurse Ed Today 2014;34(5):676–8.
- McCluskey P, McCarthy D. Nurses knowledge and competence in wound management. Wounds UK 2012;8(2):37–47.
- Benbow M. Wound care: ensuring a holistic and collaborative assessment. Br J Comm Nurs 2011;16(Sup9):S6-S16.
- van Rijswijk L, Eisenberg M. Wound assessment and documentation. Chronic wound care: the essentials e-book. Malvern, PA: HMP Communications; 2018. p. 29–46.
- Dowsett C. Use of TIME to improve community nurses’ wound care knowledge and practice. Wounds UK 2009;5(3):14–21.
- Timmins J. Can nurses’ knowledge of wound care be improved by a systematic approach to wound management? Applied wound management. Wounds UK 2009(Part 3):14–7.
- Ousey K, Cook L. Understanding the importance of holistic wound assessment. Practice Nurs 2011;22(6):308–14.
- Greatrex-White S, Moxey H. Wound assessment tools and nurses’ needs: an evaluation study. Int Wound J 2015;12(3):293–301.
- Yamane T. Statistics: an introductory analysis. 2nd ed. New York: Harper and Row; 1967.
- Baranoski S, Ayello EA, Langemo D. Wound assessment. In: Baranoski S, Ayello EA, editors. Wound care essentials: practice principles. 4th ed. Philadelphia, PA: Wolters Kluwer 2016. p. 206–44.
- Thompson N, Gordey L, Bowles H, Parslow N, Houghton P. Reliability and validity of the revised photographic wound assessment tool on digital images taken of various types of chronic wounds. Adv Skin Wound Care 2013;26(8):360–73.
- Bates-Jensen B. Bates-Jensen Wound Assessment Tool 2001. Available from: https://www.wwwoundcare.ca/Uploads/ContentDocuments/BWAT.pdf.
- Ayello EA, Baranoski S, Salati DS. A survey of nurses’ wound care knowledge. Adv Skin Wound Care 2005;18(5 Pt 1):268–75; quiz 76–8.
- Faria GBG, Prado TN, Lima EFA, Rogenski NMB, Borghardt AT, Massaroni L. Knowledge and practice of nurses on the care of wounds. J Nursing UFPE/Revista de Enfermagem UFPE 2016;10(12):4532–8.
- Ilesanmi RE, Olabisi P. Assessment of common interventions and perceived barriers to pressure ulcer prevention in southwest Nigeria. J WOCN 2014;41(3):242–6.
- Dowsett C, Protz K, Drouard M, Harding KG. Triangle of wound assessment made easy. Wounds Int 2015:1–6.
- Leaper DJ, Schultz G, Carville K, Fletcher J, Swanson T, Drake R. Extending the TIME concept: what have we learned in the past 10 years?. Int Wound J 2012;9 Suppl 2:1–19.
- Price B. Understanding attitudes and their effects on nursing practice. Nursing Stand 2015;30(15):50–7; quiz 60.
- Dilie A, Mengistu D. Assessment of nurses’ knowledge, attitude, and perceived barriers to expressed pressure ulcer prevention practice in Addis Ababa government hospitals, Addis Ababa, Ethiopia, 2015. Adv Nurs 2015;2015:796927.
- Toney-Butler TJ, Unison-Pace WJ. Nursing admission assessment and examination. StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
- Fukada M. Nursing competency: definition, structure and development. Yonago Acta Med 2018;61(1):1–7.
- Houghton PE, Kincaid CB, Campbell KE, Woodbury MG, Keast DH. Photographic assessment of the appearance of chronic pressure and leg ulcers. Ostomy Wound Manage 2000;46(4):20–6, 8–30.
- Brennan MR. Wound assessment: a step-by-step process. Nursing 2019;49(8):62–4.
- Goldberg C. Clinical images section of MedPics. UCSD School of Medicine and VA Medical Center, San Diego, CA. Available from: https://medpics.ucsd.edu/index.cfm?curpage=image&course=clinImg&mode=browse&lesson=118&img=2131
- Gordian Medical Inc. dba American Medical Technologies. Available from: http://leadingagene.org/wp-content/uploads/2018/11/Handout-Nebraska-Regional-Wound-Seminar_Part-II.pdf



