Volume 31 Number 2
Acute care nurses’ experience in providing evidence-based care for patients with laparotomy wounds: a scoping review protocol
Sarah Hulbert-Lemmel, Auxillia Madhuvu, Victoria Team
Keywords nursing, acute care, evidence-based care, experience, laparotomy wounds
For referencing Hulbert-Lemmel S, Madhuvu A & Team V. Acute care nurses’ experience in providing evidence-based care for patients with laparotomy wounds: a scoping review protocol. Wound Practice and Research 2023; 31(2):74-81.
DOI
https://doi.org/10.33235/wpr.31.2.74-81
Submitted 12 December 2023
Accepted 22 March 2023
Abstract
Background Healthcare organisations provide policies and guidelines to direct the nursing staff’s decision-making surrounding care in patients with surgical wounds to reflect the best current evidence. Nonetheless, nurses face multiple challenges in providing evidence-based care (EBC), leading to inconsistent surgical wound care. In addition, the reduction of the use of laparotomy procedures in elective practice has led to a potential decrease in competence and experience in its treatment regime, particularly related to wound management.
Study objective This is a protocol for a scoping review that will systematically search and synthesise available data on barriers and enablers to EBC for patients with laparotomy wounds reported by nurses in acute care settings. We will focus on the reported barriers and enablers related to wound assessment, wound products, dressing application, infection control techniques, documentation, holistic care and escalation of care.
Methods and analysis The Preferred Reporting Items for Systematic review and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist and explanation documents will guide the review protocol. The methodology framework formulated by Arksey and O’Malley1, revised by Levac et al2 and the Joanna Briggs Institute (JBI)3, will be utilised to structure the scoping review. Qualitative themes will be aligned with the Theoretical Domains Framework (TDF)4.
Introduction
A laparotomy is an invasive exploratory and emergency surgery often performed for gynaecological, pelvic and abdominal conditions5. It is also known as a coeliotomy or celiotomy procedure, and involves a large midline incision into the abdomen to expose the peritoneal cavity6. A laparotomy procedure can be utilised for investigating abdominal and pelvic symptoms and for diagnostic and curative purposes5,6. A laparotomy procedure is useful in traumatic injuries that require immediate stabilisation and visualisation of the abdominal cavity7.
Large incisional wounds, such as laparotomy wounds, are not as prevalent as laparoscopic approaches yet require skill and expertise to manage postoperatively5,8. Laparotomy procedures have decreased in use, favouring diagnostic abdominal and gynaecological laparoscopic approaches, better known as keyhole surgery, since the 1990s in developed countries9,10. The decrease is primarily due to the heightened risk of complications associated with open abdominal surgical approaches, high mortality risk, surgeon preference and experience, and extended length of stay for recovery5,11,12.
Laparotomy procedures are still performed in acute life-threatening presentations, and 23,115 emergency laparotomy procedures were performed in the state of Victoria, Australia, between 2007–20167. Furthermore, the Australia and New Zealand Audit of Surgical Mortality (ANZASM) report indicates inconsistent recovery outcomes, postoperative complications, and a 18.1% mortality rate for patients 80 years and over after emergency laparotomy procedures7,13. Similarly, in the United Kingdom, laparotomy procedures are associated with a high patient mortality rate and extensive financial, emotional and physical costs associated with postoperative recovery12. In addition, the limited rationale for the laparotomy approach in elective practice has led to a potential reduction in expertise in managing large abdominal surgical wounds.
Current best practice recommendations for surgical abdominal wounds involve a holistic approach to treatment planning similar to any wound cared for by clinicians. Firstly, an assessment of the patient, including a comprehensive medical history and assessment of vital signs, nutritional status, presence of pain, and overall physical health, is required to ascertain the care needs of the patient and screening for influencing factors in wound healing14–17. A vital component of wound practice is assessment, which requires the identification of the wound and documentation of the phase of wound healing, such as inflammation, reconstruction or proliferation, and maturation or remodelling phase18. Wounds are characterised by their type classification, such as acute and chronic, and healing classification, such as a surgical incision healing either by primary or secondary intention14. Physical wound details, such as its location, aetiology, wound duration, measurements of dimension, depth, peri-wound and wound edge status, appearance, condition of the wound bed and output, such as exudate or haemoserous volume, are routinely documented14. Clinicians may utilise classifications for surgical wounds by the Centers for Disease Control and Prevention (CDC), which are allocated by class I–IV and terms such as clean, clean-contaminated, contaminated and dirty-infected19-21. The National Institute for Health and Care Excellence (NICE) has made alternative recommendations to guide clinicians in surgical wound management. These guidelines highlight modification of care through surgical wound phases such as preoperative, intraoperative and postoperative22.
Using and integrating validated clinical tools enables nurses to ensure they practise evidence-based care (EBC). For example, local-level policies will stipulate documentation of assessment findings and wound care in health organisations’ wound charts and risk assessments to provide consistent care and standards for wound treatment. Clinicians are also suggested, through research evidence findings, to follow guidelines formed by the International Wound Bed Preparation Advisory Board such as the ‘TIME’ tool, which is a pneumonic for tissue, infection, moisture and edge23. The TIME acronym can form the principles of assessment and wound bed preparation as a supportive tool in clinical decision-making and management for clinicians caring for clinical wounds23,24. Nursing staff are advised to use their critical thinking in selecting the appropriate resources, with current product references and the wound practice techniques to use, such as clean, aseptic, non-touch or sterile approaches, based on their assessment findings25. Utilising the best available evidence, referring to local policies and procedures, and applying clinical judgement will assist staff in selecting the appropriate care for their patients’ wound management.
Currently, no Australian guidelines which are strictly related and isolated to laparotomy wound care for acute care nurses have been identified in the available literature. Australian guidelines direct clinicians to broadly adopt practices for acute, postoperative wound care, focusing on the wound type not the surgical procedure. The use of generalised surgical wound recommendations targeting the multidisciplinary team are also available in the United Kingdom and the United States26–28. Acute care nurses are encouraged to utilise these resources to guide their practice surrounding surgical wounds such as a laparotomy wounds.
Australian nurses work within the standards and scope of practice outlined by the Nursing and Midwifery Board of Australia (NMBA)29. A nurses’ scope underpins their clinical decisions and actions to be supported by the best available evidence29. Concerning wound care management, nurses can refer to the Wounds Australia Standards for wound prevention and management document30. Nevertheless, nurses’ adoption of EBC over practice-based experience remains varied and limited, even though nurses are familiar with and believe in EBC’s value for providing patient-centred care31–34. In addition, nurses’ theoretical underpinnings of EBC do not necessarily translate into conducting EBC habitually35,36.
The relationship between EBC gaps in nursing, especially in wound care, is well established in the literature. For example, previous studies have identified clinicians’ gaps in current knowledge and procedures, lack of education, access to resources and dressings, managerial support for utilising EBC, and environmental and psychological barriers in applying EBC to nurses caring for wounds37–42. The investigation into the nursing role in surgical site infections is also thoroughly researched, establishing how to manage impediments in preventing hospital-acquired infections21,43,44. The role of the acute nurse in wound care requires further investigation, especially concerning the reduction in laparotomy procedures, and significant postoperative complications and mortality rate. Nonetheless, acute care nurses’ perspectives on barriers and enablers to providing EBC for patients with laparotomy wounds remains an area requiring further attention.
Study rationale
Previous studies have explored the broad predictors of nurses’ EBC wound management activities and investigated the various factors influencing their wound-based care. This scoping review aims to explore barriers and enablers to providing EBC for patients with laparotomy wounds reported by acute care nurses.
Study objectives
The objectives of the proposed review are to systematically search and synthesise available data on acute care nurses’ reports of barriers and enablers to providing EBC for patients with laparotomy wounds. In particular, we will focus on the reported barriers and enablers related to wound assessment, wound products used, dressing application, infection control techniques, documentation, holistic care and escalation of care.
Protocol development
The scoping review will be completed utilising the Preferred Reporting Items for Systematic review and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist. The methodology framework developed by Arksey and O’Malley1, revised by Levac et al2 and the Joanna Briggs Institute (JBI)3, will frame the protocol with six stages.
Stage 1: Identifying the research question
The study will aim to identify themes to examine EBC among acute care nurses managing laparotomy wounds. The following research question was established based on the current evidence surrounding nursing wound care.
Research question
- What are barriers and enablers to providing evidence-based care (EBC) for patients with laparotomy wounds reported by acute care nurses?
The proposed scoping review aims to identify the information gap from the findings of the proposed research question.
Stage 2: Identifying relevant studies
Systematic and scoping reviews and published protocols were searched in the Campbell Collaboration, Cochrane collaboration and the International Prospective Register of Systematic Reviews (PROSPERO) registries. The search identified no similar review published.
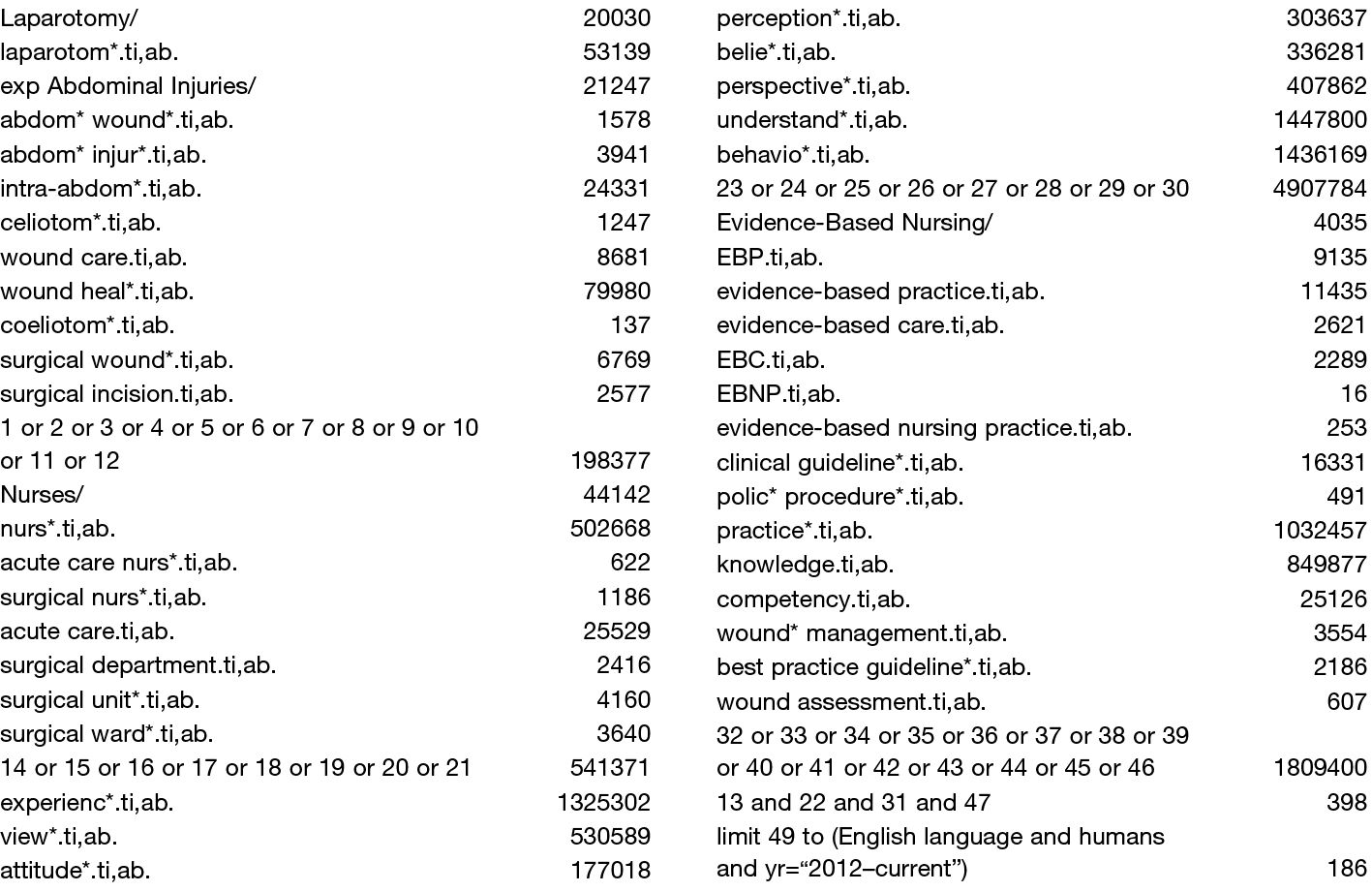
The research strategy was developed with the guidance of the research team and a librarian. The academic databases Ovid Medline, CINAHL and Embase will be searched to select appropriate research journals. The search approach and terms were drafted with the liaison librarians’ assistance and subsequently modified by the research team. Appendix A includes an example of the last search performed on Ovid Medline on 27 September 2022. Google Scholar, PubMed and Connected Papers will be utilised to scan for relevant grey literature articles.
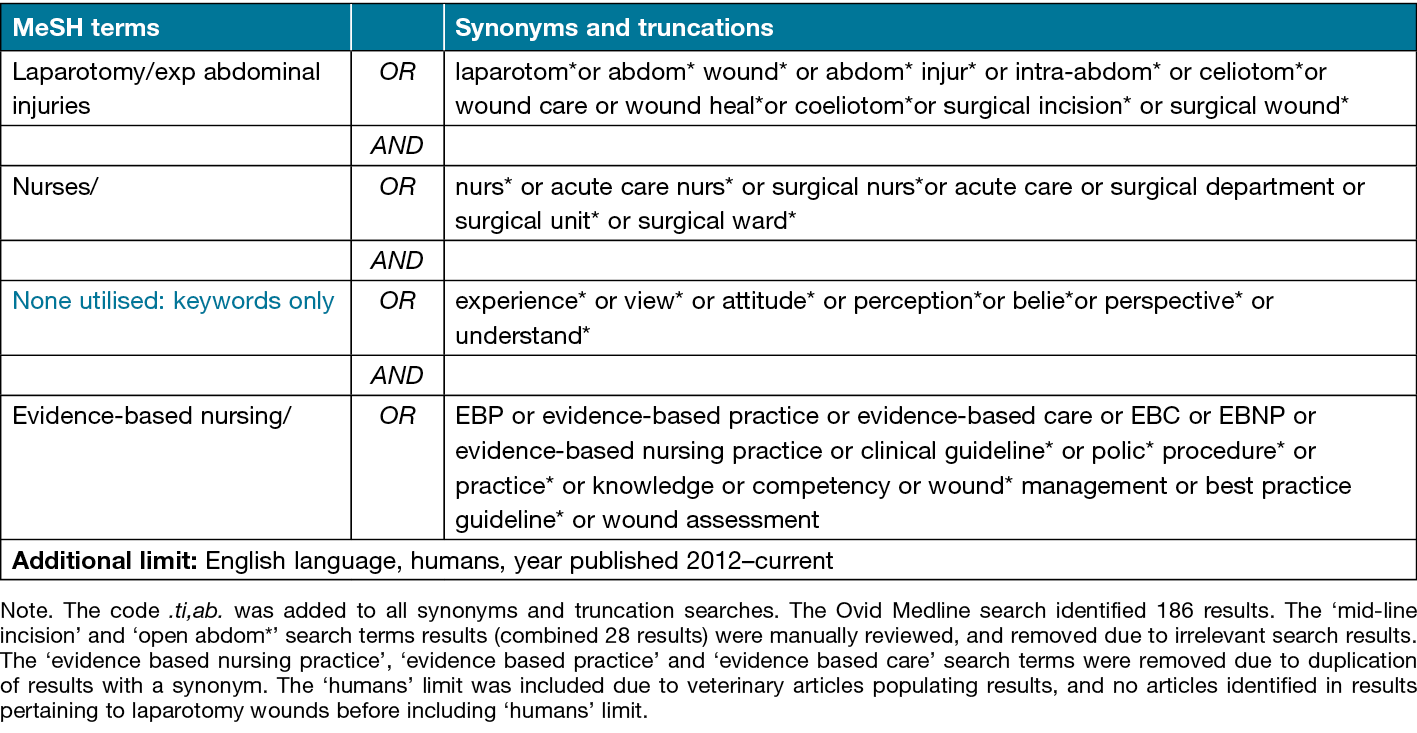
The preliminary search on Ovid Medline utilised keywords such as ‘wound care’, ‘nurse’, ‘experience’ and ‘evidence-based practice’ with truncations, synonyms and the use of MeSH terms to broaden the search results on the area of interest. Additional limits were chosen to restrict results to journal articles published within 2012–current, in English, and in human subjects to identify relevant and current evidence-based research were shown. Table 1 summarises the Ovid Medline search.
Table 1. Ovid Medline search strategy
The database results will be manually reviewed for journal articles based on the research inquiry and inclusion criteria. The search will be supplemented with manually searching key journals and hand-searching reference lists of the ‘gold set’ (key articles that can identify search terms and test the final search strategy). Co-citation and bibliographic coupling shall be identified through Connected Papers to highlight relevant articles to the inclusion criteria after a manual review.
Stage 3: Study selection
The main components to guide the research inquiry and develop the research questions were formulated using the population, interest and context (PiCo) method.
• Population: acute care nursing staff.
• Interest: studies exploring experiences, attitudes, views, perceptions, beliefs, perspectives and understanding of EBC in laparotomy wounds.
• Context: acute wards, departments and units.
Study types
Quantitative, qualitative and mixed-methods research study designs. Quantitative studies include non-experimental studies such as observation, retrospective chart audits and cross-sectional surveys. Qualitative studies included grounded theory, phenomenology, qualitative descriptive, case studies, observation, focus groups, individual interviews, and descriptive open-ended surveys.
Inclusion: EBC, evidence-based practice, experiences in abdominal surgical wound care, acute ward nurses (enrolled, endorsed and registered), and laparotomy wounds.
Exclusion: Abstract-only articles, articles published before 2012, in a non-English language, surgical wounds not located on the abdomen, studies focusing on student nurses, critical care nurses, rehabilitation nurses, post anaesthetic care unit (PACU)/recovery nurses, theatre nurses and community nurses.
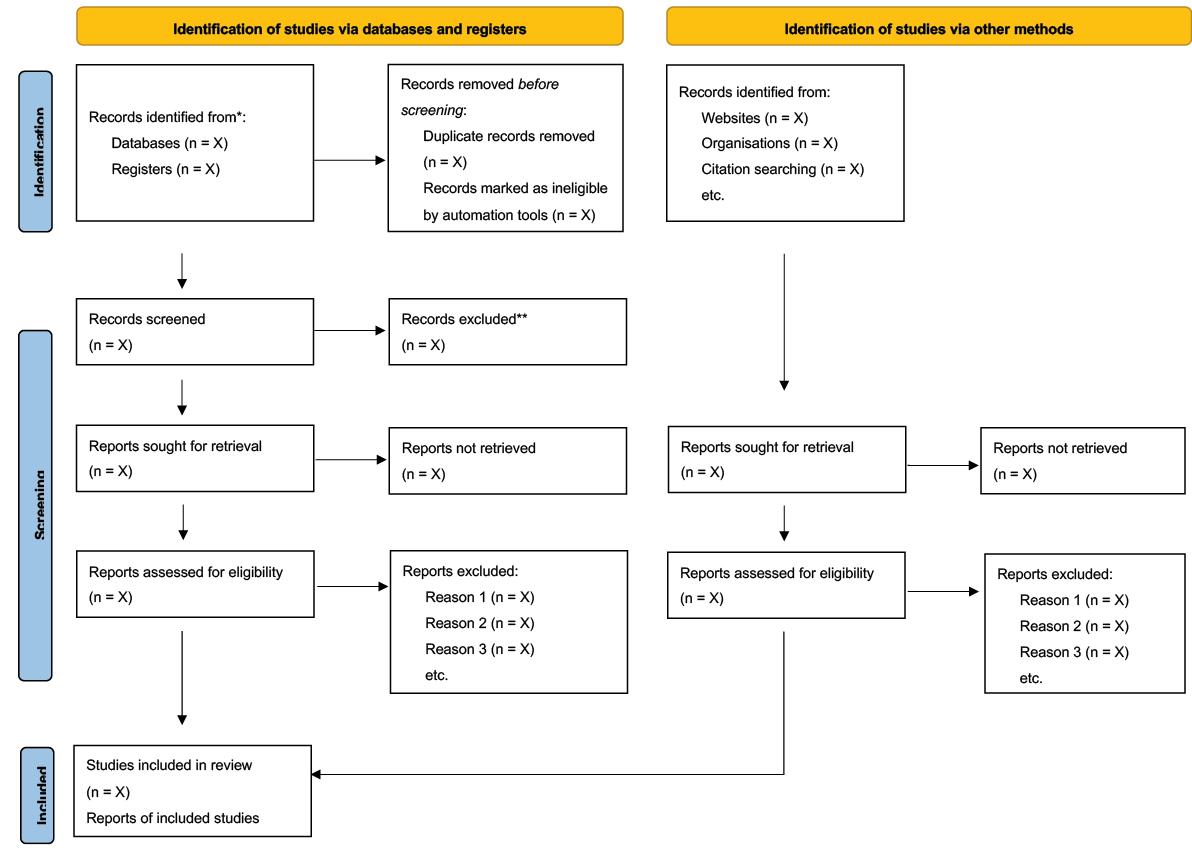
The PRISMA 2020 flow diagram for new systematic reviews, which includes searches of databases, registers and other sources, will be used to present the retrieved studies, reviewed articles, and excluded and included articles45. Appendix B displays an example of the flow diagram that will be populated with the search findings.
Stage 4: Charting the data
Two independent reviewers will screen all articles identified in the data searches; if a disagreement occurs, a third reviewer will be asked for their opinion. The EndNote 20.5 program will be used to import articles, results and reference management. Duplicate articles will be identified and removed in EndNote.
The results extraction will be populated Covidence®. We will conduct staged screening with two independent reviewers by reviewing the title and abstract of extracted results. Eligible results will have the full text assessed utilising the inclusion and exclusion criteria. The extracted results will follow the guide from the JBI Reviewers Manual 2015, Methodology for JBI Scoping Reviews46. Below are the key information points that will be documented from the search results when charting the data.
- Author(s)
- Year of publication
- Country of origin
- Aims/purpose
- Study population and sample size (if appropriate)
- Methodology/methods
- Outcome measures/results
- Funding sources
- Key findings that relate to the scoping review questions
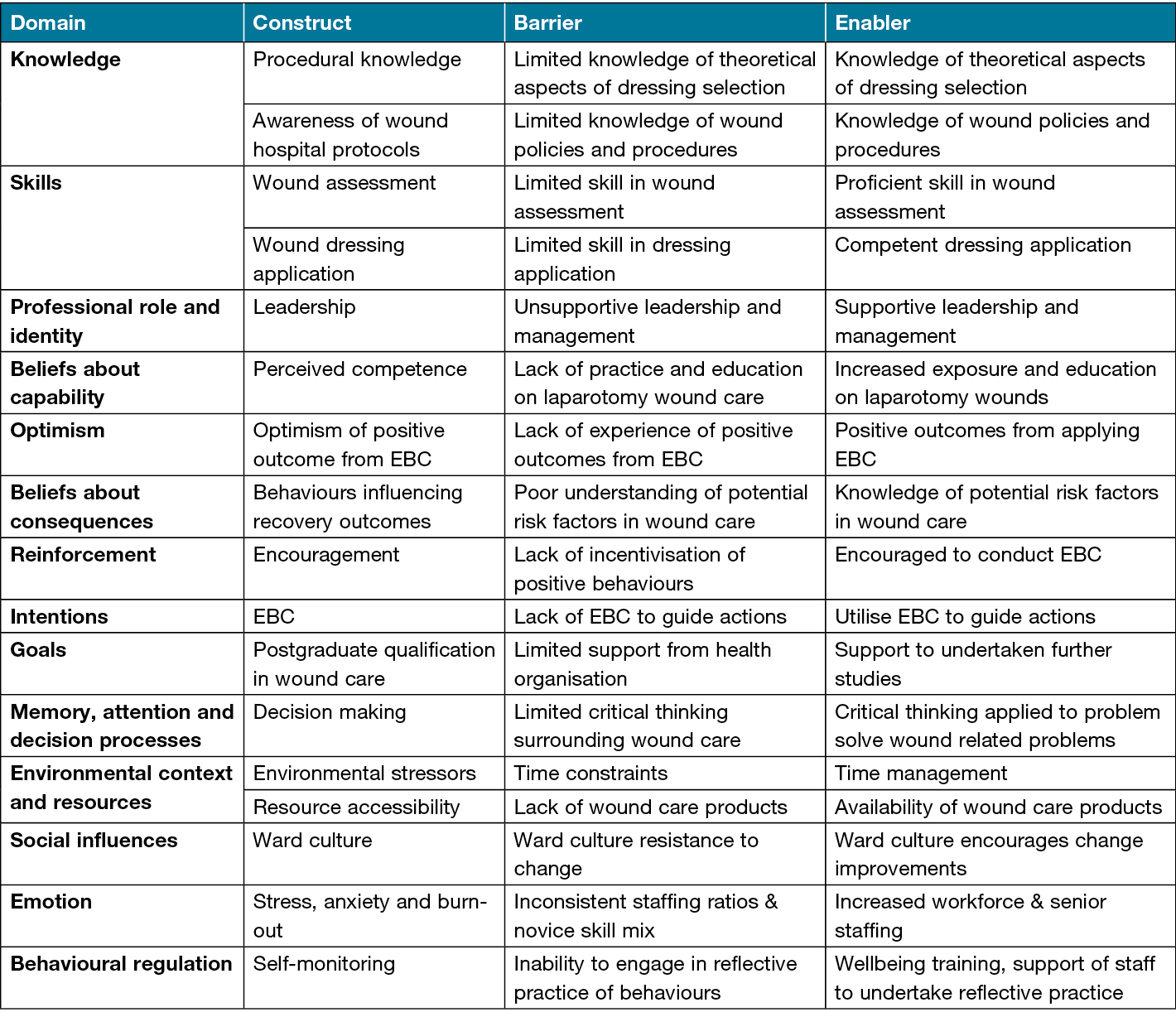
A Theoretical Domains Framework (TDF) will be applied in addition to the key points stated to ensure data extraction focuses on EBC barriers and enablers of acute care nurse4. The study introduced the TDF to understand nurse behaviours and create tailored intervention strategies to comprehensively and systematically identify barriers and enablers in EBC47. The TDF consists of 14 domains encompassing individual, environmental and resources, and social factors4,47. The TDF can identify wide contributing factors and influences of nurses’ behaviour in the acute care context, discovering new enablers, barriers and experiences in EBC47,48; Table 2 lists barriers and enablers examples for potential behaviours. The TDF is an ideal method to assist the formulation of successful change in EBC with nurses through identifying components, linking characterised behaviours, and developing effective interventions and policies to change those determinants49.
Table 2. Examples of potential barriers and enablers
Stage 5: Collating, summarising and reporting the results
Articles yielded in the search findings will be assessed and analysed for reliability and credibility. The Critical Appraisal Skills Programmes (CASP) checklist will be utilised for quantitative articles to ascertain their suitability. Each research type will be aligned with the appropriate CASP tool for appraisal and evaluation which will judge the selection of relevant articles for the review50. The Standards for Reporting Qualitative Research (SRQR) and the Consolidated Criteria for Reporting Qualitative Research (COREQ) will be applied to evaluate qualitative journals. The SRQR is a framework formulated to be applied to all forms of qualitative studies to analyse the reporting of key elements51. The SRQR does not review comprehensively all methodological aspects of studies; consequently, it cannot be used to ascertain quality and rigor of research methods and findings51. The COREQ, however, specialising in critiquing interviews and focus group studies, includes assessing the method and rigor of research findings52. The Mixed Methods Appraisal Tool (MMAT) will be utilised to appraise mixed method articles53.
Data charting will be conducted on the selected articles and displayed in formats appropriate for the type of research created to show the distribution of the studies. Qualitative articles that reflect trustworthiness and credible research will be analysed and matched with the TDF. Each reported enabler and barrier will be aligned with a relevant TDF domain and construct47. Incorporating all study types into the review ensures a broad overview of the best available evidence concerning the research inquiry.
Stage 6: Consultations – patient and public involvement
The scoping review is the first step in rationalising and conducting research into the barriers and enablers in the experiences of acute care nurses’ EBC in laparotomy wounds. There will be no direct involvement of the patients or nurses in this scoping review. Nevertheless, the findings of this review can be utilised by healthcare professionals to inform their practice and gain insight into current experiences in laparotomy care. Furthermore, the first author is a clinical nurse educator in the surgical field and has a full membership with Wounds Australia, providing a platform for future dissemination of the findings through educational formats, such as a webinar or an educational session within a healthcare facility. In addition, healthcare organisations, nurse associations, education providers, patients and clinicians can access the scoping review findings in the online peer-reviewed journal publication.
Discussion
Ethics and dissemination
The scoping review will collect data from databases and programs that are publicly available via open access or Monash University subscription. Ethics approval will not be required as no ethical considerations were identified for this scoping review. The findings of this scoping review will be communicated through the published peer-reviewed journal and virtual formats through professional social networks. Study findings will be presented at national and international forums.
Limitations
The scoping review protocol did not include all nurses’ perspectives on laparotomy wound care. The insights of non-ward based nurses can benefit understanding EBC if barriers and enablers are consistent or differ from ward nurses.
Potential articles excluded may pertain to nurses’ experiences in wound care post-laparotomy due to the publications’ country of origin and age. Furthermore, articles on traumatic abdominal and pelvic injuries that required a laparotomy procedure may have been omitted from the search findings due to potential terminology surrounding traumatic injuries.
Conclusions
The protocol provides a plan for a scoping review of barriers and enablers to providing EBC for patients with laparotomy wounds reported by acute care nurses. Based on the study findings, relevant conclusions will be developed to ascertain further research on acute care nurses’ experiences in providing EBC for patients with laparotomy wounds.
Author contribution
SHL and VT conceptualised the main ideas for this scoping review. SHL worked with AM and VT to develop the search strategy. All authors contributed to the framework for this protocol. SHL produced the drafts with support from AM and VT. AM and VT provided feedback, and reviewed and approved the final manuscript.
Acknowledgements
A special thank you to Mario Sos, liaison librarian in medicine, nursing and health sciences, and pharmacy and pharmaceutical sciences at Monash University, for his assistance in developing the search strategies.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
An ethics statement is not applicable.
Funding
The authors received no funding for preparing this study protocol.
Author(s)
Sarah Hulbert-Lemmel, Auxillia Madhuvu, Victoria Team*
Monash Nursing and Midwifery, Monash University
Clayton Campus, 35 Rainforest Walk, Clayton, VIC 3800, Australia
*Corresponding author email victoria.team@monash.edu
References
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method 2007;8(1):19–32
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5(69):1–9.
- Joanna Briggs Institute (JBI). JBI manual for evidence – the scoping review framework; 2020. Available from: https://jbi-global-wiki.refined.site/space/MANUAL/4687752
- Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N. Foy R, Duncan EM, Colquhoun H, Grimshaw JM, Lawton R, Michie S. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017;12(77):1–18.
- Galaal K, Donkers H, Bryant A, Lopes A. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database System Rev 2018;10(10):1–44.
- Rajaretnam N, Okoye E, Burns B. Laparotomy. StatPearls publishing; 2022. Available from: www.ncbi.nlm.nih.gov/books/NBK525961/
- Stevens CL, Brown C, Watters D. Measuring outcomes of clinical care: Victorian emergency laparotomy audit using quality investigator. World J Surg 2018;42(7):1981–1987.
- Wang J, Cheng L, Liu J, Zhang B, Wang W, Zhu W, Guo Y, Bao C, Hu Y, Qi S, Wang K, Zhao S. Laparoscopy vs. laparotomy for the management of abdominal trauma: a systematic review and meta-analysis. Frontier Surg 2022;9:1–13.
- Kelley WE Jr. The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. J Soc Lapa Robo Surg 2008;12(4):351–357.
- Koo YJ, Kim JE, Kim YH, Hahn H, Lee IH, Kim T, Lee K, Shim JU, Lim KT. Comparison of laparoscopy and laparotomy for the management of early-stage ovarian cancer: surgical and oncological outcomes. J Gyn Onco 2014;25(2):111–117.
- Broughton KJ, Aldridge O, Pradhan S, Aitken RJ. The Perth emergency laparotomy audit. ANZ J Surg 2017;87(11):893–897.
- Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ. Variations in mortality after emergency laparotomy: the first report of the UK emergency laparotomy network. Brit J Anae 2012;109(3):368–375.
- Royal Australasian College of Surgeons (RACS). Australian and New Zealand audit of surgical mortality national report 2016. RACS; 2016. p. 1–82. Available from: https://www.surgeons.org/-/media/Project/RACS/surgeons-org/files/surgical-mortality-audits/anzasm-reports/2017-10-05_rpt_racs_anzasm_national_report_2016.pdf?rev=84d67d943ed14d05a502f9509 adbbf3b&hash=B44712AAF2D2D0DE36985EE6F6846C8F
- Carville K. Wound care manual. Silver Chain Nursing Association; 2017.
- Ousey K, Cool L. Wound assessment: made easy. Wounds UK 2012;8(2):1–4.
- Weller CD, Team V, Sussman G. First-Line interactive wound dressing update: a comprehensive review of the evidence. Frontier Pharm 2020;11(155):1–13.
- Wilson M. Understanding the basics of wound assessment. Wounds Essen 2012;2:8–12.
- Yao K, Bae L, Ping-Yew W. Post-operative wound management. Aust Fam Physi 2013;42(12):867–870.
- Herman T, Bordoni B. Wound classification. StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554456/#_NBK554456_pubdet_
- Onyekwelu I, Yakkanti R, Protzer L, Pinkston CM, Tucker C, Seligson D. Surgical wound classification and surgical site infections in the orthopaedic patient. J Ame Aca Ortho Surg 2017;1(3):1–10.
- Adi MM, Sandy-Hodgetts S, Belooshi AA, Habib SA, Nuiami SA, Aziz H, Khazbak A, Tariq G, Tayeb M. Incision care and dressing selection in surgical incision wounds: findings from an international meeting of surgeons from the Middle East. Wounds Int 2022. Available from: https://www.woundsinternational.com/resources/details/incision-care-and-dressing-selection-surgical-incision-wounds-findings-international-meeting-surgeons-middle-east
- National Institute for Health and Care Excellence (NICE). Surgical site infections: prevention and treatment (NG125); 2019. Available from: https://www.nice.org.uk/guidance/ng125/ resources/surgical-site-infections-prevention-and-treatment-pdf-66141660564421
- Halim A, Khoo T, Saad A. Wound bed preparation from a clinical perspective. Ind J Plast Surg 2012;45(2):193–202.
- Moore Z, Dowsett C, Smith G, Atkins L, Bain M, Lahmann NA, Schultz GS, Swanson T, Vowden P, Weir D, Zmuda A, Jaimes H. TIME CDST: an updated tool to address the current challenges in wound care. J Wound Care 2019;28(3):154–161.
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service (NSQHS) Standards: preventing and controlling infections standard; 2021. Available from: https://www.safetyandquality.gov.au/sites/default/files/2021-07/nsqhs_standards_preventing_and_controlling_infections_fact_sheet_june_2021.pdf
- Huddart S, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA, Quiney N, Hemmings V, Riga A, Belguamkar A, Zuleika M, White D, Corrigan L, Howes T, Richards S, Dalton S, Cook T, Kryztopik R, Cornwell A, Goddard J, Grifiths S, Frost F, Pigott A, Pittman J, Cossey L, Smart N, Danials I. Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Brit J Surg 2015;102(1):57–66.
- Milne J, Vowden P, Fumarola S, Leaper D. Postoperative incision management made easy. Wounds UK Sup 2012;8(4):131.
- Peden CJ, Aggarwal G, Aitken RJ, Anderson ID, Foss BN, Cooper Z, Dhesi JK, French WB, Grant MC, Hammarqvist F, Hare SP, Havens JM, Holena DN, Hübner M, Kim JS, Lees NP, Ljungqvist O, Lobo DN, Mohseni S, Ordoñez CA, Quiney N, Richard D. Urman RD, Wick E, Wu CL, Young-Fadok F, Scott M. Guidelines for perioperative care for emergency laparotomy enhanced recovery after surgery (ERAS) society recommendations: part 1 – preoperative: diagnosis, rapid assessment and optimization. World J Surg 2021;45(5):1272–1290.
- Nursing and Midwifery Board of Australia (NMBA). Registered nurse standards for practice; 2016. Available from: https://www.nursingmidwiferyboard.gov.au/documents/default.aspx?record= WD16%2f19524&dbid=AP&chksum=R5Pkrn8yVpb9bJvtpTRe8w%3d%3
- Wounds Australia. Standards for wound prevention and management. Cambridge Media, 2016.
- Halberg N, Assafi L, Nørholm V. Understandings of and experiences with evidence-based practice among nurses in a surgical department: a constructivist approach. J Clin Nurs 2021;30(3–4):488–498.
- Karlsson A, Lindeborg P, Gunningberg L, Jangland E. Evidence-based nursing – how is it understood by bedside nurses? A phenomenographic study in surgical settings. J Nurs Mana 2019;27(6):1216–1223.
- Thorsteinsson HS, Sveinsdóttir H. Readiness for and predictors of evidence-based practice of acute-care nurses: a cross-sectional postal survey. Scandinavian J Car Sci 2014;28(3):572–581.
- Wallin L, Boström AM, Gustavsson JP. Capability beliefs regarding evidence-based practice are associated with application of EBP and research use: validation of a new measure. Worldviews Evid Nurs 2012;9(3):139–148.
- Alqahtani N, Kyeung M, Kitsantas P, Rodan M. Nurses’ evidence-based practice knowledge, attitudes and implementation: a cross-sectional study. J Clin Nurs 2019;29(1–2):274–283.
- Halberg N, Assafi L, Nørholm V. Understandings of and experiences with evidence-based practice among nurses in a surgical department: a constructivist approach. J Clin Nurs 2021;30(3–4): 488–498.
- Dung P, Trang L, Tung H. Nurses’ knowledge, practice, and confidence after the training program on wound care at the agriculture general hospital in Vietnam. Open J Nurs 2020;10:646–656.
- Flanagan M. Barriers to the implementation of best practice in wound care. Wounds UK 2005;1(3):74–82.
- Gartlan J, Smith A, Clennett S, Walshe D, Tomlinson-Smith A, Boas L, Robinson A. An audit of the adequacy of acute wound care documentation of surgical inpatients. J Clin Nurs 2010;19(15–16):2207–2214.
- Oseni OM, Adejumo PO. Nurses’ reported practice and knowledge of wound assessment, assessment tools and documentation in a selected hospital in Lagos, Nigeria. Afr J Med Med Sci 2014;43(2):149–157.
- Sonoiki T, Young J, Alexis O. Challenges faced by nurses in complying with aseptic non-touch technique principles during wound care: a review. Br J Nurs 2020;29(5):28–35.
- Welsh L. Wound care evidence, knowledge and education amongst nurses: a semi-systematic literature review. Intern Wound J 2018;15(1):53–61.
- Lin F, Gillespie BM, Chaboyer W, Li Y, Whitelock K, Morley N, Morrissey S, O’Callaghan F, Marshall AP. Preventing surgical site infections: facilitators and barriers to nurses’ adherence to clinical practice guidelines – a qualitative study. J Clin Nurs 2019;28(9–10):1643–1652.
- Mohsen M, Riad N, Badawy A. Compliance and barriers facing nurses with surgical site infection prevention guidelines. Open J Nurs 2020;10(1):15–33.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff K, Akl E, Brennan S, Chou R, Glanville J, Grimshaw J, Hróbjartsson A, Lalu M, Li T, Loder E, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The P.R.I.S.M.A. 2020 statement: an updated guideline for reporting systematic reviews. Brit Med J 2021;372(71):1–9.
- Peters M, Godfrey C, Mcinerney P, Soares C, Khalil H, Parker D. Joanna Briggs Institute reviewers’ manual. JBI; 2015. p. 1–24. Available from: https://nursing.lsuhsc.edu/jbi/docs/reviewersmanuals/scoping-.pdf
- Richardson M, Khouja CL, Sutcliffe K, Thomas J. Using the theoretical domains framework and the behavioural change wheel in an overarching synthesis of systematic reviews. BMJ Open 2019;9e024950:1–16.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7(37):1–17.
- Mather M, Pettigrew LM, Navaratnam S. Barriers and facilitators to clinical behaviour change by primary care practitioners: a theory-informed systematic review of reviews using the theoretical domains framework and behaviour change wheel. Systematic Rev 2022;11(180):1–20.
- Critical Appraisal Skills Programme (CASP). CASP checklist; 2022. Available from: https://casp-uk.net/how-to-use-checklist/
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med: J Asso Amer Med Col 2014;89(9):1245–1251.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. J Intern Soc Qua Health Care 2007;19(6):349–357.
- Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon MP, Griffiths F, Nicolau B, O’Cathain A, Rousseau MC, Vedel I. Mixed methods appraisal tool (MMAT) version 2018. McGill University. Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf
Appendix A. Ovid Medline search strategy
Appendix B. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers and other sources