Volume 31 Number 2
Iatrogenic hypospadias: a penile mucosal pressure injury
Anne-Maree Schweitzer, Tania Parr, Chia Hsin Tony Hsiung, Robert Smith, Eva Bruce, Patricia Hawke
Keywords iatrogenic hypospadias, urethral catheter injury, penile mucosal pressure injury, penile pressure injury
For referencing Schweitzer AM et al. Iatrogenic hypospadias: a penile mucosal pressure injury. Wound Practice and Research 2023; 31(2):87-89.
DOI
https://doi.org/10.33235/wpr.31.2.87-89
Submitted 10 May 2023
Accepted 23 May 2023
Abstract
Iatrogenic hypospadias is a common cause of iatrogenic complications in the elderly male patient with a long-term urethral catheter (IDC) device; however, there is limited research to support its prevalence. This complication is not widely recognised or documented, and the risk is not discussed with the family or patient prior to IDC insertion. There is also minimal research and evidence on the prevention of iatrongenic hypospadias, therefore further research will benefit the nursing care of these patients.
Introduction
International consensus on the staging of pressure injuries has been in place for many decades. However, it was only in 2016 that the US National Pressure Ulcer Advisory Panel (NPUAP) updated its definition of mucosal pressure injuries and noted that they could not be staged using the same classification system as skin due to the different histological characteristics of mucosal tissue1. Mucosal pressure injuries are essentially caused by pressure from medical devices.
While there is a significant amount of literature on pressure injury recognition, prevention and treatment research, there is limited research on medical device pressure-related injuries (MDPRIs), and even less on medical devices specifically causing mucosal injury. MDPRIs have been repeatedly recognised as “underreported and underestimated”1–9, despite having a high prevalence and incidence. Within the body of research that has been undertaken, it is well recognised that the very young and the elderly are the most susceptible to MDPRIs1,3,4,8,10,11. Additionally, those who are sedated or confused are recognised at higher risk4.
By far the majority of research into MDPRIs and specifically mucosal pressure injuries has been undertaken in the acute inpatient situation, primarily in intensive care units. In adults, this research has identified endotracheal tubes, nasogastric tubes, oxygen tubing, and oxygen delivery face masks as the most common causes of MDPRIs4,6,7,12.
While urethral catheters are identified as causing MDPRIs, the incidence has not been considered high. Research focused on complications associated with the use of urethral catheters has been primarily targeted at catheter-associated urinary tract infection (CAUTI) and increased bladder and urethral pain. Penile mucosal pressure injuries in spinal injury patients with long-term urethral catheters have been reported from time to time13–15. There has been a very small number of cases reported of elderly men living in residential aged care facilities (RACFs) having mucosal pressure injuries as a result of their long-term urethral catheters9,13. Again, the incidence of this has been considered “rare”8,13,16.
Methods
The Comprehensive Aged Residents Emergency – Partners in Assessment, Care & Treatment (CAREPACT) mobile emergency team (MET) operates in the Metro South Health area which encompasses southern Brisbane, Bayside and Logan areas. The team can be mobilised to attend any of the RACFs within Metro South, currently numbering 93, with the aim of assessing and delivering an emergency department level of care at the right time in the right place to residents. The team is frequently requested to troubleshoot or replace urethral catheters for residents in order to prevent transfer to an emergency department for such procedures and predominantly review residents with more complex issues in relation to their catheter. The team are therefore in a position to frequently observe and assess urethral mucosal pressure injuries.
Anecdotally, all team members have reported high numbers of penile mucosal pressure injuries in men with long-term urethral catheters. These injuries range from a mucosal pressure injury that is relatively confined to the urethral meatus area through to pressure injuries that have cleaved the entire ventral surface of the penis down to the scrotum. Patients can experience significant pain from this type of injury, are at increased risk of urinary tract infection, and can also experience a significant negative impact on their sexual self-esteem, body image and mental health8,9. This cohort of patients are also at risk of being unable to advocate for themselves with regard to such injuries.
The CAREPACT MET revised their documentation to include the extent of any penile mucosal pressure injury that was evident in any male patients that they were requested to see for urethral catheter troubleshooting or change. The team utilised the iatrogenic hypospadias classification (IHC)11. This internationally recognised classification system outlines four grades of iatrogenic hypospadias as follows (Figure 1):
- Grade 1: cleavage is from the meatus and does not extend beyond the corona glans penis.
- Grade 2: cleavage extends from meatus to the subcoronal shaft area of the penis.
- Grade 3: cleavage is from the urinary meatus to the scrotum.
- Grade 4: meatus is not affected, but pressure necrosis is seen along the penile shaft.
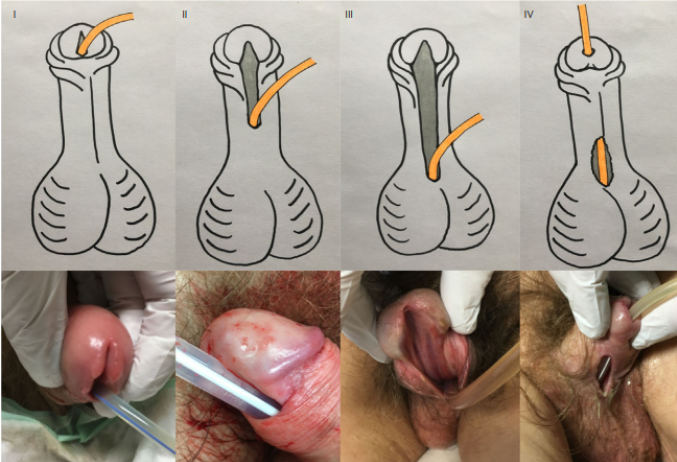
Figure 1. Examples of iatrogenic hypospadias classification
The documentation of the degree of penile injury has allowed auditing on the incidence and grade of penile mucosal pressure injuries in this cohort of patients so as to better highlight what is believed to be a previously unreported high incidence of occurrence.
Results
An audit of patients seen in a 2-month period was undertaken. A total of 51 male patients with urethral catheters were seen during this period (for either catheter troubleshooting or catheter changes). The patients were spread across 33 different RACFs, with 22 RACFs having residents with penile mucosal injuries. Of the 51 residents who were seen, 30 (58.8%) had some degree of penile injury. These were as follows:
- Grade 1 = 10 patients (19.6% of total patients).
- Grade 2 = 13 patients (25.5% of total patients).
- Grade 3 = 7 patients (13.7% of total patients).
- Grade 4 = 0 patients.
Discussion
These figures would appear to support the hypothesis that such injuries in this cohort of patients are being significantly both under-reported and underestimated. Becker et al11 report that iatrogenic hypospadias is virtually unknown to a high number of medical staff. They outline that urological referral diagnosis has often been one of the following examples: “cleft of penis”, “unknown penile condition”, “broken urethra” or “surgery required – penis looks weird”11. Evidence indicates that nurses also have a less than ideal knowledge of prevention and management of such pressure injuries5,14.
It is also postulated in the literature that since the change of nomenclature by NPUAP to differentiate between the staging of pressure injuries as opposed to mucosal- and device-related pressure injuries there has been confusion around these diagnoses1. In addition, as most clinicians consider IDCs as low risk procedure, the risk of penile mucosal injury is not usually discussed with the patient or their family.
Conclusions
This initial audit would support what has been anecdotal evidence to date that the incidence of penile mucosal pressure injury is a significant problem in the elderly, catheterised male patient. Given that the spread of patients with penile mucosal pressure injury was across 22 RACFs, this would indicate that the problem is certainly not related to just an isolated facility, but that it is widespread. To begin to understand how this problem is best addressed with preventative measures17, further research needs to be undertaken to determine the factors that contribute to the development of iatrogenic hypospadias. It is through this determination that preventative measures can be adopted with a body of evidence to support their use.
Acknowledgements
CAREPACT team, Metro South Health, QLD, Australia.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
An ethics statement is not applicable.
Funding
The authors received no funding for this study.
Author(s)
Anne-Maree Schweitzer1, Tania Parr1, Chia Hsin Tony Hsiung*2, Robert Smith3, Eva Bruce3, Patricia Hawke3
1Nurse Practitioner, CAREPACT Metro South Health, 2 Burke Street, Woolloongabba, QLD 4102, Australia
2Nurse Practitioner, CAREPACT Metro South Health, Emergency Department QEII Hospital, 2 Burke Street, Woolloongabba, QLD 4102, Australia
3Clinical Nurse, CAREPACT Metro South Health, 2 Burke Street, Woolloongabba, QLD 4102, Australia
*Corresponding author email Tony.Hsiung@health.qld.gov.au
References
- Delmore BA. Pressure injuries caused by medical devices and other objects: a clinical update. Am J Nurs 2017;117(12):36–45.
- Jaul E. A prospective pilot study of atypical pressure ulcer presentation in a skilled geriatric nursing unit. Ostomy Wound Manage 2001;57(2):49–45.
- Jackson D, Sarki A, Betteridge R, Brooke J. Medical device-related pressure ulcers: a systematic review and meta-analysis. Int J Nurs Stud 2019;92:109–120.
- Barakat-Johnson M, Barnett C, Wand T, White K. Medical device-related pressure injuries: an exploratory descriptive study in an acute tertiary hospital in Australia. J Tissue Viab 2017;26(4):236–253.
- Tan J, Cheng M, Hassan N, He H, Wang W. Nurses’ perception and experiences towards medical device-related pressure injuries: a qualitative study. J Clin Nurs 2020;29(13/14):2455–2465.
- Amirah M, Rasheed A, Parameaswari P, Nu’man O. A cross-sectional study on medical device-related pressure injuries among critically ill patients in Riyadh, Kingdom of Saudi Arabia. WCET J 2017;37(1):8–11.
- Mehta C, Ali M, Mehta Y, George J, Singh M. MDRPU – an uncommonly recognized common problem in ICU: a point prevalence study. J Tissue Viab 2019;28:35–39.
- Rassin M, Markovski I, Fishlov A, Naveh R. An evaluation of preventing pressure ulcers in the urinary meatus. Dimens Crit Care Nurs 2013;32(2):95–98.
- LeBlanc K, Christensen D. Addressing the challenge of providing nursing care for elderly men suffering from urethral erosion. J WOCN 2005;32(2):131–134.
- Ozturk H. Iatrogenic hypospadias repair caused by long-term catheterisation in a patient with neurogenic bladder: a case report. Pediatr Urol Case Rep 2019;6(5):111–113.
- Becker B, Witte M, Gross AJ, Netsch C. Iatrogenic hypospadias classification: a new way to classify hypospadias caused by long-term catheterisation. Int J Urol 2018;25(11):980–981.
- Camacho-Del Rio G. Evidence-based practice: medical device-related pressure injury prevention. Am Nurse Today 2018;13(10):50–52.
- Garg G, Baghele V, Chawla N, Gogia A, Kakar A. Unusual complication of prolonged indwelling urinary catheter – iatrogenic hypospadias. J Fam Med Prim Care 2016;5(2):493–494.
- Mansoor SN, Ayaz SB, Rathore FA, New P. Longitudinal cleavage of the penis in chronic spinal cord injury: two case reports. J Spinal Cord Med 2016;39(3):366–369.
- Bhat AL, Bhat M, Khandelwal N, Bhat A, Singh T. Catheter-induced urethral injury and tubularized urethral plate urethroplasty in such iatrogenic hypospadias. Afr J Urol 2020;26(17).
- Jindal T, Kamal MR, Mandal SN, Karmakar D. Catheter-induced urethral erosion. Urolog Nurs 2012;32(2):100–101.
- Waird A, Monaro S. Reducing the incidence and severity of pressure injuries in a high level care residential aged facility: a quality improvement project. Wound Pract Res 2021;29(2):77–85.



