Volume 5 Number 1
CrashMARCHE: a dual stream mnemonic for patient care and scene safety in response to vehicle collisions
Sam Miletta
Keywords trauma, road crash rescue, extrication, collision, pre-hospital
For referencing Miletta S. CrashMARCHE: a dual stream mnemonic for patient care and scene safety in response to vehicle collisions. JHTAM 2023; 5(1):10-16.
DOI
https://doi.org/10.33235/JHTAM.5.1.10-16
Submitted 9 February 2023
Accepted 28 March 2023
Abstract
Firefighters, paramedics, police and rescue authorities can find themselves confronted with highly chaotic and stressful situations on arrival at vehicle collisions with casualties including those who are trapped. Cognitive overload can occur as first responders find themselves juggling the responsibility of scene safety alongside patient care. This paper introduces CrashMARCHE, a dual stream mnemonic built on an existing patient care mnemonic (MARCHE) developed in the tactical medicine sub-discipline. CrashMARCHE adds a scene safety stream, prompting users to undertake certain tasks to improve their safety and that of others on the scene. This model is scalable to individual training, skills and agency procedures and is encouraged to be used by all involved in this type of response. It intends to prompt first responders to undertake key life-saving actions whilst also establishing a safe work environment. It is hoped this model will be considered for inclusion as part of formal training and qualifications as well as organisational procedures.
Introduction
During the response to vehicle collisions with casualties including those who may be trapped, those first arriving on the scene are often faced with the need to balance their priorities between patient care of any injured parties and ensuring scene safety, including safety to themselves. For the first arriving agency, this is critically important until they can handover the patient care responsibility or scene safety element to the appropriate service. While internal processes and shared models and training likely exist within various agencies around the world, it has been difficult to locate a universal model with applicability to all services that deal with these scenes.
Therefore this paper aims to provide firefighters, paramedics, police, rescue technicians, or anyone else responding to such incidents, a single mnemonic with a dual stream format covering key life-saving patient care priorities alongside scene safety considerations. The mnemonic proposed is MARCHE1, a pre‑existing mnemonic for patient care and assessment borne out of the medical sub-discipline of tactical medicine. The author has identified key scene safety considerations and created a scene safety stream following the MARCHE mnemonic, with the term CrashMARCHE used to distinguish this proposed model. Users will be able to follow the M-A-R-C-H of the scene safety and patient care streams before bringing both together where the E is proposed as Extrication, to prompt the safe removal of the patient from the vehicle (Figure 1).
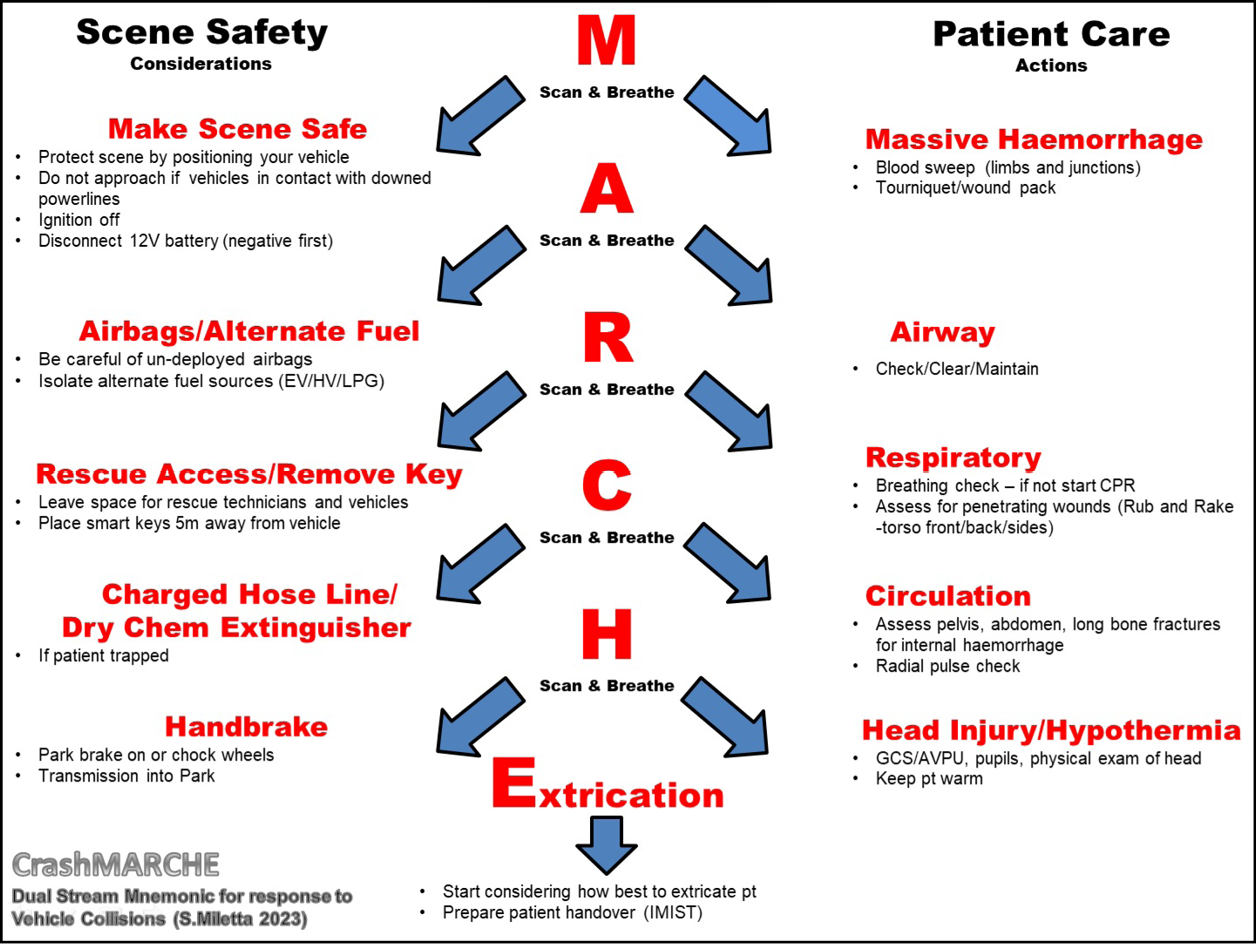
Figure 1. Proposed vehicle collision dual stream scene safety / patient care model – CrashMARCHE
Rather than multiple mnemonics to remember for the same situation, CrashMARCHE allows responders to follow a single mnemonic, but with two streams to balance their priorities in the early stages of an incident. It is aimed as a prompt to reduce the cognitive load on the user during a potential period of heightened stress. The model is intended to be scalable depending on the individual’s training, available equipment, agency protocols, and presenting situation. A similar conceptual model has been developed and used for the response to chemical, biological, radiological and nuclear (CBRN) incidents with (MARCHE)2 providing a framework that balances patient care alongside safety and decontamination actions2.
Background
The need for a tool to aid first responders
Vehicle collisions with casualties, especially trapped occupants, can present a challenging and stressful situation for first responders. They generate circumstances involving potential life threat, uncertainty, and a need for immediate action all within an environment that limits an individual’s ability to control certain aspects. These are factors consistent with what has been termed a ‘crises’ situation, where levels of stress and arousal are heightened.
Stress can be described as a result of “a perceived imbalance between the demands of the emergency situation and your ability to meet those demands where failure to do so has important consequences to you”3. Cognitive faculties used for task performance can be impaired by excess stress, thus resulting in a decrease of effective and quality decision making, problem-solving and situational awareness, likely leading to poor outcomes3. No matter what uniform is worn, there is a likely expectation by the community that those first responders arriving on scene will assist regardless of their role or skillset. The pressure of this community expectation, along with other factors presenting at vehicle collision scenes, may quickly see the initial first responders overwhelmed with that need to balance scene safety and patient care.
Evidence suggests that military personnel who were adequately prepared to undertake their role whilst on operational deployments had a reduced likelihood of developing mental health problems as a result4. Other research supports this by suggesting that poor psychological outcomes are associated with a lack of preparedness5. Reports of dissociation and depression symptoms are more probable for those who experience the perception of low levels of safety during traumatic events6.
While training can improve confidence, there is still limited evidence on exactly how this will translate to post-incident mental health outcomes; however, providing a tool to first responders in these situations is likely to better prepare them to respond and balance the stress experienced on scene, improve their safety and perception of safety, as well as guide improved patient care activities. The benefits should translate to the individual, the patients they are treating, and the community as a whole.
Origins of MARCHE
The MARCHE mnemonic and its versions were borne out of medical lessons learned on the battlefield which were later transitioned to the civilian setting by the Committee for Tactical Emergency Casualty Care7. MARCHE provides a patient assessment and treatment process that prioritises the treatment of life-threatening injuries to address the leading preventable causes of death, listed later in this paper. Additionally, it aims to identify potential haemorrhagic shock, while considering the lethal triad, and the detrimental effects hypothermia has on trauma patients8.
While versions of MARCHE maintain the same M-A-R-C-H format, the addition of E in some models represents Eye injuries or Everything else1. For CrashMARCHE, E has been selected to represent Extrication relevant to the vehicle collision environment it is designed for. Whilst the origins of MARCHE are built on the need for trauma care in tactical and high-threat environments, its use can be argued to be a more thorough and effective process for the treatment of all trauma patients when compared to the traditional ABC (airway/breathing/circulation) approach9,10. Whilst pre-hospital care clinicians may opt to switch their ABC to CAB in trauma patients, this process and the process taught in first aid courses fall short when compared to MARCHE in identifying and promoting the treatment of life-threatening traumatic injuries and the prevention of hypothermia in trauma patients.
The Australian Resuscitation Council (ARC) Guidelines11 state that “in life-threatening bleeding, control of bleeding takes priority over airway and breathing interventions”; however, this is not reflected in the patient care mnemonic DRSABCD (danger/response/send for help/airway/breathing/CPR/defibrillation). A closer look at the ARC guidelines uncovers that the DRSABCD mnemonic provided in their basic life support (BLS) flowchart is recommended for use in patients who are “unresponsive and not breathing normally”12. Despite this, DRSABCD and its versions are the standard patient care/primary survey mnemonic taught in first aid and many pre-hospital care courses, even for conscious trauma patients.
A 2017 article on a version of MARCHE used by US Airforce pararescuemen (PJs), known as MARCHE-PAWS, identified its effectiveness in not only treating battlefield injuries but also “at treating a vast majority of non-battle related injuries”9. In this study, 45.1% of the 465 patients surveyed had sustained non-battle related injuries or sickness. Of these patients, 94.9% received treatments within the MARCH-PAWS mnemonic9. Whilst it could be argued this mnemonic’s effectiveness had four extra prompts added within the PAWS element, it should be acknowledged that the research looked beyond just the initial stages of patient care, and therefore PAWS likely played a role later on in the patients’ management.
This research demonstrates the applicability of MARCHE beyond the tactical or battlefield environment and supports a need for further research assessing its effectiveness in civilian trauma settings. Currently, there is a lack of research comparing the two primary survey methods. This literature gap limits the ability to argue the effectiveness of one method over the other, apart from highlighting the additional trauma-related considerations tabled within MARCHE when compared against DRSABCD.
The dual stream model
While this paper will not address stress mitigation strategies in depth, it is arguing for a dual stream mnemonic, with CrashMARCHE used as a prompt for first responders to start undertaking both key scene safety and patient care tasks. Checklists are recognised within the medical field to help guide invasive procedures, reduce errors and improve outcomes. Within operational environments, checklists may not be practical; however, that is where mnemonics can play an effective role9.
While there is limited research on this topic, confusion generated by too many acronyms is a reality, with a risk that users of first-letter mnemonics incorrectly remember certain words within it13. CrashMARCHE has tried to reduce that likelihood by building upon an already existing mnemonic which has been gaining more attention within the medical field. Users can also choose to adopt the patient treatment stream for a range of trauma care settings beyond just vehicle collisions.
The use of core algorithms by medical staff has identified benefits for patients by providing more structured pathways informing treatments within clinical settings, therefore similar processes for frontline staff are envisioned to create comparable benefits14 – “In stressful situations, decision-making is most effective when those in charge have simple tools to help them remember the main tasks that must be performed”15. Self-talk has been researched and used to improve performance under stress, with evidence suggesting that a ‘cue word’ providing an instructional statement can activate selective attention and concentration3. Training on a specific mnemonic could increase long-term memorisation and assist in prompting critical tasks in these vehicle collision situations16.
Bortle13 discusses stress acronyms, used to remember simple tasks and sequences in stressful settings, verse memory acronyms, used to recall rarely used information in non-stressful settings. His research identified that “while medical practitioners know fewer stress acronyms than memory acronyms, they may use the stress acronyms more frequently”13. This finding supports this paper’s justification for a mnemonic to inform actions in these stressful road trauma settings. Participants in Bortle’s research also discussed their use of mnemonics during the early stages of their careers before they had obtained real-life experience, with some no longer needing the prompting as their experience grew. That shows the potential adaptability for CrashMARCHE to be used as a prompt during stressful situations for both experienced and inexperienced individuals. Even high-performing surgical teams have benefited from checklists during crisis scenarios to guide actions16, and CrashMARCHE can be viewed as just that.
Shared mental models have been identified in improved performance of trauma teams as they “are assumed to enable team members to predict task needs and the actions of other team members by offering an immediate and internalised understanding of how team members coordinate behaviour and choose different actions without explicit demands being made for coordination”17. By adopting this dual stream mnemonic, first responder teams are likely to interact and perform better in these situations as all team members are following the same process with improved understanding. If adopted by an organisation, shared knowledge means that colleagues can come in at any stage of the process and assist through simple communications or commands such as “I have completed MAR of patient care, can you take over from Circulation while I make the vehicle safe”. Or they may just begin undertaking scene safety activities if they notice the patient is already being treated effectively. Additionally, if multiple agencies within a jurisdiction adopt this system, improvements in shared understanding and communications will likely improve performance within multi-disciplinary teams operating at these scenes. This may also improve post-incident mental health outcomes for first responders as there is evidence to suggest that team-based skills training and team cohesion can reduce PTSD and common mental disorders18.
The users of this proposed mnemonic can break it down by each letter to help prevent cognitive overload, allowing them to focus on key critical tasks one by one. While first responders may initially need to refer to a reference card or prompt, with increased training and operational use it is aimed that this mnemonic will eventually become a well-versed process that just flows for those who use it often. For others, it remains a process they can refer to when confronted with vehicle collisions with patients suffering traumatic injuries.
The CrashMARCHE model
Beating the stress – scan and breathe
In high-stress or crisis situations, people can be overwhelmed with difficulty in processing pieces of information or may have short-term memory deficits3. To aid some of these factors, CrashMARCHE acts as a list of actions that can be broken down into small tasks to achieve the overall objectives of scene safety and life-saving patient care. However, we know that stress can affect our memory and likely limit our ability to remember a whole mnemonic. An ability to think clearly and act decisively, maintain situational awareness, enhance memory recall, and perform key tasks is likely to occur when we train our bodies and undertake actions to mitigate stress3.
This is where the scan and breathe comes into play to further aid users of CrashMARCHE in managing the stress and resulting physiological responses. “Respiration is the only autonomic function that can be controlled and modified consciously”3, so users of CrashMARCHE are encouraged to apply breathing techniques as a quick and effective tool to counter their body’s stress response. Controlled, slow, deep breathing can reduce pulse rate, a key physiologic indicator of stress3.
As seen in Figure 1, ‘scan and breathe’ is included as a repeating prompt to remind the user to take a short pause to maintain their situational awareness and refocus on the task at hand. The pause in your actions needs only to be a second or two but is advised to be trained on and practised so that, under stress, the user can counter some of their body’s stress responses such as fixation (tunnel vision)19. The user is advised to take a deep controlled breath, raise their head, and have a quick look around their surroundings. This action can help re-orientate them to the tasks at hand while identifying any changes in the environment which may affect their safety19.
Scene safety stream
During the initial stages of a vehicle collision, especially those with trapped casualties requiring extrication, a balance between patient care and establishing a safe scene/work environment is paramount. Firefighters, paramedics, police and rescue authorities can find themselves juggling these roles until supported by further resources or emergency service colleagues directly responsible for those tasks. While casualties may need immediate care, the safety of those providing that care is crucial so as to not become victims themselves. Therefore the author has developed a scene safety stream using the established mnemonic of MARCHE to provide a list of considerations and potential actions to improve safety (Figure 2).
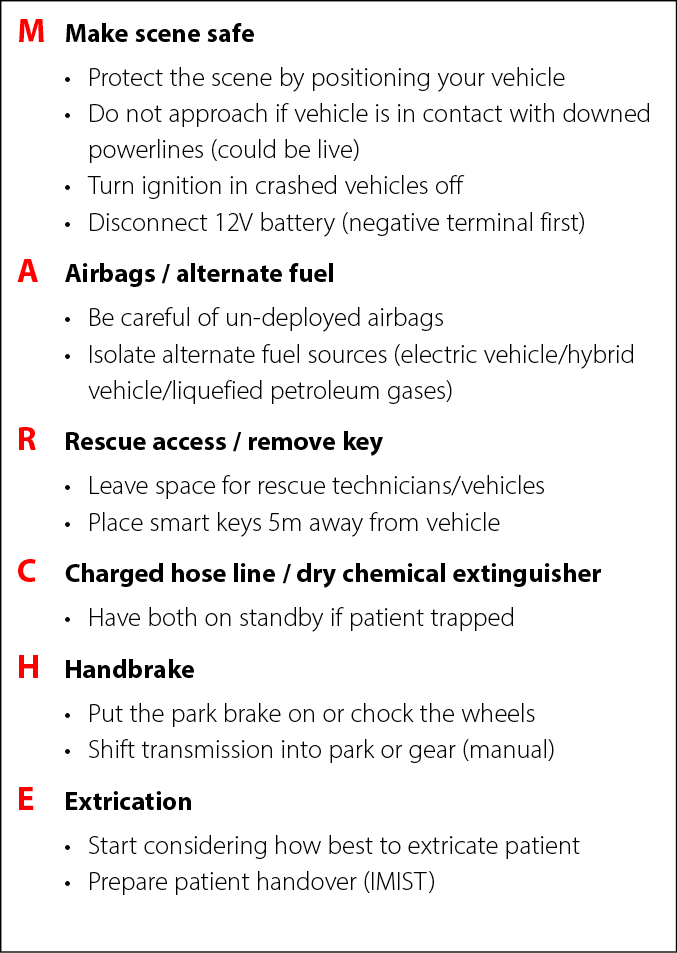
Figure 2. The CrashMARCHE scene safety stream considerations
Unlike the patient care stream, the scene safety stream is intended as more of a checklist and not a set order of specific actions to follow. It is again scalable to the individual’s training, available equipment, agency protocols, and presenting situation. The need to protect the scene, turn the ignition off, activate the park brake, and be cautious of un-deployed airbags is reflected in ARC guidelines for managing an emergency20. The dangers of working on the roadside are often highlighted by the many cases of first responders experiencing injuries or near-misses while operating at collision scenes. Scene protection is achieved first and foremost with the positioning of vehicles or warning equipment critical to alert oncoming drivers of the incident to protect those operating within. If the collision has involved any power poles or electrical equipment, vehicles should not be approached if they are in contact with downed lines or structures that are potentially live, due to the risk of electrocution21. If there are no live power concerns, proceed to turn the ignition off and apply the park brake on any crashed vehicles so the risk of them moving is reduced. It should be noted that tasks like opening windows or moving powered seats should be completed before turning the ignition off22.
Un-deployed airbags are a common concern often discussed in the extrication field, although data on incidents of first responders injured by un-deployed airbag systems are almost non-existent23. While it is important to be mindful of the risk, the likelihood of this happening should be kept in context when you consider how many vehicle collisions and extrication operations take place around the world daily without incident23.
The disconnecting of the 12V battery, removal of smart keys, and isolating alternate fuel sources all aid in reducing ignition sources and other risks that present when the vehicle is still powered22. The vehicle’s smart key should be placed approximately 5m from the vehicle to prevent the signal from still being able to operate the vehicle22.
The remainder of the considerations helps to improve operations. Having a charged hose line and dry chemical extinguisher readily available provides a quick ability to extinguish a fire and protect any trapped occupant/s should a fire ignite in the crashed vehicle. Access for rescue technicians and equipment makes for more efficient operations once those resources arrive.
It should be reiterated that the tasks suggested above are only considerations and should only be undertaken by those trained and authorised to do so. Tasks like disconnecting the 12V battery can cause sparks and present a danger if done incorrectly so users of this model should only carry out the actions they are trained and capable of. Extrication will be discussed later on in this paper.
Patient care stream
Vehicle collisions provide a mechanism for considerable traumatic injuries for those involved. With this mechanism of injury in mind, the MARCHE mnemonic provides a structured process scalable to all levels of first aid/medical training, allowing those providing care to address the leading preventable causes of death, identify other injuries and the potential for shock, and prevent hypothermia in trauma patients. The patient care stream is presented in Figure 3.
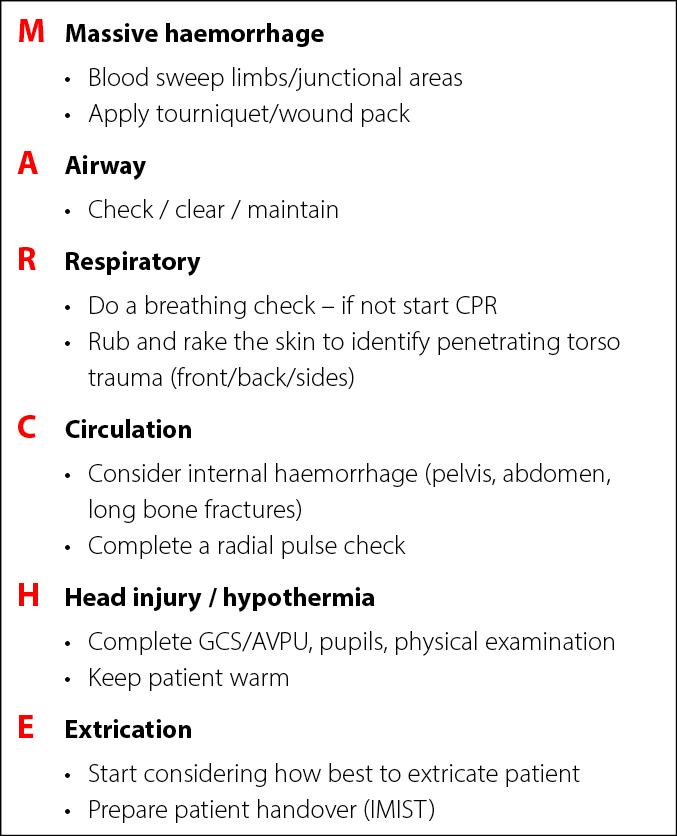
Figure 3. The CrashMARCHE patient care stream considerations
The first steps of this mnemonic, the M-A-R, are designed to address the three leading preventable causes of death, haemorrhage, airway obstruction and tension pneumothorax, in the specific order that these injuries are likely to prove fatal for patients24. Firstly, ensure the patient is not suffering from a life-threatening bleed from any limbs or junctional areas (axilla, neck, pelvic region). If they are, apply a tourniquet or wound pack to control the haemorrhage8. Once controlled, ensure the patient has an open and clear airway and has an ability to maintain this. Then ensure the patient is breathing and assess the torso, front/back/sides, for any penetrating trauma using a rub and rake motion with your hands. The Committee for Tactical Emergency Casualty Care (C-TECC) guidelines advise the use of a chest seal for penetrating injuries and to monitor for any deterioration in the patient’s breathing which could be a sign of tension pneumothorax, a serious condition requiring advanced clinical care25.
Next the C for Circulation part of the process aims to identify signs of haemorrhagic shock, a life-threatening condition caused by major blood loss. The pelvic region, abdomen, chest and long bone fractures, such as the femur, are areas of the body where patients can suffer significant internal haemorrhage which can lead to death26. Locating or suspecting potential fractures or internal haemorrhage in these areas assists in recognising the urgent need for advanced care for patients. The radial pulse check is listed in the C-TECC guidelines8 as the absence of a radial pulse can present as a significant, but late, finding of haemorrhagic shock26. The responder should not get caught up in having to locate this pulse though, rather use it as a quick field indicator.
In H for Head injury/hypothermia, the care provider is prompted to assess and identify any potential head injury in the patient through both a physical examination of the head and face, and a neurological exam, using the Glasgow Coma Scale for those trained in its use27 or the simpler to use AVPU score (Figure 4)28.
The next part of H is to check the patient’s pupils to ensure they are equal and reacting to light, with deficiencies in this alerting the care provider to a potentially serious head injury29. The second part of this step focuses on hypothermia. The lethal triad is a concept that occurs in trauma patients with severe haemorrhage30. Blood loss leads to a vicious cycle of hypothermia, reduced clotting abilities, and acidosis in the patient. Patient outcomes can be improved by keeping this in mind and keeping trauma patients warm30.
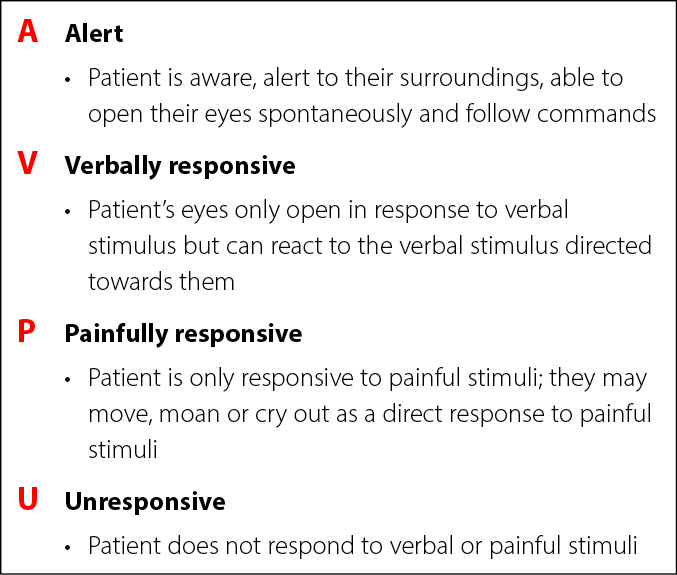
Figure 4. AVPU scale
Extrication
The final part of this model proposes E for Extrication which aims to bring the scene safety stream and patient care stream together to close off the initial actions and prepare for the transition to the next stage where advanced patient care and specialist road crash rescue activities, if needed, are undertaken by the responsible agencies.
In Extrication, it is advised to start considering how best to get these patients out of the vehicle. This does not mean you are going to be extricating them. However, assess the situation – get an idea if and how the casualty is trapped, consider what measures may help in the process, and have this information ready to handover to arriving rescue technicians. This information can help provide them with earlier situational awareness and can aid in their planning and decision-making when they take over rescue activities.
During this period it is also advised to start obtaining patient details and prepare to handover the patient. For patient handover, IMIST is advised for its efficiency in covering key information for medical care providers, including some basic vital signs, pulse rate, respiration rate, and consciousness level31 (Figure 5). This can be delivered as a verbal handover covering just key information on the patient’s injuries and status.
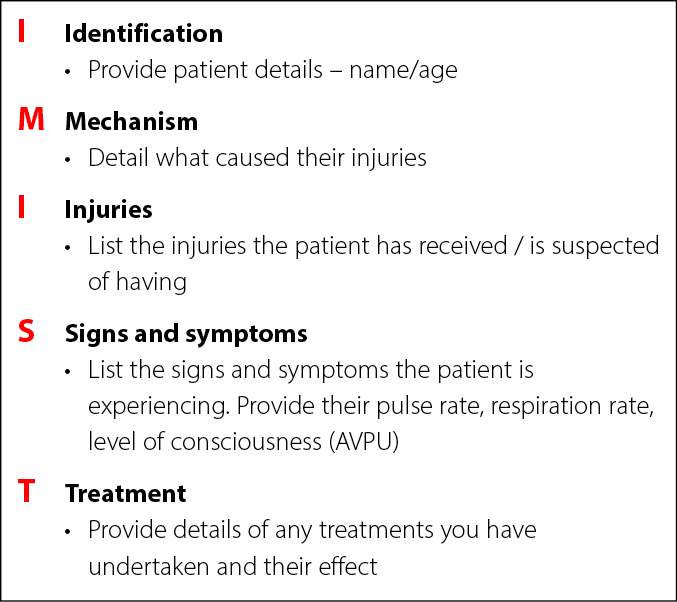
Figure 5. IMIST handover information
Conclusion
This paper has proposed the application of CrashMARCHE, a dual stream mnemonic for use by all firefighters, paramedics, police, rescue authorities, or anyone else during the initial stages of their arrival at vehicle collisions with casualties, especially those with trapped casualties. It has built upon the existing MARCHE mnemonic used in the tactical medicine sub-discipline to improve safety and patient care. Its use is aimed to reduce the cognitive load on the user and provide them with evidence-based and structured guidance and considerations to assist their actions and decision-making in what can be chaotic and highly stressful situations. This model is scalable to an individual’s scope of practice and is able to be used within multi-disciplinary team environments as a shared mental model improving understanding and performance. It should be emphasised that actions undertaken by the individual should be in-line with their training, available equipment, and agency procedures. The scene safety considerations are provided as a prompt to create a safer scene, not as a must-do list if certain activities are beyond that individual’s scope or abilities.
The adoption of this model is aimed to equip first responders with an aid to prompt decision-making and influence actions to improve patient outcomes and establish safer conditions when working on the scenes of vehicle collisions. It is hoped that this dual stream mnemonic is considered for inclusion in nationally and internationally recognised and certified training programs, individual agencies’ training and procedures, and adopted by those individuals reading this who are undertaking professional development hoping to improve their knowledge. Whilst not an exhaustive list of actions to mitigate these incidents, it is designed to highlight key actions to improve patient outcomes and safety during incidents that may present as quite chaotic and overwhelming for the initial arriving responders.
Barriers to implementation may exist in the absence of widespread use of MARCHE within civilian settings. While MARCHE is gaining more momentum and recognition as a beneficial trauma care primary survey beyond the military setting, its use and related outcomes within the civilian context remain significantly under-researched. First aid qualifications within Australia have traditionally been aligned to DRSABCD with a need to contextualise and expand beyond that process evident within this paper. It is hoped that this will encourage further research investigating the effectiveness of the MARCHE and CrashMARCHE mnemonics against other mnemonics. Optimistically, future research will bolster the justification for widespread adoption of the model or, alternatively, identify elements for improvement within the CrashMARCHE proposal.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Sam Miletta
School of Paramedic Science, Central Queensland University, Australia
*Corresponding author email s_miletta@outlook.com.au
References
- Shertz M. MARCH versions; 2018 [cited 2022 Mar 20]. Available from: https://www.crisis-medicine.com/march-versions/
- DeFeo D, Givens M. Integrating chemical biological, radiologic, and nuclear (CBRN) protocols into TCCC introduction of a conceptual model – TCCC + CBRN = (MARCHE)2. J Spec Oper Med 2018;18(Spring):118–23.
- Lauria MJ, Gallo IA, Rush S, Brooks J, Spiegel R, Weingart SD. Psychological skills to improve emergency care providers’ performance under stress. Ann Emerg Med 2017;70(6):884–90.
- Wild J, Greenberg N, Moulds ML, Sharp ML, Fear N, Harvey S, et al. Pre-incident training to build resilience in first responders: recommendations on what to and what not to do. Psychiatry 2020;83(2):128–42.
- Brooks SK, Dunn R, Amlôt R, Greenberg N, James Rubin G. Training and post-disaster interventions for the psychological impacts on disaster-exposed employees: a systematic review. J Ment Health 2018;2018:1–25.
- Lanza A, Roysircar G, Rodgers S. First responder mental healthcare: evidence-based prevention, postvention, and treatment. Prof Psychol Res Pract 2018;49(3):193–204.
- Callaway DW, Smith ER, Shaprio G, Cain JS, McKay SD, Mabry RL. The Committee for Tactical Emergency Casualty Care (C-TECC): evolution and application of TCCC guidelines to civilian high threat medicine. J Spec Oper Med 2011;11(2):94–9. Available from: https://www.c-tecc.org/images/content/C-TECC-JSOM-Spring-11.pdf
- Committee for Tactical Emergency Casualty Care. Guidelines; 2023 [cited 2020 Aug 22]. Available from: http://www.c-tecc.org/guidelines
- Kosequat J, Rush SC, Simonsen I, Gallo I, Scott A, Swats K, et al. Efficacy of the mnemonic device “MARCH PAWS” as a checklist for pararescuemen during tactical field care and tactical evacuation. J Spec Oper Med 2017;17(4):80–4.
- Duckworth R. EMS trauma car: ABCs vs. MARCH EMS1; 2017 [cited 2022 Mar 20]. Available from: https://www.ems1.com/trauma-assessment/articles/ems-trauma-care-abcs-vs-march-vdnYK1J4Pq5cZbnV/
- Australian Resuscitation Council. ANZCOR guideline 9.1.1 – first aid for management of bleeding vol. 9.1.1. Australian Resuscitation Council Guidelines; 2021. Available from: https://resus.org.au/download/9_1_trauma/anzcor-guideline-9-1-1-bleeding-april-2021.pdf
- Australian Resuscitation Council. ANZCOR basic life support flowchart; 2021 [cited 2022 Mar 20]. Available from: https://resus.org.au/download/flowcharts/anzcor-basic-life-support-flowchart-april-2021.pdf
- Bortle CD. The role of mnemonic acronyms in clinical emergency medicine: a grounded theory study. University of Phoenix 2010 [cited 2023 Feb 28].
- Watterson LM, Morris RW, Williamson JA, Westhorpe RN. Crisis management during anaesthesia: tachycardia. BMJ Qual Saf 2005;14(3):e10–e10.
- Giaume L, Daniel Y, Calamai F, Derkenne C, Kedzierewicz R, Demeny A, et al. “I AM THOR/DUST DAHO”: mnemonic devices used by the Paris Fire Brigade to teach initial measures in undertaking a CBRN event. Crit Care 2021;25(1):1–3.
- Arriaga AF, Bader AM, Wong JM, Lipsitz SR, Berry WR, Ziewacz JE, et al. Simulation-based trial of surgical-crisis checklists. N Engl J Med 2013;368(3):246–53. doi:10.1056/NEJMsa1204720
- Westli HK, Johnsen BH, Eid J, Rasten I, Brattebø G. Teamwork skills, shared mental models, and performance in simulated trauma teams: an independent group design. Scand J Trauma Resusc Emerg Med 2010;18(1).
- Tan L, Petrie K, Deady M, Bryant RA, Harvey SB. Systematic review of first responder post-deployment or post-incident psychosocial interventions. Occup Med (Lond) 2022;72(3):160–9.
- Harris B. Can TP be a lifesaver? Trauma Monkeys blog [cited 2022 Mar 28]. Available from: http://www.traumamonkeys.com/blog/tp
- Australian Resuscitation Council. ANZCOR Guideline 2: managing an emergency; 2021 [cited 2022 Jul 29]. Available from: https://resus.org.au/download/section_2/anzcor-guideline-2-managing-an-emergency-apr-2021.pdf
- Boyle J. Understanding step and touch potential incident prevention blog; 2013 [cited 2022 Mar 29]. Available from: https://incident-prevention.com/blog/understanding-step-and-touch-potential/
- Firefighter Nation Staff. Power isolation for vehicle incidents;2009 Sep 30 [cited 2022 Mar 20]. Available from: https://www.firefighternation.com/firerescue/power-isolation-for-vehicle-incidents/#gref
- Dunbar I. Airbag deployment during extrication. International Fire Fighter 2019 Sep 9 [cited 2022 Mar 20]. Available from: https://iffmag.mdmpublishing.com/airbag-deployment-during-extrication/
- Eastridge BJ, Mabry RL, Seguin P, Cantrell J, Tops T, Uribe P, et al. Death on the battlefield (2001–2011): implications for the future of combat casualty care. J Trauma Acute Care Surg 2012;73(6 SUPPL. 5):431–7.
- Sahota RJ, Sayad E. Tension pneumothorax. StatPearls 2021.
- Kowalski A, Brandis D. Shock resuscitation. StatPearls 2021.
- Royal College of Physicians and Surgeons of Glasgow. Glasgow coma scale [cited 2022 Mar 20]. Available from: https://www.glasgowcomascale.org/
- Romanelli D, Farrell MW. AVPU score. StatPearls 2021.
- Chowdhury T, Kowalski S, Arabi Y, Dash HH. Pre-hospital and initial management of head injury patients: an update. Saudi J Anaesth 2014;8(1):114–20.
- Moffatt SE. Hypothermia in trauma. Emerg Med J 2013;30(12):989–96.
- Iedema R, Ball C, Daly B, Young J, Green T, Middleton PM, et al. Design and trial of a new ambulance-to-emergency department handover protocol: ‘IMIST-AMBO.’ BMJ Qual Saf 2012;21(8):627–33.