Volume 5 Number 1
Public order medicine: an operational sub-speciality within UK high threat medicine
Sean Brayford-Harris, Nicolas Mattock, Andrew Barrett, Claire Park
Keywords tactical combat casualty care, High threat medicine, police, pre-hospital care, public disorder
For referencing Harris S et al. Public order medicine: an operational sub-speciality within UK high threat medicine. JHTAM 2023; 5(1):17-26
DOI
https://doi.org/10.33235/JHTAM.5.1.17-26
Submitted 9 January 2023
Accepted 8 March 2023
Abstract
This paper examines the history and current provision of medical care within public order (PO) situations in the United Kingdom (UK). In exploring the definitions and categories of disorder, it describes a high threat, non-permissive environment that can be compared to the threat of a firearms environment, an area in which high threat medicine, tactical medicine or tactical emergency medical support (TEMS) has been formally recognised. Although UK PO scenarios are only rarely associated with firearms discharges, after considering the unique challenges, characteristics, prevalence and injuries arising within this particular environment, the paper proposes that PO medicine should be recognised as an operational sub-speciality of UK high threat medicine in its own right. The obligations of those groups potentially providing care within PO has some bearing on the care that can be provided. This paper examines the UK legal powers, equipment, experience and training requirements to assist pre-hospital care providers in the recognition and development of this unique sub-speciality both in the UK and internationally.
Introduction
The concept of civilian high threat medicine, tactical medicine or tactical emergency medical support (TEMS) is still in its infancy in the United Kingdom (UK). Even more so is the sub-speciality of public order (PO) medicine – the provision of medical care during violent disorder – which is rarely considered in comparison to ballistic threat. However, the lack of representation and lack of definition in the medical literature is surprising considering the severity of civil disturbance and disorder seen in the UK over the past 4 decades1–3.
High threat medicine is most commonly associated with a firearms or explosive threat4,5; however, it is important to recognise that there are alternative categories of threat, whether interpersonal or environmental. Whilst none of the factors are unique to disorder in isolation, no other field of medicine is required to deliver point of wounding care in an environment with a combination of dense crowds6, direct physical assaults with or without weapons7–9, and the use of chemical incapacitants10–12, corrosive substances13, projectiles, including attenuated energy weapons14,15, incendiary devices9,16,17, deliberate or accidental vehicular collisions5, horses18,19, and protected vehicles20,21. Only in public disorder do these risks overlap to create a dynamic environment too dangerous for conventional medical assets and therefore necessitating specialist training, equipment and experience, distinct from those employed in a ballistic or explosive threat environment5.
When looking at 313 riot-related injured civilians (n=225) and police officers (n=88) conveyed to hospital during disorder in Beirut, reported injuries included upper extremity soft tissue or orthopaedic injury (n=103), lower extremity soft tissue or orthopaedic injury (n=72), head, neck and facial injuries (n=47) or multiple injuries (n=34). The majority of these injuries were caused by direct interpersonal violence (n=100) closely followed by indirect projectiles (n=88). Stones, rocks and gas canisters were the most common causes of injury. Although the majority of patients were seen, treated and discharged home (n=291), many required imaging (n=241), wound management (n=88) and/or medication (n=235). A small proportion required admission to critical care (n=3), general wards (n=12) or surgery (n=8)7.
The violence experienced in Northern Ireland, described as ‘The Troubles’ saw over 2600 people killed and 30,000 injured between 1969–198922. The PSNI (Police Service of Northern Ireland), formally the RUC (Royal Ulster Constabulary), has experienced decades of policing violent disorder23. Between 1969 and 1972, over 800 police officers were treated for riot-related injuries in one hospital alone9. In 2005, the ‘Belfast riots’ which included small arms fire, improvised explosive and incendiary devices, saw 81 PSNI officers injured alongside multiple civilians24. In 2013, five PSNI officers were significantly injured during a violent demonstration at Belfast City Hall25. In the first 2 weeks of April 2021, 88 PSNI officers were injured in widespread rioting across Northern Ireland8.
During the English inner-city riots of the early 1980s, at least 1000 officers were injured, and one killed, in 14 cumulative days of rioting26,27. PC Keith Blakelock was stabbed 43 times and murdered whilst attempting to protect firefighters in Tottenham’s Broadwater Farm estate28. Later, during the 1990s, there were several significant violent demonstrations in Central London, for example the Poll Tax riots which were attended by approximately 25,000 people, resulting in extensive violent disorder including 542 injured police officers29. The summer of 2011 saw violence erupt in London and spread across England following the police shooting of Mark Duggan, resulting in five civilian deaths and large numbers of both police and civilians injured30,31. In one night, the Metropolitan Police Service announced they had been stretched to invisibility after experiencing a 400% increase in demand32.
In the last 2 years, the UK has seen disorder as a result of protests regarding climate change, ‘Brexit’ and ‘Remain’, women’s rights, the Police, Crime, Sentencing and Courts Bill 2021 and structural and historic racism in the UK. In June 2020, at least 27 police officers were injured in the Black Lives Matter protests in London33, with recorded injuries including sprains, bruising, cuts, loss of consciousness due to head injury, maxillo-facial injuries and long bone fractures34. Disorder in Bristol in 2021 saw 46 officers and at least 62 members of the public injured, including bruises of varying severity, cuts, puncture wounds, ligament damage, paint and irritant spray in eyes and long bone fractures35,36.
The global SARS-CoV-2 pandemic and associated public health initiatives including vaccinations, lock-downs and breaches therein have also prompted disorder resulting in injuries to police officers37. Following the cessation of public health restrictions and return to stadia, the UK has experienced a 59% increase in football related arrests, most commonly for disorder or violent disorder38; high profile examples include the violence seen at the 2020 European Cup Final at Wembley39. The nature of the dynamic UK socio-economic, political and health climate ensures that the threat of disorder will remain.
Defining public order medicine
Public order vs disorder
The literal interpretation of PO is fundamentally the absence of disorder – the peaceful and orderly behaviour of people in public spaces40. Disorder, as an opposing state to that of PO, is defined in the UK by the Public Order Act 198641. Disorder ranges from causing harassment, alarm, distress and fear of violence through to affray, violent disorder and rioting. Disorder can be an individual use of threatening or abusive words through to large groups using unlawful violence collectively for a common purpose.
Within policing, public order and public safety (POPS) (often shortened to public order or PO) is the term given to situations where routine PO may be disrupted, applying more generally to crowd management situations, be these spontaneous incidents or during pre-planned, local, regional or national events42. This may arise from events including large-scale sporting, music or ceremonial events through to public gatherings, assemblies, demonstrations, protests and processions where crowd management for the sake of maintaining PO is necessary.
The police use a disorder model to categorise the nature of disorder on a scale ranging from a state of normality, in which no specialist or additional policing is required, rising through tension, disorder, serious disorder/riot and, lastly, unrest being the most serious43. Each stage of the model has a fixed description to assist in providing an objective measure. Tension describes a level of concern or feelings within a community, group or crowd43. Disorder describes when this tension manifests in disruption, damage or violence43. Serious disorder/riot is where this behaviour becomes widespread43. In simple terms, PO policing exists in a variety of forms and is, crucially, not limited to large events.
Event medicine vs public order medicine
At large events such as festivals or sporting events, the pre-planned provision of medical care is described as event medicine – an informal sub-speciality of pre-hospital emergency medicine (PHEM). Although there is no current legislation regulating event medicine, event planners are required to submit risk assessments and provide appropriate medical resources; this can range from basic first aiders and simple tentage to registered healthcare professionals and ambulances44. Large events are routinely attended by PO policing assets and, by the nature of their presence, these police officers may come into contact with patients. However, if a medical incident occurs during a non-hostile/permissive period of an event, the pre-planned medical infrastructure is tasked and expected to manage most routine presentations without impacting on police resources.
It is important to acknowledge that PO and event medicine are two separate operational specialities that can exist within the same geographic footprint. The key difference is that during periods of tension, disorder or serious disorder, when the environment shifts towards being hostile/non-permissive, any pre-planned event medical resources are unlikely to able to respond safely within the environment due to the existence of a threat.
The Brixton Academy incident, occurring in South London during December 2022, is a prime example of this transition from event medicine to PO medicine. The Metropolitan Police Service reported receiving multiple calls to a large crowd outside of a ticketed music venue who were described as attempting to force entry into the venue45. The crush resulted in one arrest, two deaths (including a member of event security staff) and eight hospitalisations46. The safe or effective management of a large crowd forcing entry into a building or the care of any casualties within that crowd is likely to fall outside of the capabilities of any event medical or security provider, triggering requests for police support and a transition into PO medicine. This transition is likely to remain in place until patients are extricated to safety or the policing operation is able to reduce the threat, re-enabling event medical providers or facilitating access by emergency service partners, as reflected in other form of high threat incidents.
Public order medicine within high threat medicine
Internationally, the dominant model of high threat medicine arises from the work of Butler et al47 which exists today in the form of TCCC (tactical combat casualty care), the United States military guidelines for trauma life support in pre-hospital combat medicine48. TCCC was modified for civilian application by Smith and Callaway4. The authors recognised that conventional civilian medical response models were “inadequate” for high threat situations, resulting in tactical emergency casualty care (TECC) guidelines49. TECC is closely related to TCCC, although the civilian-orientated TECC guidelines allow for a more subjective evaluation of the threat, acknowledging that the civilian experience may differ from military combat scenarios, and includes guidelines for all range of patients including paediatric and the elderly.
The increasing international awareness of ‘civil disturbance’ as an area of high threat that should also be considered in these guidelines has led to a recent change in the TECC guidelines to stress that such medicine is relevant to a number of different threat situations49. Both TCCC and TECC divide high threat medicine into three phases, each determining the appropriate clinical actions depending on the variable level of threat. This three-phase interpretation of high threat medicine is further demonstrated in NATO (North Atlantic Treaty Organisation) military guidelines as well as current UK civilian guidelines in responding to marauding terrorist attacks50,51 (Figure 1).
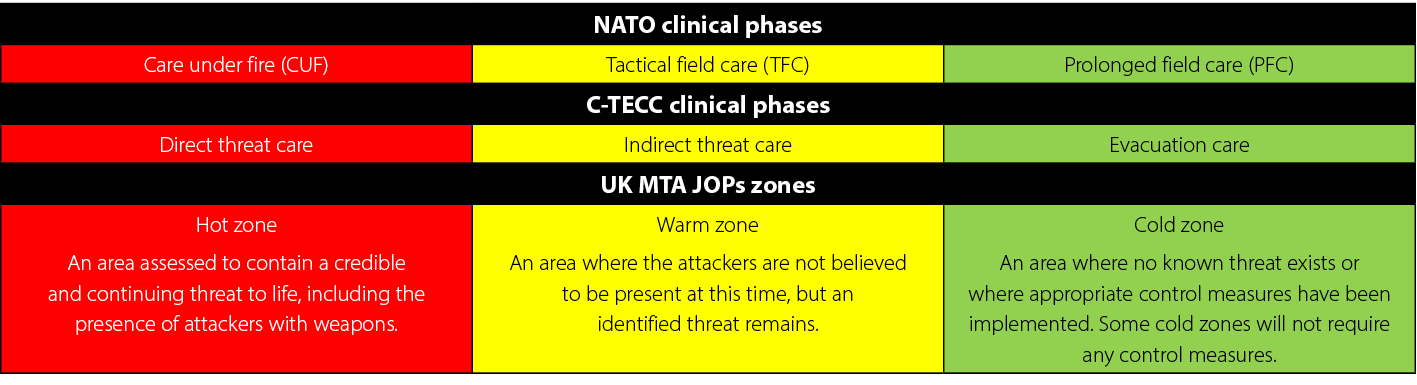
Figure 1. A comparison of three phased high threat medicine models
Much of the UK’s PO policing occurs in the state of normality or tension, with some escalating to disorder, whilst serious disorder/riot or unrest are relatively uncommon52. Whilst in tension, although there is no violence or explicit threat of violence, a trigger incident can result in a no-notice move to disorder43 which may impact on the willingness of conventional medical providers to operate in such environments even prior to disorder, with the doctrine of ‘scene safety’ being paramount for pre-hospital providers21,53,54.
Although UK disorder and rioting do not regularly involve firearms discharge, they do involve dynamic hostile crowds, criminal damage, projectiles, incendiary devices and gross interpersonal violence, all of which should initiate and justify the application of threat-based clinical care such as that outlined by the C-TECC ‘civil unrest’ working group and practised by international models49,55. Examples of tension or potential disorder can be interpreted as a clinical ‘warm zone’ where, akin to ballistic threat environments, specialist trained and equipped clinicians could operate. A state of active disorder, serious disorder/riot or unrest are environments that are definitively hostile and currently interpreted as no longer permissive for medical responders.
Pre-hospital care providers must consider that, unlike classic high threat operations – where the provision of a conventional firearm allows a police officer to project force, creating a relatively safe area of working for healthcare staff – this concept does not translate into PO scenarios. PO policing commonly involves separating opposing parties, protecting vulnerable premises, or holding a cordon to prevent further crime or harm42; this is often done in close proximity to a crowd, often at arms length. The use of pre-emptive or reactive self-defence tactics are therefore commonplace and personal security cannot be guaranteed by the presence of PO policing colleagues alone8,28,30,31. As a result, formally provisioned PO medicine in the ‘hot zone’ of UK PO is currently limited to police assets.
Public order policing
In the UK, PO policing is usually undertaken by groups of police officers organised into police support units (PSUs) of between 22 to 25 officers, usually operating in protected vehicles21. The training and levels of personal protective equipment (PPE) vary (Table 1).
Table 1. A comparison of three levels of PO trained police officers42
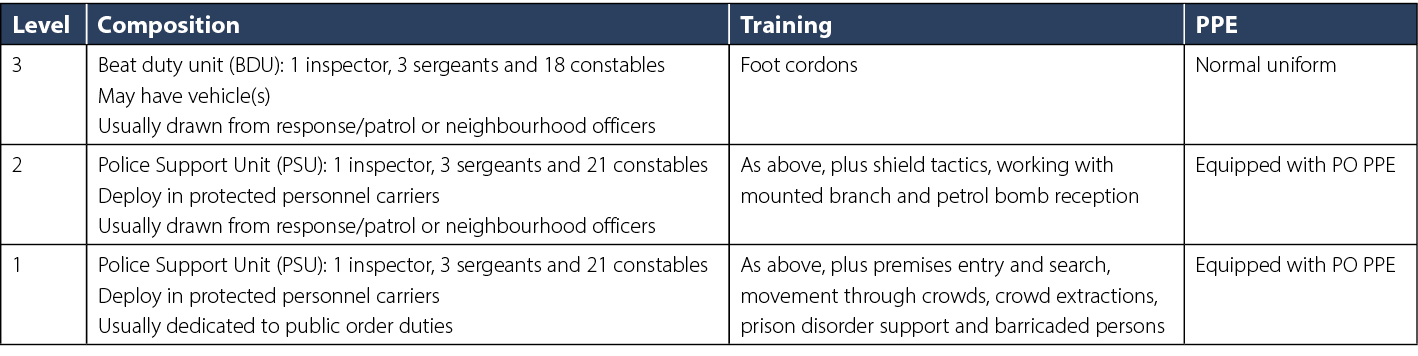
Level 1 or Level 2 officers will not automatically deploy in PPE, and when they do so they are known as ‘protected officers’. The decision to deploy in PO PPE (Figure 2) will ordinarily be made by a commander based on intelligence as to the threat they may face and the health and safety needs of the officers but will also take into consideration other factors like public perception21.

Figure 2. A police PO medic in PO PPE [image courtesy of the Metropolitan Police Service]
Officers in PO PPE are frequently utilised in the policing of other incidents that share similar themes such as undertaking rapid premise entry as part of high-risk arrest or search warrants where violence is anticipated, or dealing with other violent subjects, e.g. barricaded persons. PO PPE equipped officers may also be used when responding to unlicensed music events and, more recently, public health legislation breaches. These can be considered as ‘trigger’ events, where policing intervention may subsequently result in public disorder or where disorder is expected to occur regardless of policing intervention.
The majority of injuries to sparsely protected officers in Northern Ireland between 1969 and 1972 were to lower limbs from thrown projectiles but were relatively minor in nature9. A large proportion of any serious injuries (primarily burns and fractures) were to the face, prompting development of a helmet with facial protection, shin guards and shields9. It was deemed that PO PPE needed to be a compromise between protection and mobility; the resulting system included flame-retardant overalls, limb guards and helmets, in addition to the body armour routinely worn by officers56.
There is notable variance in international practice, and provision of specific PO PPE is not universal57,58. The UK approach appears effective in mitigating blunt injuries, whether at close quarters, with weapons, or at range with projectiles59,60,61, although a distinct paucity in evidence regarding modern operational injuries makes it difficult to assess its true effect.
Police first aid
The Metropolitan Police Service was founded in London in 1829. Although there was no specific provision of first aid, the first general instructions to the force referred to constables as “being responsible for the security of the lives of every person within his beat”62. As it was at the formation of the UK’s first public police force, policing still accepts that “protecting life” is amongst their core duties63. However, there is no general duty on the police to provide first aid, the circumstances in which they are obliged to do so are governed by legislation and policy.
The Health and Safety (First Aid) Regulations 198164, stemming from the Health & Safety at Work Act 197465, state that employers should ensure that they have provision for “adequate first aid to employees that are injured or become ill”. The Police (Health and Safety) Act 199766 specifically extended all health and safety legislation to include police officers, who as crown servants were otherwise not recognised as employees. As such, the police are obliged to provide first aid for unwell or injured officers, with no exemptions for dangerous environments such as PO. Under the same acts, the police are obliged to ensure that their work does not expose the public to risk. The policing of a riot with the use of batons and horses inevitably poses a risk of harm to the public. It is obligatory that the police minimise that risk, and part of this is through the provision of first aid in circumstances where the insult itself cannot be avoided.
The Basic principles on the use of force and firearms by law enforcement officials67 states that, where someone is subject to police use of force, the police should ensure that assistance and medical aid are rendered to any injured or affected persons at the earliest possible moment. This was further reinforced by a review of the police response to the 2011 summer disorder which generated ten key principles governing the police use of force. One of the principles includes the availability of adequate medical expertise to respond to harm caused by the use of force2.
Under the Human Rights Act 1998, every citizen has a right to life, except in very specific circumstances68. The Act created positive obligations when the State must take action in order to uphold the right, rather than simply refrain from breaching it. So, in the case of the ‘right to life’, when the State use lawful force on a citizen, in circumstances where this action may take their life, there is a duty then to attempt to save their life once the threat has passed69.
These laws and international convention have influenced police policy and procedure, and thus have been incorporated into practice through authorised professional practice (APP), the national ‘best practice’ guidance for how policing should be undertaken. Under the Operations APP, commanders must consider “the health and safety implications for officers and members of the public who may be affected by police action”70, embedding both public and police health and safety legislation. Likewise, the Operations Planning APP reflects the 1998 Act in that fact that police must “ensure that assistance and aid are rendered to any injured or affected persons at the earliest practicable opportunity”63.
Public order medics
As far back as 1975 it was identified that the availability of first aid for police officers in a riot would prevent unnecessary interactions with healthcare professionals for minor injuries, thereby retaining officers in operational settings9. Additional first aid training was given to some PO officers in both the UK and other countries with similar policing systems54. Following the inquiry into the death of Stephen Lawrence71, the then National Police Improvement Agency, now the College of Policing, introduced a national modular first aid learning programme consisting of four modules72:
- Module 1 is delivered to all police personnel.
- Module 2 is designed for police personnel who have contact with the public and meet the requirements of the Health and Safety Executive’s (HSE) Emergency First Aider at Work.
- Module 3 includes the content of Module 2 with additional inputs relevant to the custody setting.
- Module 4 was designed for officers and staff working in medium to high-risk environments and meets the requirements of the HSE’s First Aid at Work.
The importance of point of wounding care is universally recognised49,53,73; however, none of the modules included the skills necessary to deal with major trauma, to operate in environments devoid of healthcare support, nor to extricate casualties from those environments. Forces developed ad hoc solutions and the standard of training and/or equipment varied massively. It was noted that the standard of clinical care in firearms operations could be “a police medic carrying a pack of plasters, where in other forces it is people who can do chest drains”74. Officers at both ends of the spectrum called for standardisation.
The then Association of Chief Police Officers (ACPO) approached the Faculty of Pre-Hospital Care (FPHC) for assistance and a working group was convened75, the result of which was Module D13 of the National Police Firearms Training Curriculum76. Recognising that other areas of policing also required enhanced first aid skills, D13 became the basis for Module 5 of the First Aid Learning Programme73. Module 5 can be considered as a nationally-approved ‘menu’ of options from which forces, acting on clinical governance recommendations, can select the relevant clinical skills they need for a variety of high-risk policing environments, including but not limited to PO.
Whereas Module D13 is the first aid element of the National Police Firearms Curriculum, the equivalent first aid element of the PO Curriculum is Module F377. Officers operating at Module 5 trained are subject to national and local clinical governance21 with capabilities that commonly align with Level D on the FPHC78 Competency Framework (Table 2).
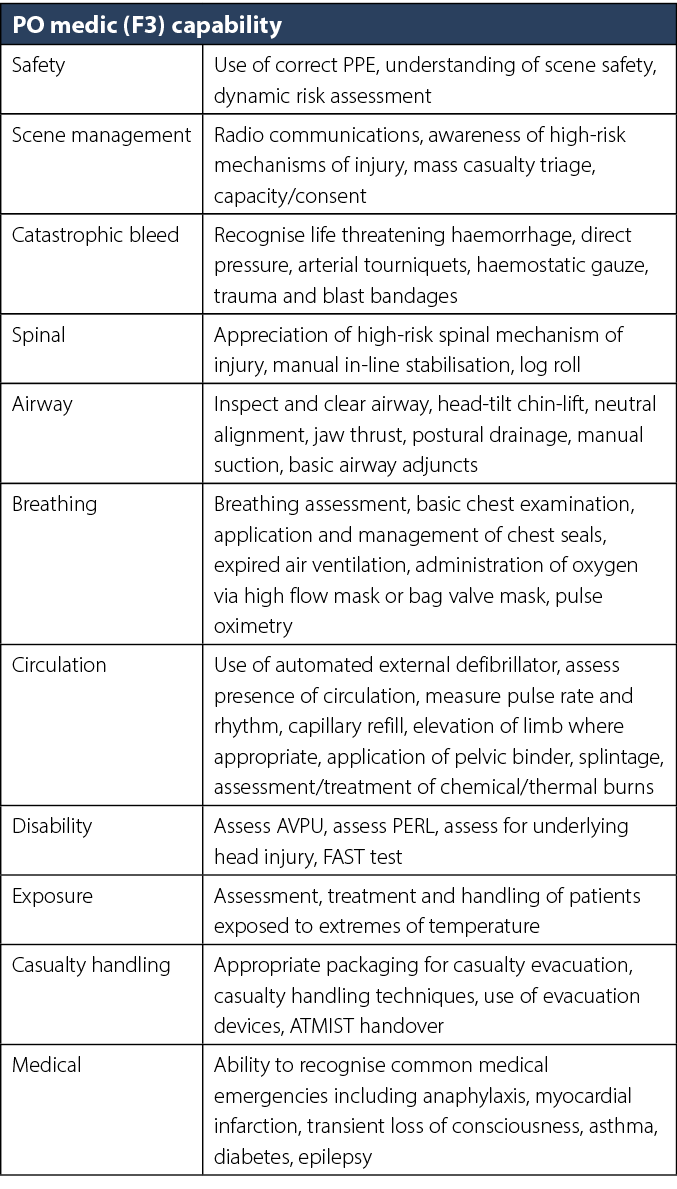
Table 2. Metropolitan Police Service PO medic (F3) capability (as of March 2023) in reference to FPHC PHEM competency framework78
F3 emphasises the need for contextualised learning76,77 but it is not prescriptive about specific tactics. Being able to adapt to unfolding events, potential threats and operate seamlessly alongside police PO tactics requires medics to be both occupationally and operationally competent PO officers before training as a medic77. This enables them to fulfil their core roles and responsibilities, including understanding strategic, tactical and operational intent and plans as well as their individual policing and clinical role within it, operating within the law and policy, environmental scanning and risk assessment, recognition and application of crowd psychology and dynamics, and being able to liaise with the operational commander in a relevant fashion to inform their planning and tactics21,42,43.
The dynamic nature of the PO environment requires a flexible response commensurate with the constantly changing environment, thereby negating the ability to follow a set process. The use of police officers already experienced in the PO environment, further enhanced by regular role specific training, intends to enable them to maintain sufficient ‘bandwidth’ to perform the clinical tasks required in the dynamic PO environment79. PO medics are routinely deployed in pairs for safety and clinical efficacy, allowing for ‘contact and cover’ casualty care as well as ensuring an evacuation capability. During serious disorder, the pairs model can be replaced by larger numbers where resources allow. PO medics are additional to officers deployed as PSUs, but they may be attached to an individual PSU for transportation or command purposes21.
The ambulance service and healthcare
A series of cases in the 1990s had held that the fire service and coast guard were not duty-bound to go to the aid of any individual in danger80,81. A similar series held that police services do not owe a duty of care to individual members of the public who suffer as a result of the criminal’s activity; instead, the police retain an ongoing duty of care to the public as a whole82,83. In contrast, an unreasonably delayed response by an ambulance service to an emergency call could be actionable negligence, creating a duty of care for individual patients for the ambulance service84. Once a patient is identified as needing ambulance care, the service has the responsibility to that individual84.
In light of this duty of care, UK National Health Service (NHS) trusts must have in place arrangements to safely respond in the event of local or national acts of public disorder, i.e. riots or demonstrations85. The UK Ambulance Services Emergency Preparedness Resilience and Response Group (EPRRG) has developed a Public Safety and Public Order Guidance to provide direction of operational and tactical options for such incidents29. At some large-scale events, medical cover can include the provision of foot mounted medical response teams (MRT) including volunteer or NHS ambulance service personnel29,86. A small number of ambulance services also have the capability of deploying foot mounted MRTs in full PO protective (MRTPO) equipment to the peripheries of disorder29. In practice, this capability is based around the concepts of creating a casualty collection point and using MRTPO staff to collect patients from police medics who have extricated them out of a PO hot zone or deploying into areas with no active disorder threat. Due to the considerable command and logistical elements required to deploy them, these teams are predominantly limited to pre-planned operations29.
Though the ambulance service teams are often registered healthcare professionals with the appropriate PPE, good medicine alone does not make for good high threat medicine87,88. The PO hot zone, a high threat environment, cannot be mitigated through the wearing of PPE alone. When considering the C-TECC guidelines49, it would be reasonable to consider ambulance service assets as PO warm zone operatives. These ambulance service teams cannot independently function or defend themselves within active disorder, i.e. within the PO hot zone. As a result, these teams should be considered as event assets with additional protection rather than true independent public disorder assets.
Cocks identified different models of pre-hospital care in civil disorder54. Examples included healthcare professionals with PO PPE and specific tactical training to integrate with police operations as well as healthcare professionals with no additional training for the environment but with some form of distinctive PO PPE54. In both cases he concludes that the opportunity for healthcare professionals to deliver meaningful interventions beyond those delivered by police medics in this environment does not outweigh the additional risk to them through transfer of malice by their proximity to both police and the threat. He concludes that the safest and most efficient use of pre-hospital care resources in civil disorder is at fixed location”casualty retrieval points”, a conclusion also made post the Hillsborough crush89 and now reflected in current national healthcare guidance29. This historic model remains unchanged and has been demonstrated at a number of modern UK incidents, both within London and in outer counties such as during the Bristol Sentencing and Courts Bill protests29,36.
Although the current police and healthcare guidance clearly recognises the unique challenges that PO brings, supporting the concept of recognising the area as an operational subspeciality of high threat medicine, questions do remain as to whether the clinical aspects of the UK model meet the needs of casualties that occur within the PO hot zone. This potential gap within care provision, commonly described as the therapeutic vacuum within high threat medicine90, is equally valid within disorder. The limited data regarding modern injury profile fails to answer whether there are patients that may benefit from alternative systems of care or skills and equipment not yet contained in Module 5. Equally, it fails to identify if there are any elements of F3 that are inappropriate for the modern PO environment.
Internationally, there are alternative models which see healthcare professionals embedded in, or deployed with, police units in disorder. The identification of separate provision for disorder recognises the sub-speciality, especially as most have been developed from existing TEMS units. Following violent election protests in 2016, the Portland Bureau of Fire & Rescue in the US created a team to work with the police’s disorder-oriented rapid response team55 building on the experience of, but distinct from, the TEMS support to the police’s special weapons and tactics unit and special emergency response team5.
In New Zealand, Wellington Free Ambulance established a TEMS team to respond active-shooter situations, with paramedics working alongside police special tactics group and armed offender squads. Public health-related protests at the parliament buildings in early 2022 saw three paramedics working with the PO policing support units, ahead of conventional ambulance units on the perimeter of the warm and cold zone. The paramedics were described as operating in the warm and hot zone with police protection13. Broad variances in the definition and presentation of disorder and the gross impact of availability of firearms within each setting make it difficult to generalise findings; however, these examples unanimously support the concept that PO presents unique challenges within high threat medicine.
Summary
In ballistic-orientated interpretations of high threat medicine, the threat is often considered as the response to incidents involving conventional firearms, bladed weapons or other means considered otherwise so dangerous. These threats are predominantly mitigated by the projection of force using police firearms, creating safe distances and/or employing exclusionary zones whilst the threat is identified, located, contained and subsequently neutralised. Within PO, threat presents itself differently and is rarely amenable to the same mitigation techniques. PO policing occurs in close quarters and commonly involves separating opposing parties, protecting vulnerable premises, or holding a cordon to prevent further crime or harm. This style of policing makes it extremely difficult to project force, create safe distance or employ large exclusionary zones. As a result, this greatly limits the area in which healthcare providers can work without adequate protection and the means to defend themselves.
There are multiple threats to the public, police and any pre-hospital care providers; this can include dynamic hostile crowds, direct interpersonal violence and projectiles including incendiary devices, corrosive and chemical substances, moving vehicles and large animals. Any state of active disorder, serious disorder/riot or unrest where these threats are active or likely are environments that should be considered as hostile, necessitating specialist training, equipment and experience. These clear operational, tactical and clinical challenges that occur within areas of violent disorder are not amenable to quintessential ballistic or explosive threat TEMS responses. The development of the C-TECC ‘civil unrest’ working group demonstrates a recognition of these challenges as part of high threat medicine as a whole, with a small number of international TEMS systems demonstrating specific disorder/riot-based capabilities.
Within the UK, however, NHS resources are generally unable to operate in environments where disorder or an uncontrollable threat of disorder exists. As a result, the primary model of care is that of police PO medics supported by NHS ambulance service resources based at casualty retrieval points. This UK model demonstrates that some form of intentional PO medicine exists; however, it presents as a tactical option within POPS policing rather than a defined area of operational high threat medical practice described internationally. In recognising PO medicine as an operational subspeciality of UK high threat medicine, we propose that there is scope to further develop our understanding of the area, identify any PO ‘therapeutic vacuum’, and improve our response to it.
Despite a reasonable understanding of historic injury patterns in UK disorder, there is very little published data regarding the modern UK PO experience, by either the police or ambulance service. Recognising the speciality in its own right will provide the opportunity to develop the clinical content within F3 and the overall role of the PO medic. Where there is limited space to carry extensive medical equipment, an improved understanding of the environment may positively influence the issue of equipment and its carriage. This same understanding may allow for better nuanced training within this environment.
Whilst the police are unable to discharge their statutory pre-hospital care obligations to a third party, it is not yet understood whether there is a role for specialist trained clinicians assisting the police in this environment, and how any benefits are weighed against the potential risk to the clinicians involved. Although national guidance exists, the requirement for ambulance services to respond to incidents in close proximity to disorder is not currently clearly defined. Data describing the current frequency and nature of such demand, and interpretation of the available intelligence to determine the potential for it, would assist ambulance services and/or enhanced care providers in considering, developing or adapting their capability and interoperability to meet their obligations in that environment.
Acknowledgements
With special thanks to the PO medics and instructors of the Metropolitan Police Service, Chief Inspector Joseph Stokoe, Inspector Jim Cole, Police Sergeant Gavin Marjolin, Police Constables Daniel Greene, Lee Lashmore, Damien Davies, Daniel Champion, Victoria Harriott, Phil Hollister, Chris Eales and James Duthoit, and the extended team at the Metropolitan Police Specialist Training Centre, Gravesend, Kent, UK.
ORCID numbers
Sean Brayford-Harris 0000-0001-9054-1342
Nicolas Mattock 0000-0001-8659-3756
Andrew Barrett 0000-0002-7060-2694
Claire Park 0000-0003-0175-4480
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Sean Brayford-Harris*1, Nicolas Mattock2, Andrew Barrett3, Claire Park4,5
1Interoperability Development Officer (Metropolitan Police Service) & Tactical Response Paramedic, London Ambulance Service, UK
2Operational Police Officer, UK
3Police Sergeant & Public Order Medic, Metropolitan Police Service, UK
4Pre-Hospital Care Consultant, Institute of Pre-Hospital Care at London’s Air Ambulance & Barts Health NHS Trust, UK
5Medical Advisor to Specialist Firearms Command, Metropolitan Police Service, UK
*Corresponding author email sean.harris4@nhs.net
References
- McKittrick D, McVea D. Making sense of the troubles: the story of the conflict in Northern Ireland. New Amsterdam Books; 2002.
- His Majesty’s Inspectorate of Constabulary and Fire & Rescue Services (HMICFRS). The rules of engagement: a review of the August 2011 disorders. 2011. Available from: https://www.justiceinspectorates.gov.uk///hmicfrs/media/a-review-of-the-august-2011-disorders-20111220.pdf
- Reicher S, Stott C. On order and disorder during the COVID-19 pandemic. Br J Soc Psychol 2020;59(3):694–702.
- Callaway DW, Smith ER, Cain J, Shapiro G, Burnett WT, McKay SD, et al. Tactical emergency casualty care (TECC): guidelines for the provision of prehospital trauma care in high threat environments. J Spec Oper Med 2011;11(3):104–22.
- West M. Portland’s rapid response team, a novel approach to TEMS in civil disturbance. Tactical and Law Enforcement Medicine Newsroom: American College of Emergency Physicians; 2021.
- McPhail C, Wohlstein RT. Individual and collective behaviors within gatherings, demonstrations, and riots. Ann Rev Sociol 1983;9(1):579–600.
- El Zahran T, Mostafa H, Hamade H, Mneimneh Z, Kazzi Z, El Sayed MJ. Riot-related injuries managed at a hospital in Beirut, Lebanon. Am J Emerg Med 2021;42:55–9.
- Devlin K. Northern Ireland riots: 88 police officers injured in ‘unacceptable’ violence. The Independent; 2021 Apr 13. Available from: https://www.independent.co.uk/news/uk/politics/northern-ireland-riots-violence-police-b1830661.html
- James W. Riot injuries to policemen: an analysis of 808 policemen injured in rioting between 1969 and 1972 in Northern Ireland. Injury 1975;7(1):41–3.
- Unuvar U, Yilmaz D, Ozyildirim I, Dokudan EY, Korkmaz C, Doğanoğlu S, et al. Usage of riot control agents and other methods resulting in physical and psychological injuries sustained during civil unrest in Turkey in 2013. J Forensic Legal Med 2017;45:47–52.
- Zekri A, King W, Yeung R, Taylor W. Acute mass burns caused by o-chlorobenzylidene malononitrile (CS) tear gas. Burns 1995;21(8):586–9.
- Schep LJ, Slaughter RJ, McBride DI. Riot control agents: the tear gases CN, CS and OC – a medical review. BMJ Mil Health 2015;161(2):94–9.
- New Zealand Police Association. Men in green; 2022. Available from: https://www.policeassn.org.nz/news/men-in-green#/.
- Mahajna A, Aboud N, Harbaji I, Agbaria A, Lankovsky Z, Michaelson M, et al. Blunt and penetrating injuries caused by rubber bullets during the Israeli–Arab conflict in October, 2000: a retrospective study. Lancet 2002;359(9320):1795–800.
- Millar R, Rutherford W, Johnston S, Malhotra V. Injuries caused by rubber bullets: a report on 90 patients. J Br Surg 1975;62(6):480–6.
- Azad TA, Hasan I, Ahmmed R, Saha MK, Moni SJ, Chowdhury S. Anthropogenic disaster: petrol bomb explosion consequences analysis in Bangladesh. Am J Renew Sustain Energy 2018;4(4):64–76.
- Kolaitis DI, ed. An experimental investigation of improvised incendiary devices used in urban riots: the ‘Molotov cocktail’. Proceedings of the 2nd IAFSS European Symposium of Fire Safety Science, Nicosia, Cyprus; 2015.
- Giacomantonio C, Bradford B, Davies M, Martin R. Making and breaking barriers assessing the value of mounted police units in the UK: summary report. Rand Europe; 2014. Available from: https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR830z1/RAND_RR830z1.pdf
- Orr R, Canetti EF, Pope R, Lockie RG, Dawes JJ, Schram B. Characterization of injuries suffered by mounted and non-mounted police officers. Int J Environ Res Public Health 2023;20(2):1144.
- McNab C. Riot control vehicles: 1945–present: Bloomsbury Publishing; 2015.
- College of Policing. Tactical options; 2018. Available from: https://www.app.college.police.uk/app-content/public-order/planning-and-deployment/tactical-options.
- Barr R, Mollan R. The orthopaedic consequences of civil disturbance in Northern Ireland. J Bone Joint Surgery Br Vol 1989;71(5):739–44.
- Police Service of Northern Ireland (PSNI). A history of policing in Ireland; 2021. Available from: https://www.psni.police.uk/inside-psni/our-history/a-history-of-policing-in-ireland
- Chrisafis A. Riots rain on Belfast’s parade. The Guardian. 2005 Sep 12. Available from: https://www.theguardian.com/uk/2005/sep/12/northernireland.angeliquechrisafis
- McDonald H. Belfast loyalists attack police as riots over union flag dispute continue. The Guardian. 2013 Jan 6. Available from: https://www.theguardian.com/uk/2013/jan/06/belfast-loyalists-attack-police-flag
- Weatheritt M. Talking blues: the police in their own words. HeinOnline; 1990.
- Field S, Southgate P. Public disorder: a review of research and a study in one inner city area: HM Stationery Office; 1982.
- Hall R. PC Blakelock killing: What happened on night of riots? BBC News. 2014 Apr 9. Available from: https://www.bbc.co.uk/news/av/uk-26961881.
- United Kingdom Ambulance Services Emergency Preparedness Resilience and Response Group. UK NHS Ambulance Service Public Safety & Public Order Guidance. United Kingdom Ambulance Services Emergency Preparedness Resilience and Response Group; 2019.
- The Guardian. UK riots aftermath – Friday 12 August 2011. The Guardian. 2011 Aug 11. Available from: https://www.theguardian.com/uk/blog/2011/aug/12/uk-riots-day-six-aftermath.
- BBC. England riots – maps and timelines. BBC. 2011 Aug 15. Available from: https://www.bbc.co.uk/news/uk-14436499.
- Milmo C. The night that rioters ruled and police lost control of the streets of London. The Independent. 2011 Aug 10. Available from: https://www.independent.co.uk/news/uk/crime/the-night-that-rioters-ruled-and-police-lost-control-of-the-streets-of-london-2335067.html
- BBC. George Floyd: London anti-racism protests leave 27 officers hurt. BBC. 2020 Jun 7. Available from: https://www.bbc.co.uk/news/uk-england-london-52954899.
- Metropolitan Police Service. Injuries to police officers at the Black Lives Matter protests in London in June 2020. 2020. Available from: https://www.met.police.uk/foi-ai/metropolitan-police/disclosure-2020/july/injuries-police-officers-black-lives-matter-protests-june2020/
- Cork T. Full list of all the 46 police injuries in the ‘Kill The Bill’ Bristol protests. Bristol Post. 2021 Apr 21. Available from: https://www.bristolpost.co.uk/news/bristol-news/full-list-46-police-injuries-5325518
- Avon and Somerset Police. Kill the Bill protests (Op Hyacinth/Op Harley) – person specific injury/illness reports; 2021. Available from: https://media.aspolice.net/uploads/production/20221019123021/Op-Harley-Redacted-Injury-on-Duty-forms.pdf
- Glover E. Anti-lockdown protests turn violent as police officers sustain ‘minor’ injuries. The Independent. 2021 Dec 18. Available from: https://www.independent.co.uk/news/uk/home-news/antilockdown-protest-london-police-b1978716.html
- Home Office. Football-related arrests and banning orders, England and Wales: 2021 to 2022 season; 2022. Available from: https://www.gov.uk/government/statistics/football-related-arrests-and-banning-orders-england-and-wales-2021-to-2022-season
- The Football Association. Statement following UEFA’s sanctions over Euro 2020 final [press release]. The Football Association 2021 Oct 18. Available from: https://www.thefa.com/news/2021/oct/18/fa-statement-uefa-20211810
- The Open University and Metropolitan Police Authority. International Centre for the History of Crime, Policing and Justice: Police and public order online; 2009. Available from: http://www.open.ac.uk/Arts/history-from-police-archives/Met6Kt/PublicOrder/poIntro.html.
- HM Government. Public Order Act 1986, United Kingdom. Available from: https://www.legislation.gov.uk/ukpga/1986/64
- College of Policing. Public order; 2018. Available from: https://www.app.college.police.uk/app-content/public-order/.
- College of Policing. Disorder model; 2018. Available from: https://www.app.college.police.uk/app-content/public-order/planning-and-deployment/#disorder-model.
- Events Industry Forum. The purple guide - 5. Medical; 2014. Available from: https://www.thepurpleguide.co.uk/index.php/the-purple-guide/101-5-medical.
- Metropolitan Police Service. Detectives renew appeal for photos and video of Brixton Academy crush [press release]; 2022 Dec 30. Available from: https://news.met.police.uk/news/detectives-renew-appeal-for-photos-and-video-of-brixton-academy-crush-459729
- Sky News. Four people in critical condition after fans break into Asake concert in Brixton. Sky News 2022 Dec 16. Available from: https://news.sky.com/story/four-people-in-critical-condition-after-crowd-trouble-at-asake-concert-in-brixton-12769065.
- Butler Jr FK, Hagmann J, Butler EG. Tactical combat casualty care in special operations. Mil Med 1996;161(suppl_1):3–16.
- US Department of Defence. Joint trauma system tactical combat casualty care (TCCC) guidelines 5 November 2020. 2020. Available from: https://www.deployedmedicine.com/content/40
- Committee for Tactical Emergency Casualty Care (C-TECC). TECC guidelines – June 2015. Available from: https://www.c-tecc.org/images/content/TECC_Guidelines_-_JUNE_2015_update.pdf.
- Sharpe D, McKinlay J, Jefferys S, Wright C. Military prehospital emergency care: defining and professionalising the levels of care provided along the operational patient care pathway. BMJ Mil Health 2019;165(3):188–92.
- Joint Emergency Services Interoperability Principles (JESIP). Responding to a marauding terrorist attack: joint operating principles for the emergency services, edition 2, December 2020. 2020.
- Waddington D, King M. Identifying common causes of UK and French riots occurring since the 1980s. Howard J Crim Justice 2009;48(3):245–56.
- Joint Royal Colleges Ambulance Liaison Committee and Association of Ambulance Chief Executives (JRCALC & AACE). JRCALC PLUS: JRCALC clinical practice guidelines 2023 – Version 2.1(2). Mobile App: Class Publishing; 2022.
- Cocks RA. Medical care in civil disorder. Trauma 1999;1(3):255–63.
- Pennardt A, West M. Riot medicine: civil disturbance applications of the national tactical emergency medical support competency domains. J Spec Op Med 2020;20(4):73–6.
- College of Policing. National police public order training curriculum – guidance for forces. Module G3 – public order standards, training, equipment and resources. 2018.
- Zygoura A, Fragkos D, Giannouleas P, Sotiriou A, Pyrros DG. Emergency medical services response to the Athens riots in December 2008. Prehosp Disaster Med 2009;24(S1):s43.
- Kapil N, Parmar M, Saini S. Study to analyze and improve anti riot body protector. Man-Made Textile India 2021;49(1).
- Malbon C. PSDB protective headwear standard for UK Police (2004) – public order helmet. Home Office; 2004. Available from: https://ped-cast.homeoffice.gov.uk/standards/21-04_PROTECTIVE_HEADWEAR_STANDARD_FOR%20POLICE_LOW_RES.pdf
- Malbon C. HOSDB blunt trauma protector standard for UK Police (2007). Home Office; 2007. Available from: https://ped-cast.homeoffice.gov.uk/standards/20-07_HOSDB_Blunt_Trauma_Protector_Standard_(2007)_Limb_Torso.pdf
- Malbon C. HOSDB flame retardant overalls standard for UK Police (2008). Home Office; 2008. Available from: https://ped-cast.homeoffice.gov.uk/standards//89_08_flame_retardant_overalls.pdf
- Morning Chronicle. New police instructions. 1829 Sep 24. Available from: www.britishnewspaperarchive.co.uk
- College of Policing. Core principles; 2018. Available from: https://www.app.college.police.uk/app-content/operations/operational-planning/core-principles/.
- Health and Safety Executive. The health and safety (first-aid) regulations 1981. Guidance on regulation. 2013. Available from: https://www.hse.gov.uk/pubns/priced/l74.pdf
- Health and Safety Executive. Health and Safety at Work etc. Act 1974. Available from: https://www.hse.gov.uk/legislation/hswa.htm
- HM Government. Police (Health and Safety) Act 1997. Available from: https://www.legislation.gov.uk/ukpga/1997/42/contents
- Office of the High Commissioner for Human Rights. Basic principles on the use of force and firearms by law enforcement officials, 1990. Available from: https://www.ohchr.org/en/instruments-mechanisms/instruments/basic-principles-use-force-and-firearms-law-enforcement
- HM Government. Human Rights Act 1998. Available from: https://www.legislation.gov.uk/ukpga/1998/42/contents
- Osman v. The United Kingdom (Application no. 87/1997/871/1083). European Court of Human Rights. Available from: https://hudoc.echr.coe.int/fre#%7B%22itemid%22:[%22001-58257%22]%7D
- College of Policing. Deployment planning; 2018. Available from: https://www.app.college.police.uk/app-content/operations/operational-planning/deployment-planning/.
- Macpherson W. The Stephen Lawrence inquiry: report of an inquiry by Sir William Macpherson of Cluny. London; 1999. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/277111/4262.pdf
- College of Policing. First aid learning programme specification version 2.2; 2016.
- Park CL, Grier GR. Provision of pre-hospital medical care for terrorist attacks. Elsevier; 2021.
- Police Review. Policing paramedics. Police Rev 1997:18–21.
- Hartley F, Howells A, Thurgood A, Hall F, Porter K. Medical training for police officers in specialist role (D13): a retrospective review of patient report forms from 2010–2015. Trauma 2018;20(1):20–4.
- College of Policing. Module D13 – provides first aid in armed operations, national police firearms training curriculum; 2017.
- College of Policing. Module F3 – public order medic, national police public order training curriculum. College of Policing; 2016.
- Faculty of Prehospital Care, Royal College of Surgeons, Edinburgh. PHEM competency descriptors and skills framework; 2017. Available from: https://fphc.rcsed.ac.uk/media/2911/phem-competency-descriptors-and-framework.pdf.
- Rutherford G. Human factors in paramedic practice. Class Professional Publishing; 2022.
- Capital and Counties Plc v. Hampshire County Council. 1997. Q.B. 1004. United Kingdom.
- OLL Ltd v. Secretary of State for Transport (1997) 3 All E.R. 897. United Kingdom.
- Hill v. Chief Constable of West Yorkshire. (1989) AC 53. United Kingdom.
- Alexandrou v. Oxford (1993) 4 All E.R. 328. United Kingdom.
- Williams K. Litigation against English NHS ambulance services and the rule in Kent v. Griffiths. Med Law Rev 2007;15(2):153–75.
- National Ambulance Resilience Unit (NARU). Service specification for UK ambulance services – emergency preparedness resilience & response; 2012. Available from: http://naru.org.uk/wp-content/uploads/2013/02/Nov-2012-EPRR-Service-Spec.pdf
- St John Ambulance. Event first aid cover; 2021. Available from: https://www.sja.org.uk/what-we-do/our-first-aid-services/event-first-aid-cover/.
- Goodloe J. Tactical training proves beneficial for EMS. J Emerg Med Serv 2012. Available from: https://www.jems.com/operations/tactical-training-proves-beneficial-ems/
- Ciccone TJ, Anderson PD, Gann CA, Riley JM, Maxwell M, Hopkins R, et al. Successful development and implementation of a tactical emergency medical technician training program for United States federal agents. Prehosp Disaster Med 2005;20(1):36–9.
- Walsh M. Taylor on Hillsborough: what can we learn. Disaster 1989;13(3):274–7.
- Park CL, Langlois M, Smith ER, Pepper M, Christian MD, Davies GE, et al. How to stop the dying, as well as the killing, in a terrorist attack. BMJ 2020;368.