Volume 5 Issue 2
Retraining of home parenteral nutrition (HPN) users in Australia and New Zealand: a consumer audit
Karen Winterbourn, Chris Walker, Miranda Einstein, Gillian Anderson and Fay Boyd
Keywords Home parenteral nutrition, HPN, HPN training, Parenteral Nutrition Down Under Inc, PNDU
For referencing Winterbourn K et al. Retraining of home parenteral nutrition (HPN) users in Australia and New Zealand: a consumer audit. Vascular Access 2019; 5(2):29-37.
DOI https://doi.org/10.33235/va.5.2.29-37
Abstract
Introduction Published guidelines recommend patients and carers are trained and meet competency in certain criteria of connecting and disconnecting procedures before discharge from hospital on home parenteral nutrition (HPN). Despite many HPN users requiring HPN indefinitely, Parenteral Nutrition Down Under Inc. (PNDU), the consumer support and advocacy organisation for HPN users and carers in Australia and New Zealand, was not aware of any retraining of HPN users unless the user had recurring central line-associated bloodstream infection (CLABSI).
Objectives To survey PNDU members on their experiences of formal retraining in HPN procedures, and to assess how members perform one aspect of these procedures – withdraw back (into syringe) – for comparison with the latest recommended protocols.
Methods An anonymous online questionnaire was circulated in November 2018 to all PNDU HPN users and carers in Australia and New Zealand, with an invitation to all active adult HPN users – or carers of active child/adult HPN users – to participate. Following screening and demographic questions, the survey had two parts. First, questions regarding the form of any initial training before hospital discharge, followed by questions regarding any experiences in formal retraining in HPN procedures, including extent, frequency and reason. Second, questions regarding one step of the connecting procedures – withdraw back (into syringe) – sought to identify responders’ specific protocols, and determine if this was taught during the initial HPN training.
Results There were 40 responders, representing 30 adult and 10 child HPN users. This represented 56.3% of active HPN users in PNDU, and 14.2% of the estimated 282 HPN users in Australia and New Zealand. A total of 32 (80.0%) responders had been on HPN for two or more years, receiving initial training before discharge. Just over half (57.9%) had received retraining, with most (81.0%) retraining prompted by a specific event, commonly related to a suspected or confirmed CLABSI, or change of medical equipment/item used to perform the procedure. Overall, 34 (85.0%) responders withdrew back into the syringe before connecting to parenteral nutrition (PN), 25 (73.5%) discarded the aspirate, and nine (26.5%) pushed the fluid back into the central line.
Conclusions Few HPN users receive regular retraining as part of HPN management. Beyond the written instructions given with initial HPN training, we recommend regular retraining and updating in protocols be included in HPN care to realise complication prevention benefits such as maintaining quality of life and reducing healthcare costs. Additionally, in view of technique variations, more research is needed to determine best practice for withdrawal of blood and, if required, how much drawback is sufficient and safe. These results should be included in HPN procedure guidelines.
INTRODUCTION
Home parenteral nutrition (HPN) is required when there is ongoing insufficient nutrient intake through the digestive system – intestinal failure (IF)1. Intestinal failure can be caused by a wide range of digestive conditions, congenital problems and surgical complications2. Although a life-saving therapy conducted at home, HPN is complex, with serious risks and possible complications3,4, including parenteral nutrition (PN)-associated liver disease5, thrombosis6, central line-associated bloodstream infection (CLABSI)7–10, and loss of central venous access2. Home parenteral nutrition (HPN) CLABSI incidence has been recorded between 0.38–6.8 episodes per 1000-line days9,11,12. Indeed, it is the need for central venous access and care for HPN that results in the majority of complications and hospitalisations13,14. And while there are increasing research and knowledge in the use of central venous access devices (CVADs) for PN15 and encouraging studies and developments in line lock therapies16–19, aseptic protocol and good CVAD care continue to be the best weapon against CLABSI4.
Home parenteral nutrition for IF is also rare. In the absence of a register of HPN users in Australia, data requested from the three commercial suppliers of HPN solutions in Australia and New Zealand (personal communication, February 201920) gave the approximate total of 282 adult and paediatric HPN users for IF in Australia and New Zealand, a prevalence of 9.4 per million inhabitants. This compares to a prevalence of HPN for chronic IF in Europe of an estimated 5–20 per million inhabitants2, and HPN prevalence in the United States of America of an estimated 79 per million inhabitants21.
Not only can prevention and avoidance of complications reduce hospitalisations – and, with them, additional costs10 – it can also lessen the impact on the health and quality of life of the HPN user and his/her carer(s) and loved ones. For HPN users and carers without formal medical training, Home parenteral nutrition procedures can be very unfamiliar, and performing them at home without a healthcare professional present to assist can be daunting22. Home parenteral nutrition procedures involve a number of steps, including hand washing, preparing a PN bag for infusion, handling the CVAD using aseptic technique, cleaning the needleless connector, withdrawing back into the syringe, using an ambulatory infusion pump, flushing the CVAD, changing a needleless connector, preparing the skin for the new dressing and, possibly, inserting and removing implantable port needles. To perform aseptic protocol and good – often daily – CVAD care at home, most HPN users and carers will therefore need to undergo some level of training before discharge from hospital2,23.
In 2008, the Australasian Society for Parenteral and Enteral Nutrition (AuSPEN) published a guideline for the clinical practice for HPN patients in Australia and New Zealand23. In that guideline, it could not make a recommendation based on published evidence on how patients should be trained for HPN. However, by consensus, it recommended patients should be trained to meet competency in certain criteria such as the principles of asepsis. Similarly, the European Society for Clinical Nutrition and Metabolism’s (ESPEN) 2016 guidelines2, while strongly recommending specific elements to patient training for HPN, advises the evidence was very low.
The rarity of IF necessitating HPN has meant a shortage in good quality evidence, including from randomised controlled trials, for many recommendations relating to HPN CVAD care, and a reliance on observational cohort studies and expert opinion24. Furthermore, there is no mention of retraining in AuSPEN’s guideline despite some HPN users requiring this therapy indefinitely2,3. By extension, there is also no mention of training HPN users in new or updated evidence-based or best practice protocols. Similarly, the ESPEN guidelines2 only recommend re-education of the HPN patient if repeated CLABSI occur.
Our organisation, Parenteral Nutrition Down Under Inc. (PNDU), is the consumer-run support and advocacy organisation for HPN users (for IF) and carers in Australia and New Zealand. PNDU aims to support, research and inform consumers, carers and providers of PN for intestinal failure through provision of: resources and information; an annual awareness campaign; opportunities for HPN users and carers to connect with others living with HPN; representation on projects, in committees, at clinical conferences; and through conducting member surveys on matters of importance to HPN users and carers.
| PNDU membership is open internationally to any adult (over 18 years) with an interest in HPN. Members enrol through a sign-up form on PNDU’s website. |
In November 2018 PNDU membership totalled 129 adults. Of these, 104 were Category 1 HPN users/carers (active or past HPN users/carers of child or adult HPN users in Australia and New Zealand). These 104 Category 1 members represented approximately 71 active HPN users comprised of 49 active adult HPN users or their carers, and carers of 22 active paediatric HPN users. The 71 active HPN users/carers resided in every state of Australia, and in both the north and south islands of New Zealand.
While aseptic protocol and good CVAD care are important preventives of CLABSI4, PNDU suspected that little or no retraining or updating of HPN users takes place except if there is recurring CLABSI. This is in contrast to the hospital environment where clinicians accredited to care for CVADs – and with inherently more medical training and experience than an average HPN user – are provided in-service training whenever a change in policy or best practice occurs, and possibly also undergo semi-regular reaccreditation in CVAD care.
A Google Scholar search did not locate any articles or studies investigating the extent or value of retraining HPN users in CVAD care. However, two published studies on other patient cohorts have shown benefits of patient retraining in medical procedures performed at home25,26. In addition, two studies of HPN users27,28, while not primarily focused on retraining, do make relevant secondary conclusions. These four studies are considered in the Discussion.
OBJECTIVES
The aim of this survey was to identify and understand the individual experiences of PNDU active HPN users/carers of formal retraining in connecting and disconnecting to PN in the home environment.
The survey further sought to collect data on one aspect of the PN connection process, the drawing back into the syringe from the CVAD before connecting to PN. We wished to see if this step was performed in accordance with the current expert opinion of the Alliance for Vascular Access Teaching and Research (AVATAR) (personal communication, 2018), and whether there was any correlation between years of HPN use, retraining or lack thereof, and the use – or not – of the latest recommended protocols for this one step of the PN connection process.
METHOD
An invitation email to participate in the survey was sent directly to all 104 Category 1 members of PNDU. The invitation email stated only one representative for each active HPN user represented in PNDU’s Category 1 membership should complete the survey. The survey took place over 2 weeks in November 2018 and involved completing an online questionnaire compiled by PNDU’s Management Committee using a SurveyMonkey program. The survey introduction stated the survey was anonymous and outlined eligibility, objectives, rationale, parameters, how results would be used, definitions, and approximate time to complete. Home parenteral nutrition carer respondents were instructed to answer the questions on behalf of the HPN user under their care (adult or child).
The survey consisted of 19 questions and took approximately 5–10 minutes to complete (see Appendix A for the survey questions). Retraining was defined as follows:
At some point in time after initial training the responder was:
- Given additional detailed oral instructions on all or a particular technique in connecting/disconnecting to PN; and/or
- Given additional written instructions on all or a particular technique in connecting/disconnecting to PN; and/or
- Given an additional demonstration on all or a particular technique in connecting/disconnecting to PN; and/or
- Required to again demonstrate competence in performing all or a particular technique in connecting/disconnecting to PN.
Connecting techniques referred to preparation of the CVAD for connection to the bag of PN. Disconnecting techniques referred to the procedure done after stopping the infusion pump to just before administering the CVAD lock, if a lock was used. Responders were instructed not to include procedures relating to preparing a PN bag or using an infusion pump.
The survey began with a screening question to exclude any Category 1 PNDU members who were not active HPN users – nor caring for an active HPN user – and continued in two parts. The first part was a descriptive cross-sectional survey beginning with three demographic questions – the HPN user’s age, year of starting HPN, and their length of time on HPN. Questions followed regarding initial training in HPN procedures, and experiences in formal retraining in HPN procedures, including the extent, frequency and reason for retraining. The second part was an analytic, observational case control study looking at one specific component of the connecting procedure – drawing back into the syringe from the CVAD before connecting to PN. The questions sought to identify the specific protocol used by responders and if the same protocol was taught during initial HPN training. The results were compared with latest expert opinion, and were to be analysed for any link between years of HPN use, retraining or lack thereof, and use – or not – of latest recommended protocol.
For analysis purposes, HPN users younger than 18 years – represented in the survey by their carer – were classified as children. The survey was voluntary, anonymous, and no children were surveyed. No identifiable details were collected, including no demographic data regarding gender or state/country of residence. This eliminated potential identification by geography of the small number of HPN users in Australia and New Zealand. Consent was implied by survey completion.
Potential resulting benefits to responders of completing the survey were a review of current practices regarding regular formal retraining of HPN users, identification of protocol variations, and consensus of best practice for HPN procedures. The potential risk of identification was negligible due to the omission of identifying demographic questions, including geography and gender.
As a volunteer, HPN-user/carer-run, non-profit organisation existing for the benefit of HPN users and carers in Australia and New Zealand, there was no conflict of interest for PNDU to conduct this consumer audit survey. Consequently, ethics approval was not sought.
RESULTS
Responders
Forty responses were received, equating to a 56% response rate of the approximate 71 active HPN users represented in PNDU’s Category 1 membership. The 40 responses represented 30 (75.0%) adult and 10 (25.0%) child HPN users. The length of time on HPN ranged from less than two years (8 (20%); seven adults, one child) up to more than 20 years.
Initial training
The earliest initial training for HPN for any survey participants took place in 1992 (one adult) and the most recent initial training took place in 2018 (one adult). Overall, 26 (65.0%) of the 40 responders had initial training prior to 2016 and 14 (35.0%) were prior to 2011.
Thirty (75.0%) rresponders (representing 24 adult, six child HPN users) were given written instructions during initial training. Of the 10 who did not receive written material, seven had initial training prior to 2016 (Figure 1).
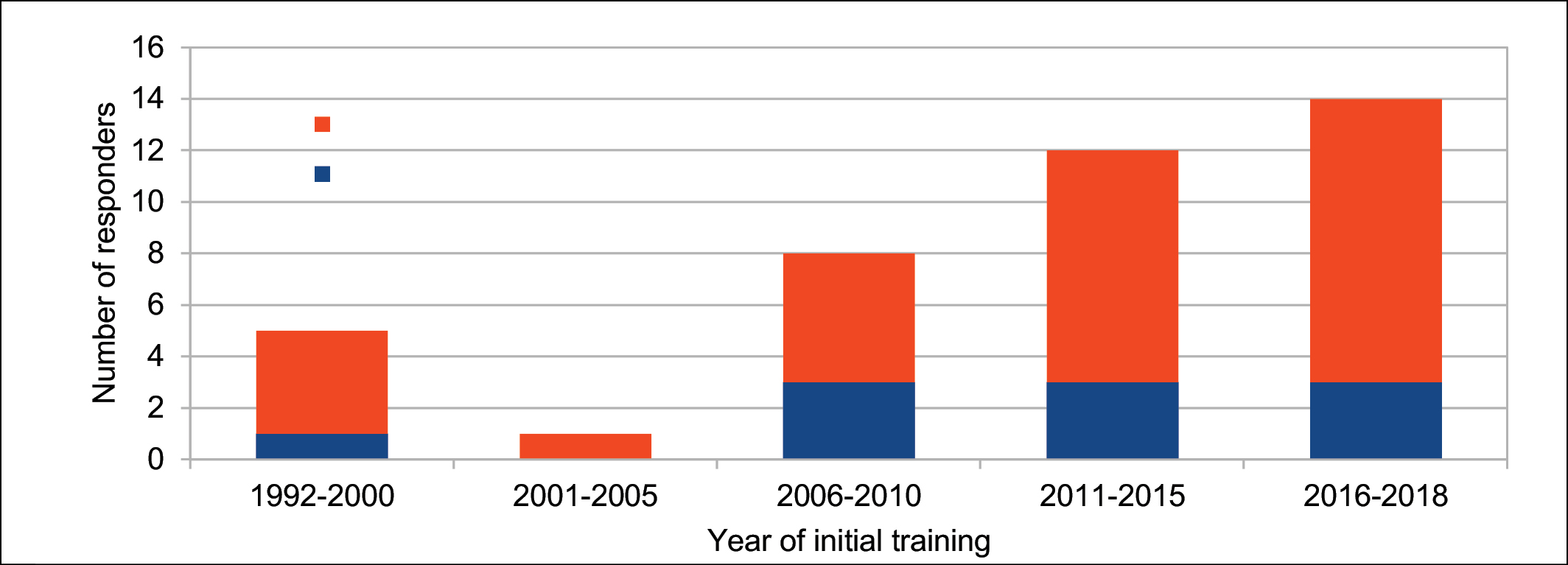
Figure 1. Year of initial training versus whether written material was given during that training.
Retraining
It was unclear whether two responders had been retrained in HPN procedures since hospital discharge. Of the remaining 38 responders, 16 (42.1%), including 12 adults and four carers of children, did not receive any retraining. Further, of these 16 responders, nine (56.3%) had received initial training during 2015 or earlier, including six receiving initial training prior to 2011 (Figure 2).
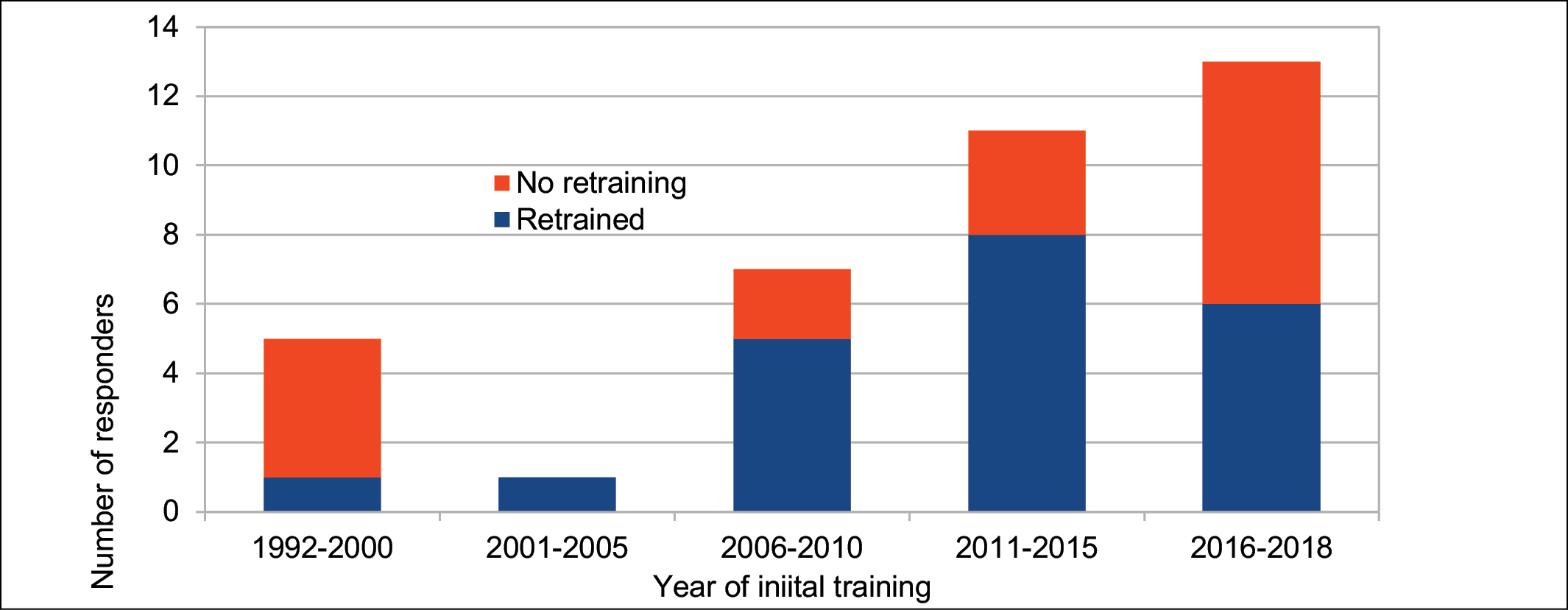
Figure 2. Year of initial training versus retraining.
Of those 22 responders who reported receiving retraining, 16 (72.7%) had received retraining once or twice, two (9.1%) regularly every year, three (13.6%) regularly every 2 years, and one responder could not remember how many times retraining had occurred. For those 16 reporting further training only once or twice, two were retrained the same year as their initial training. For the others, retraining occurred 1–13 years post-initial training.
Of the 21 responders who could remember the type of their retraining, eight (38.1%) reported being given retraining in more than one format. Overall, 11 (52.4%) reported being given additional detailed oral instructions, six (28.6%) additional written instructions, nine (42.9%) an additional demonstration, and nine (42.9%) were required to again demonstrate competence in performing a particular technique.
Eleven of the 21 responders (52.4%) reported that their retraining involved being taught new or updated procedures in connecting/disconnecting and CVAD care rather than a repeat of the initial training content. The new or updated procedures related to cleaning of the needleless connector, flushing the CVAD, using an antibacterial locking agent, and changing the CVAD used.
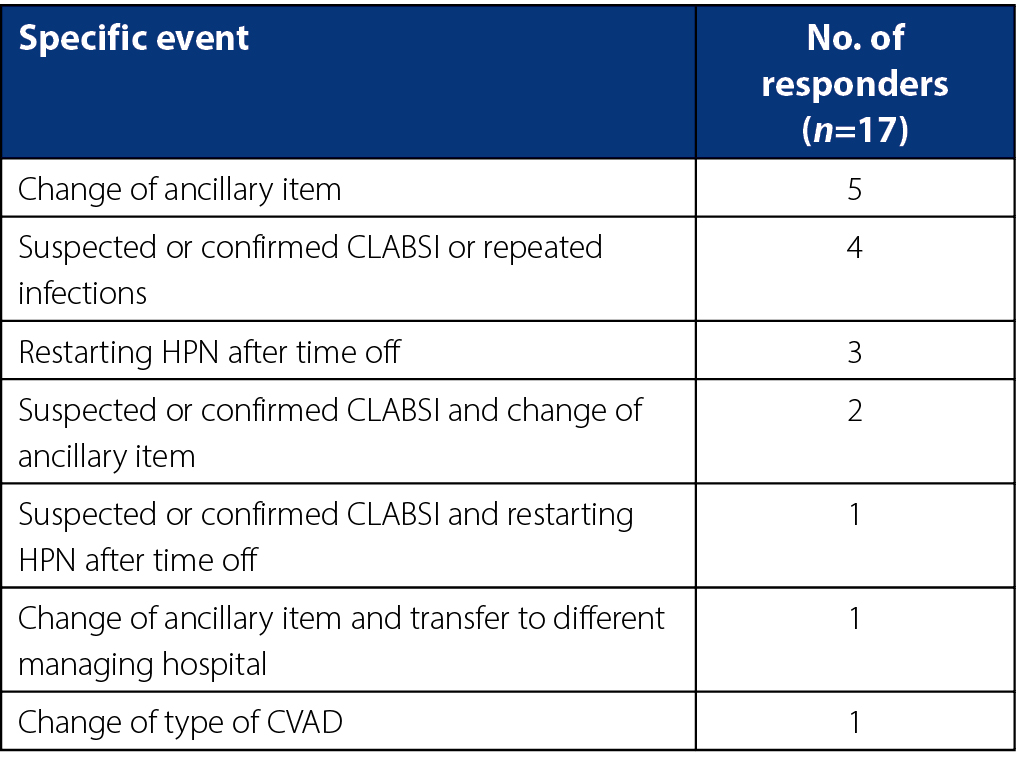
Specific events prompted retraining for 17 (81.0%) of the 21 responders. This occurred to three responders on more than one occasion. The most common events were a suspected or confirmed CLABSI (seven responders, 41.2%) or a change in use of medical equipment or item, apart from the PN and infusion pump, used to perform the connecting procedure (ancillary item), for example locking agent, pre-filled syringes, gloves, giving set (eight responders, 44.4%) (Table 1).
Table 1. Specific events prompting retraining.
Withdrawing back into the syringe before connecting to PN
Overall, 34 (85.0%) of the 40 responders reported withdrawing back into the syringe before connecting to PN. This included 24 of the 30 adults and all 10 child HPN users. Ten (eight adults and two children) of the 34 withdrew only until the first sight of blood in the CVAD/connector, with nine of these pushing the fluid back into the CVAD. Responders were not asked what sort of CVAD they used and it is noted that, unlike implantable ports and PICCs, Hickman® and Broviac® CVADS are opaque. This results in not seeing blood on drawback until blood enters either the needleless connector or syringe.
A total of 24 (70.6%) responders withdrew the line lock or a quantity of blood. These 24 all discarded the fluid withdrawn (Figure 3). Thirty (76.9%) of 39 responders currently used the same drawback procedure – or no drawback – as taught before initial discharge from hospital on PN. This included four who did not drawback and 26 who did. The reasons for the nine responders changing the drawback procedure included: three being retrained by the medical team; two being told by their medical team to change but not receiving detailed retraining; two changing the technique without the medical team knowing (reason not stated); one having to remove blood clots; and one commencing using a line lock.
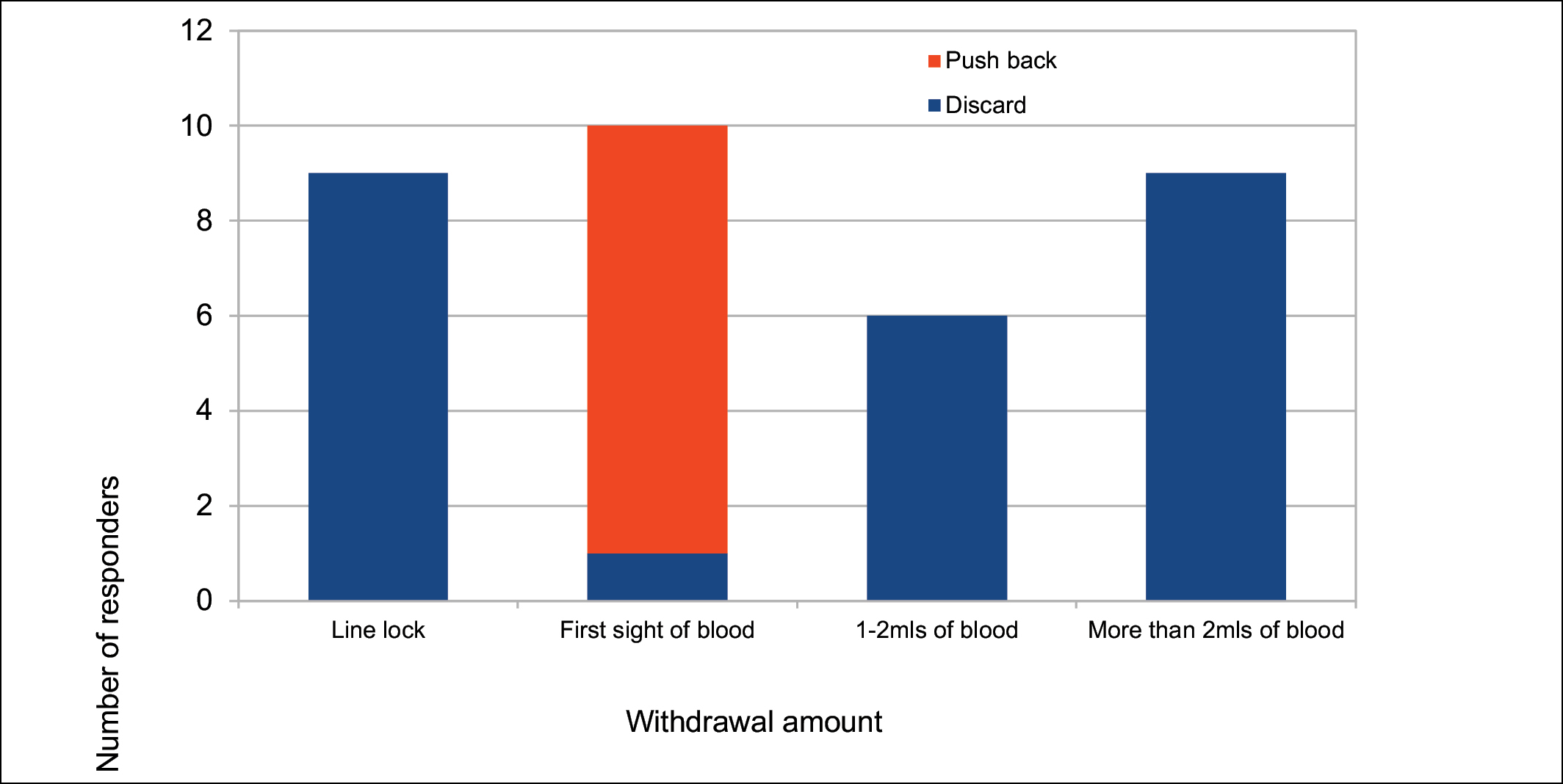
Figure 3. Withdrawal versus push back or discard.
Of the nine (eight adults, one child) responders who withdrew more than 2mL, five (four adults, one child) had received initial training prior to 2014. Further, of the nine responders, five had received some form of retraining and seven used the same drawback procedure as taught before initial discharge from hospital on PN.
DISCUSSION
With 40 responders, our survey had a 56% response rate of active HPN users represented in PNDU membership. As PNDU HPN users/carers comprise active HPN users – or their carers – of all ages in every Australian state and both New Zealand’s north and south islands, the study sample was geographically representative and a significant 14.2% of the estimated 282 HPN users across Australia and New Zealand.
HPN is a life-saving, yet complex, therapy2 that some users require for many years, and others even for the rest of their lives2,3. Therefore, it is vital that patients are trained in competent management of HPN, including the connecting and disconnecting procedures and care of the CVAD, in order to prevent complications2,23.
Surprisingly, a quarter of survey participants were not given written instructions on connection/disconnection procedures before initial hospital discharge on HPN. Considering the multiple steps involved in HPN procedures, a set of written step-by-step instructions might be expected to aid retention of procedures and be helpful as a reference for the HPN user or carer, especially in the early weeks after discharge from hospital. This is supported by both ESPEN’s 2016 guidelines2 and a retrospective study12, which recommend that patient training for HPN includes written instructions.
As many patients remain on HPN long-term2,3, it is also reasonable to expect that some further training or repeat demonstration of competency by the HPN user would reinforce good practice, and that the HPN user would benefit from being updated in the latest evidence-based or best practice procedures as part of that retraining. However, retraining is not addressed in AuSPEN’s guidelines23, and only in the event of repeated CLABSI in ESPEN’s guidelines2. In our study, 42% of participants had not received retraining, even though just over half of these had received their initial training three or more years earlier. Further, most of those who were retrained reported that the retraining was prompted by a specific event, commonly a suspected or confirmed CLABSI, in accordance with the ESPEN guidelines2, or a change in an ancillary item.
By extension, the secondary findings of two studies of HPN users27,28 challenge this omission of HPN user retraining from HPN guidelines and care. Konrad et al.27, investigating the education and treatment of dehydration in users of home parenteral support – both PN and intravenous fluids – concluded that there is an ongoing need for patient education no matter how long a patient has been receiving a specific therapy.
In addition, the study of long-term HPN users by Smith et al.28 to evaluate a specific mode of patient education demonstrated that adding this specific education mode to experienced HPN patients’ standard care education was associated with reduced CLABSI and rehospitalisations due to infection.
Furthermore, two studies of other patient cohorts required to perform medical procedures at home also showed greater adherence and better health outcomes following patient retraining25,26. First, a study of diabetes mellitus patients concluded that retraining in insulin injection technique led to glycaemic control improvement, and the study therefore called for greater focus on retraining of home patients25. Second, an investigation of cystic fibrosis patient retraining in airway clearance techniques documented not only lung function improvement outcomes but also sustained improvement through continued use of the retraining program26.
With progress in research and the increase and evolution of CVAD care products, regular retraining of HPN users also could ensure that the HPN patient cohort remains updated in the latest evidence-based or agreed best practice and protocols in HPN CVAD care. Acknowledging the limited evidence in HPN CVAD care24, a look at similar protocols in the in-hospital setting illustrates protocol change over time: pulsatile flushing technique as opposed to continuous flush technique29–31; scrubbing time of the needleless connector – 5, 15 or 30 seconds32–34; frequency of needleless connector change – 24, 48, 96 hours or once weekly35–37; or back and forth friction method as opposed to concentric circle method for skin cleaning when applying or changing a dressing38,39. As good healthcare practice involves updating clinicians in protocol and policy changes for best outcomes, it is reasonable to expect similar updating of HPN users in HPN CVAD protocols.
We therefore recommend investigation into both the most beneficial frequency and form of retraining and as well as who is best suited to conduct retraining, with a view to regular retraining of HPN users being included in an HPN model of care. In order that HPN users receive maximum benefit from regular retraining, we recommend it include HPN users demonstrating continued competence in CVAD use and care as well as updating HPN users in any new evidence-based or agreed best practice protocols.
Regarding the specific step of the PN connection procedure we surveyed – withdrawing back into the syringe – there was notable variation amongst responders. Most survey participants withdrew back into the syringe before connecting to PN. Nineteen of these withdrew back in accordance with the expert opinion of AVATAR (personal communication, 2018), that is, to draw back only until the first sight of blood in order to check catheter patency and/or removal of a line lock. Of note, a further nine responders withdrew more than 2mL of blood and seven of these had not changed their withdrawing procedure since initial hospital discharge on HPN. It would be interesting to know why these responders were instructed to withdraw this volume and whether it was due to a valid clinical reason, since it is likely that the volume of CVAD and needleless connector combined is less than 2mL40. It would also be interesting to know if this volume of blood withdrawal occurred daily and if it impacted negatively on the iron levels of the HPN users, especially the child users.
In light of the long-term and possibly indefinite nature of HPN for HPN users2,3, more research and resulting evidence-based protocols on all steps required for HPN, including this small but necessary step, would therefore be welcome. Moreover, we recommend development of evidence-based – or, where unavailable, agreed best practice – guidelines of all steps involved in HPN CVAD care for use by all Australian and New Zealand HPN hospitals and HPN users and carers.
Limitations
While 14.2% of the estimated 282 HPN users in Australia and New Zealand is significant representation, our study sample was still small so the results cannot be generalised to all HPN users. We also only surveyed HPN users who are PNDU members, resulting in possible selection bias. Limiting participation to eligible PNDU members may have selected for specific characteristics of people likely to join consumer groups and therefore possibly not representative of all HPN users. Further, the survey relied on patient recall and, although we attempted to define the term ‘retraining’, interpretation may have varied amongst the responders.
It was recognised on analysis of the responses that the year ranges offered as answer options to the questions of age and the length of time on HPN were overlapping, creating possible ambiguity. As a result, we could only definitively state the number of HPN users younger than 18 (child) and those 18 or over (adult), and therefore only reported adults and children rather than different age categories. Also, we could only definitively state the number on HPN less than two years and the number for two years or more. However, we were able to convey some patients’ long-time HPN use by stating the range since their first HPN training. Consequently, alongside specific data on gender, geography, social environment and underlying disease, which were not sought, the survey also lacks specific data on the age and duration of HPN.
This lack of clear data on the duration of HPN impacted on our ability to investigate any correlation between the length of HPN use, retraining or lack thereof, and the use – or not – of latest recommended protocols when looking at one small step of the PN connecting-up process – withdrawing back into a syringe. This component of the survey investigation was also impacted by the absence of evidence-based protocols for withdrawing back into the syringe, and the resulting question of the value of expert opinion versus evidence-based protocols.
DISCLOSURE STATEMENT
There are no conflicts of interest nor financial support for the study to report.
ACKNOWLEDGEMENTS
PNDU wishes to thank the following people. Sharyn Ingarfield performed the data analysis and wrote the initial draft of the report. Tricia Kleidon (Nurse Practitioner, Paediatric Vascular Access, Queensland Children’s Hospital, research fellow with Griffith University, and paediatric chapter lead for AVATAR) and Nicole Gavin (Clinical Nurse, Haematology and Bone Marrow Transplant, Royal Brisbane and Women’s Hospital, PhD student with NHMRC Centre for Research Excellence in Nursing, Griffith University) provided expert opinion on drawing back protocol. Gillian Ray-Barruel (Senior Research Fellow AVATAR) and Emily Larsen (Senior Research Assistant, Griffith University – School of Nursing and Midwifery) provided feedback on the survey questions and analysis. Thank you also to the members of PNDU who participated in the survey.
APPENDIX A – SURVEY QUESTIONS
Q1. Are you currently on Home Parenteral Nutrition (HPN)?
Yes
No
Q2. How old are you (at your last birthday)?
0–7 years
7–12 years
12–17 years
18 years and over
Q3. How long have you been on HPN, i.e. living at home on Parenteral Nutrition?
Less than 2 years
Over 2 years but less than 10 years
Over 10 years but less than 20 years
Over 20 years
Q4. In what year was your initial training to go home on Parenteral Nutrition? (enter a 4-digit year, for example, 2010)
Q5. With your initial training in connecting/disconnecting techniques before going home, were you given any written procedures and/or written advice to follow once at home?
Yes
No
Can’t remember
Q6. Since your initial training in connecting/disconnecting technique before going home on HPN, have you ever had any further training or updating by your medical care team? (tick as many as apply)
Yes, I’ve been given additional detailed oral instructions on all or a particular technique in connecting/disconnecting to PN; and/or
Yes, I’ve been given additional written instructions on all or a particular technique in connecting/disconnecting to PN; and/or
Yes, I’ve been given an additional demonstration on all or a particular technique in connecting/disconnecting to PN; and/or
Yes, I’ve been required to again demonstrate my competence in performing all or a particular technique in connecting/disconnecting to PN?
No
Can’t remember
Q7. How many times have you had further training or updating since first starting on HPN?
Once or twice
Regularly every year
Regularly every 2 years
Other (please specify)
Q8. In what year(s) did this further training or updating take place? (enter 4-digit year(s), for example, 2012 (and 2016))
Q9. Was any of your further training or updating undertaken because of a specific event, e.g. suspected or confirmed central line-associated bloodstream infection (CLABSI), change of ancillary items used, restarting HPN after a period off, or other medical problem?
Yes
No
Q10. What was the specific event(s) which led to you receiving further training or updating? (tick as many as apply)
Suspected or confirmed CLABSI
Change of ancillary item(s) used
Restarting HPN after a period off
Other medical problem
Can’t remember
Other reason altogether (please specify)
Q11. How many times have you had further training or updating because of a specific event(s)?
Once
Twice
Three times
Four times or more
Q12. During retraining, have you ever been taught new or updated procedures or techniques in connecting/disconnecting and CVAD care?
Yes
No
Can’t remember
Q13. What was/were the new or updated procedures or technique(s) you were taught during this retraining (short description, e.g. a new way of cleaning the hub, or flushing the line with 20mLs saline rather than 10mLs)?
Q14. Do you ever draw back into a syringe before connecting the CVAD to the administration/giving set of a bag of PN?
Yes
No
Q15. How much do you usually draw back?
Just enough to withdraw the line ‘lock’
Only until the first sight of a flash of blood in the CVAD/connector, i.e. to ensure the line is clear. I’m not concerned about withdrawing line ‘lock’
1–2mLs of blood
More than 2mLs of blood
Q16. What do you do with the blood you have withdrawn from the CVAD?
Discard it
Push it back in to the central line
Q17. Is how you carry out this drawback procedure (or not drawback at all) the same as you were taught by your hospital when you first went home on HPN?
Yes
No
Q18. Why has your technique for this procedure changed?
My medical care team retrained me in this technique
Someone in my medical care team told me to change it, but I did not receive formal retraining (i.e. detailed oral instructions; written instructions; a demonstration) nor was I required to demonstrate it myself
I changed my technique without my medical care team knowing
Other (please specify)
Q19. Thank you from the PNDU team for completing this survey! Please provide any other comments below in respect of retraining of connecting/disconnecting procedures.
Author(s)
*Karen Winterbourn; Chris Walker; Miranda Einstein; Gillian Anderson; Fay Boyd
*Corresponding author
Karen Winterbourn, Parenteral Nutrition Down Under Inc. (PNDU), 128 Rainbow Street, Randwick NSW 2031, Australia
Email contactpndu@gmail.com
Web www.pndu.org
References
- Pironi L, Arends J, Baxter J, Bozzetti F, Peláez RB, Cuerda C, et al. ESPEN endorsed recommendations. Definition and classification of intestinal failure in adults. Clin Nutr 2015;34(2):171–80.
- Pironi L, Arends J, Bozzetti F, Cuerda C, Gillanders L, Jeppesen PB, et al. ESPEN guidelines on chronic intestinal failure in adults. Clin Nutr 2016;35(2):247–307.
- Bielawska B, Allard JP. Parenteral nutrition and intestinal failure. Nutrition 2017;9(5):466.
- Dibb M, Teubner A, Theis V, Shaffer J, Lal S. Review article: the management of long-term parenteral nutrition. Alimen Pharm Ther 2013;37(6):587–603.
- Kelly DA. Intestinal failure-associated liver disease: what do we know today? Gastroenterol 2006;130(2):S70–77.
- Duerksen DR. Central venous thrombosis in patients receiving long-term parenteral nutrition. Appl Physiol Nutr Metab [Internet] 2008;33(1):32–38. doi:10.1139/H07–153
- Nielson XC, Chen M, Hellesøe AMB, Jeppesen PB, Gyldenlykke J, Tvede M, et al. Etiology and epidemiology of catheter related bloodstream infections in patients receiving home parenteral nutrition in a gastromedical center at a tertiary hospital in Denmark. Open Microbiol J 2012;6:98–101.
- Santarpia L, Buonomo A, Pagano MC, Alfonsi L, Foggia M, Mottola M, et al. Central venous catheter related bloodstream infections in adult patients on home parenteral nutrition: prevalence, predictive factors, therapeutic outcome. Clin Nutr 2016;35:1394–98.
- Durkin MJ, Dukes JL, Reeds DN, Mazuski JE, Camins BC. A descriptive study of the risk factors associated with catheter-related bloodstream infections in the home parenteral nutrition population. J Parenter Enteral Nutr 2016;40(7):1006–13.
- Gillanders L, Angstmann K, Ball P, Callaghan M, Thomson A, Wong T, et al. A prospective study of catheter-related complications in HPN patients. Clin Nutr 2012;31(1):30–34.
- Dibb MJ, Abraham A, Chadwick PR, Shaffer JL, Teubner A, Carlson JL, et al. Central venous catheter salvage in home parenteral nutrition catheter-related bloodstream infections: long-term safety and efficacy data. J Parenter Enteral Nutr 2016;40(5):699–704.
- Santarpia L, Pasanisi S, Alfonsi L, Violante G, Tiseo D, De Simone G, et al. Prevention and treatment of implanted central venous catheter (CVC)-related sepsis: a report after six years of home parenteral nutrition (HPN). Clin Nutr 2002;21(3):207–11.
- Wanten G, Calder PC, Forbes A. Managing adult patients who need home parenteral nutrition. BMJ 2011;342:d1447.
- Huisman-de Waal G, van Achterbeg T, Jansen J, Wanten G, Schoonhoven L. ‘High-tech’ home care: overview of professional care in patients on home parenteral nutrition and implications for nursing care. J Clin Nurs 2011;20(15–16):2125–34.
- Micic D, Semrad C, Chopra V. Choosing the right central venous catheter for parenteral nutrition. Am J Gastroenterol 2019;114(1):4–6.
- John BK, Khan MA, Speerhas R, Rhoda K, Hamilton C, DeChicco R, et al. Ethanol lock therapy in reducing catheter-related bloodstream infections in adult home parenteral nutrition patients: results of a retrospective study. J Parenter Enteral Nutr 2012;36(5):603–10.
- Chong CY, Ong RYL, Seah VXF, Tan NWH, Chan MY, Soh SY, et al. Taurolidine–citrate lock solution for the prevention of central line-associated bloodstream infection in paediatric haematology–oncology and gastrointestinal failure patients with high baseline central line-associated bloodstream infection rates. J Paediatr Child Health [Internet] 2019. doi: 10.1111/jpc.14506.
- Liu F, Hansra S, Crockford G, Köster W, Allan BJ, Blondeau JM, et al. Tetrasodium EDTA is effective at eradicating biofilms formed by clinically relevant microorganisms from patients’ central venous catheters. mSphere [Internet] 2018. doi: 10.1128/mSphere.00525–18
- Chaftari AM, Viola GM, Rosenblatt J, Hacham R, Raad I. Advances in the prevention and management of central line-associated bloodstream infections: the role of chelator-based catheter locks. Cambridge UP [Internet] 2019. doi: 10.1017/ice.2019.162
- Data from Baxter Healthcare, Fresenius Kabi Australia Pty Ltd and Biomed Limited, February 2019. Baxter Healthcare Pty Ltd operates in the HPN market in both Australia and New Zealand, Fresenius Kabi Australia Pty Ltd operates in the HPN market in Australia, and Biomed Limited operates in the HPN market in New Zealand.
- Mundi MS, Pattinson A, McMahon MT, Davidson J, Hurt RT. Prevalence of home parenteral and enteral nutrition in the United States. Nutr Clin Pract 2017 Dec;32:711–843.
- Howard L, Ashley C. Management of complications in patients receiving home parenteral nutrition. Gastroenterol 2003;124(6):1651–61.
- Gillanders L, Angstmann K, Ball P, Chapman-Kiddell C, Hardy G, Hope J, et al. AuSPEN clinical practice guideline for home parenteral nutrition patients in Australia and New Zealand. Nutrition 2008;24:998–1012.
- Kovacevich DS, Corrigan M, Ross VM, McKeever L, Hall AM, Braunschweig C. American Society for Parenteral and Enteral Nutrition guidelines for the selection and care of central venous access devices for adult home parenteral nutrition administration. J Parenter Enteral Nutr [Internet] 2019 Jan;43(1):15–31. doi:10.1002/jpen.1455.
- Nakatani Y, Matsumura M, Monden T, Aso Y, Nakamoto T. Improvement of glycemic control by re-education in insulin injection technique in patients with diabetes mellitus. Adv Ther 2013;30(10):897–906.
- Zanni RL, Sembrano EU, Du DT, Marra B, Bantang R. The impact of re-education of airway clearance techniques (REACT) on adherence and pulmonary function in patients with cystic fibrosis. BMJ Qual Saf 2014;23:i50–55.
- Konrad D, Roberts S, Corrigan ML, Hamilton C, Steiger E, Kirby DF. Treating dehydration at home avoids healthcare costs associated with emergency department visits and hospital readmissions for adult patients receiving home parenteral support. Nutr Clin Pract 2017;32(3):385–91.
- Smith CE, Curtas S, Kleinbeck SVM, Werkowitch M, Mosier M, Seidner DL, et al. Clinical trial of interactive and videotaped educational interventions reduce infection, reactive depression, and rehospitalizations for sepsis in patients on home parenteral nutrition. J Parenter Enteral Nutr 2003;27(2):137–45.
- Ferroni A, Gaudin F, Guiffant G, Flaud P, Durussel JJ, Descamps P, et al. Pulsative flushing as a strategy to prevent bacterial colonization of vascular access devices. Med Devices (Auckl) 2014;7:379–83.
- Guiffant G, Durussel JJ, Merckx J, Flaud P, Vigier JP, Mousset P. Flushing of intravascular access devices (IVAD) – efficacy of pulsed and continuous infusions. J Vasc Access 2012;13(1):75–78.
- Boord C. Pulsatile flushing: a review of the literature. J Infus Nurs 2019;42(1):37–43.
- Rupp ME, Yu S, Huerta T, Cavalieri RJ, Alter R, Fey PD et al. Adequate disinfection of a split system needleless intravascular connector with a 5-second alcohol scrub. Infect Control Hosp Epidemiol 2012;33(7):661–65.
- Björkman L, Ohlin A. Scrubbing the hub of intravenous catheters with an alcohol wipe for 15 sec reduced neonatal sepsis. Acta Paediatr 2015;104(3):232–36.
- Btaiche IF, Kovacevich DS, Khalidi N, Papke LF. The effects of needleless connectors on catheter-related bloodstream infections. Am J Infect Control 2011;39(4):277–83.
- Bliss DZ, Dysart M. Techniques and procedures: using needleless intravenous access devices for administering total parenteral nutrition (TPN): practice update. NCP [Internet] 1999 Dec;14(6):299–303. doi: 10.1177/088453369901400604.
- Do AN, Ray BJ, Banerjee SN, Illian AF, Barnett BJ, Pham MH, Hendricks KT, et al. Bloodstream infection associated with needleless device use and the importance of infection control practices in the home health care setting. J Infect Dis 1999;179(2):442–48.
- Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy standards of practice. J Infus Nurs Supplement 2016;39(1S):S69. Available from www.journalofinfusionnursing.com
- Stonecypher K. Going around in circles: is this the best practice for preparing the skin? Crit Care Nurs Q 2009;32(2):94–98.
- Hadaway L. Short peripheral intravenous catheters and infections. J Infus Nurs 2012;35(4):230–40.
- Goossens GA. Flushing and locking of venous catheters: available evidence and evidence deficit. Nurs Res Pract [Internet] 2015. doi: 10.1155/2015/985686
